Abstract
Lichen aureus is a rare type of chronic pigmented purpuric dermatosis. The eruptions consist of discrete or confluent golden to brownish lichenoid macules and papules, and are usually asymptomatic. Lichen aureus commonly occurs in young adults, but less frequently in children. We report the first case of multiple lichen aureus occurring in a Korean child.
Lichen aureus is a rare type of chronic pigmented purpuric dermatosis. It is usually characterized by a single localized golden macule on an extremity1. Five cases of lichen aureus have been reported in the Korean literature2-6. However, a childhood case has not been previously reported. We herein report the first case of multiple lichen aureus in an 8-year-old Korean child.
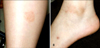
An 8-year-old Korean girl presented with a single asymptomatic round brownish patch on the right arm and two similar shaped patches on the left leg. The lesion on the arm first appeared one year previously, and the lesions on the leg started to appear three months ago. There was a history of a right tibial fracture four months ago, and no other preceding trauma around the skin lesions. Routine laboratory tests during hospitalization for treatment of the fracture showed slightly elevated liver enzymes (AST: 58 IU/L, normal 0~40 IU/L; ALT: 111 IU/L, normal 0~40 IU/L), which were thought to reflect a non-alcoholic steatohepatitis due to obesity. No other significant health problems or family history of similar disorders were noted. Physical examination revealed multiple round patches of yellow or brown on the right upper arm and left leg (Fig. 1). No evidence of other skin diseases was noted on complete examination of the skin.
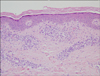
Histopathological examination of the left leg revealed a perivascular lymphocytic infiltration in the upper dermis with extravasation of red blood cells and mild exocytosis of lymphocytes in the epidermis (Fig. 2). Based on these clinical and histopathological features, the skin lesion was diagnosed as multiple lichen aureus.
The patient was treated with 0.1% methylprednisolone aceponate cream applied twice a day for four months. At the end of this time, the lesions were nearly completely resolved (Fig. 3).
Lichen aureus is an uncommon variant of pigmented purpuric dermatosis, which was first described by Marten7 in 1958. Most cases manifest as asymptomatic discrete or confluent golden to brownish lichenoid macules and papules that clinically resemble a bruise. The lesions usually persist unchanged for many years8,9. In a review of cases reported by Price et al.8, the average duration of lichen aureus is about 2.5 years (range, 1~10 years). Lichen aureus commonly occurs in young adults and the involved sites are most often on the lower legs.
Childhood lichen aureus has some distinctive characteristics. First, in general, it occurs less frequently than in adults10,11. Gelmetti et al.10 reported that only 17% of the total number of cases included children. Second, the disease in children is more self-limiting compared to the disease in adults10. Third, uncommon sites such as the trunk and arms are more frequently observed in children1,10. In children, Schamberg disease and lichen aureus are relatively common types of pigmented purpuric dermatosis; however, Majocchi's disease and eczematoid-like purpura of Doucas and Kapetanakis are very rare. To date, pigmented purpuric lichenoid dermatosis of Gougerot and Blum has not been reported in children.
The etiology of lichen aureus remains unknown but several mechanisms have been suggested including venous insufficiency12, infection13 and drugs14.
Histopathologically, lichen aureus differs from other purpuric pigmented dermatoses by variable exocytosis of lymphocytes, lichenoid infiltration of superficial dermis, and marked accumulation of hemosiderin-containing macrophages8. Many reports on the prognosis of lichen aureus have suggested that lichen aureus may potentially progress to mycosis fungoides with similar histologic findings and clonal populations of lymphocytes15. But a recent study shows that no progression to mycosis fungoides was observed in 23 patients with conventional lichen aureus16. Although a relationship between lichen aureus and mycosis fungoides is debatable, lichen aureus belongs to the expanding spectrum of clonal dermatoses17, and possible progression to mycosis fungoides cannot be ruled out. Therefore, patients with lichen aureus should have regular follow up and remain under close observation.
Lichen aureus is generally considered difficult to treat as topical corticosteroids are usually ineffective9,11. Recent case reports suggest several treatments for lichen aureus: psolaren-UVA therapy18, topical pimecrolimus19, and combination therapy with pentoxifylline and prostacyclin20 have elicited good patient responses.
Our patient had multiple lesions on the arm and leg, which was an uncommon presentation. Although the patient had trauma and underlying steatohepatitis, the correlation of these factors to the development of the lichen aureus is uncertain; indeed the first lichen aureus lesion developed before the trauma. Unlike previous cases, topical steroid treatment was effective in our patient.
To date, five cases of lichen aureus have been reported in the Korean literature2-6; however, none of the cases included a prepubertal child. In addition, we could find only two cases of Asian childhood lichen aureus in our review of the published English medical literature. Lichen aureus in children has a tendency to be overlooked because it is so rare and presents with variable clinical features. It can be confused with contact dermatitis, stasis dermatitis, purpura, and other types of pigmented purpuric dermatoses. Histopathological characteristics and their incidence can help to make the exact diagnosis. Therefore, lichen aureus should be considered in the differential diagnosis of skin lesions that appear to be a simple bruise in children and need to be differentiated.
Figures and Tables
Fig. 1
(A) A single round brownish patch on the left calf and (B) a similar patch at the left malleolar area.
References
1. Schroeder-Devere T. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Pigmented purpuric dermatoses. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;1633–1637.
2. Chun SI, Chung KY, Nam IW, Park HY. A case of lichen aureus. Korean J Dermatol. 1985. 23:795–798.
3. Kwon KS, Han EH, Chung TA, Lim MK, Park SK. A case of lichen aureus. Korean J Dermatol. 1994. 32:312–315.
4. Yoon SP, Lee IH, Lee SH, Kim BS, Lee JH, Lee SC. A case of bilateral lichen aureus with good response to PUVA therapy. Korean J Dermatol. 1999. 37:420–422.
5. Bahn JY, Kim YS, Kwon SJ, Yu HJ. A case of segmental lichen aureus. Korean J Dermatol. 1999. 37:798–800.
6. Oh TH, Lee JW, Lee SH, Lee WS. Multiple lichen aureus. Korean J Dermatol. 2004. 42:1600–1602.
7. Marten RH. Case for diagnosis. Trans St Johns Hosp Dermatolo Soc. 1958. 40:98.
8. Price ML, Jones EW, Calnan CD, MacDonald DM. Lichen aureus: a localized persistent form of pigmented purpuric dermatitis. Br J Dermatol. 1985. 112:307–314.

9. Graham RM, English JS, Emmerson RW. Lichen aureus--a study of twelve cases. Clin Exp Dermatol. 1984. 9:393–401.

11. Kahana M, Levy A, Schewach-Millet M, Trau H, Feinstein A. Lichen aureus occurring in childhood. Int J Dermatol. 1985. 24:666–667.

12. Reinhardt L, Wilkin JK, Tausend R. Vascular abnormalities in lichen aureus. J Am Acad Dermatol. 1983. 8:417–420.

13. Nishioka K, Katayama I, Masuzawa M, Yokozeki H, Nishiyama S. Drug-induced chronic pigmented purpura. J Dermatol. 1989. 16:220–222.

14. Yazdi AS, Mayser P, Sander CA. Lichen aureus with clonal T cells in a child possibly induced by regular consumption of an energy drink. J Cutan Pathol. 2008. 35:960–962.

15. Toro JR, Sander CA, LeBoit PE. Persistent pigmented purpuric dermatitis and mycosis fungoides: simulant, precursor, or both? A study by light microscopy and molecular methods. Am J Dermatopathol. 1997. 19:108–118.

16. Fink-Puches R, Wolf P, Kerl H, Cerroni L. Lichen aureus: clinicopathologic features, natural history, and relationship to mycosis fungoides. Arch Dermatol. 2008. 144:1169–1173.
17. Guitart J, Magro C. Cutaneous T-cell lymphoid dyscrasia: a unifying term for idiopathic chronic dermatoses with persistent T-cell clones. Arch Dermatol. 2007. 143:921–932.
18. Ling TC, Goulden V, Goodfield MJ. PUVA therapy in lichen aureus. J Am Acad Dermatol. 2001. 45:145–146.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download