Abstract
Graft versus host disease (GVHD) has traditionally been divided into acute GVHD and chronic GVHD based on the period it occurs after transplantation. Chronic cutaneous GVHD has traditionally been classified into the lichenoid and scleroderma-like forms. However, unusual clinical forms have been reported such as dermatomyositis, lupus erythematosus and exfoliative dermatitis. A 35-year-old woman presented with a 2 week history of a pruritic maculopapular rash on the whole body. The rash rapidly progressed to confluent erythematous scaly patches and plaques with micaceous scales and this finally led to a generalized exfoliative dermatitis in a 1 month period. Here we present an unusual case of chronic cutaneous GVHD with the clinical features of exfoliative dermatitis. The histopathologic examination demonstrated the lichenoid features of chronic cutaneous GVHD.
Graft versus host disease (GVHD) is a frequent complication that occurs in 23% to 80% of the patients who undergo allogenic bone marrow transplantation1. GVHD has traditionally been divided into acute GVHD and chronic GVHD based on the time period it occurs after transplantation2. Chronic cutaneous GVHD has traditionally been classified into the lichenoid and scleroderma-like forms3. As the incidence of GVHD has recently increased and new, less intensive preparative regimens have been developed, chronic cutaneous GVHD is now appearing in pleomorphic and unusual clinical forms such as dermatomyositis, lupus erythematosus and exfoliative dermatitis4-6. We report here on a patient who developed chronic cutaneous GVHD with the clinical features of exfoliative dermatitis.
A 35-year-old woman presented with a 4 day history of myalgia. The initial laboratory test showed a WBC of 79,390/mm3 and a PLT of 21,000/mm3. After bone marrow biopsy, she was diagnosed with acute myeloid leukemia in December 2006. She was treated with induction chemotherapy and achieved a complete response (CR) state. After consolidation chemotherapy, she underwent allogenic BMT. She received GVHD prophylaxis with cyclosporin and methotrexate. On the day 23 after transplantation, she developed acute cutaneous (demonstrated in a skin biopsy) and gut GVHD, which resolved completely after a short course of prednisone (Fig. 1, 2). The cyclosporin was gradually tapered until suspension on day 115 after transplantation, and then the patient developed oral mucositis and a pruritic measle-like papulosquamous rash on the whole body including the palms and soles.
There was no evidence of a leukemia relapse on the bone marrow biopsy. She was treated with a mild topical corticosteroid agent and oral agents (prednisone 10 mg daily and antihistamines), but she showed no response. Two weeks later, the rash had rapidly progressed to confluent erythematous scaly patches and plaques with micaceous scales and this finally led to a generalized exfoliative dermatitis during a 2 month period (Fig. 3). The laboratory tests showed high levels of AST 49 U/L and ALT 99 U/L. No serologic evidence of reactivation or recent infection by hepatitis viruses was found. The histopathological examination revealed hypergranulosis, acanthosis, mild spongiosis, many dyskeratotic cells of the epidermis and a mild perivascular inflammatory infiltrate that was mainly composed of lymphocytes in the papillary dermis (Fig. 4). These findings were consistent with the diagnosis of chronic cutaneous GVHD. With the help of topical agents (an emollient and a potent topical corticosteroid ointment) and immunosupressant agents (cyclosporine 200 mg and prednisone 20 mg daily), she finally showed clinical improvement.
The erythematous rash and fine scaling on our patient involved more than 90% of the body surface area and this was clinically consistent with the diagnosis of exfoliative dermatitis7. Exfoliative dermatitis may be caused by a variety of underlying dermatoses, drug reactions and malignancies such as lymphoma, leukemia and solid tumors7-9.
Acute cutaneous GVHD usually presents as a pruritic or burning erythematous eruption of the palms, soles, neck and trunk. More severe reactions may progress to exfoliative dermatitis or total epidermal sloughing that resembles toxic epidermal necrolysis2. Chronic cutaneous GVHD has traditionally been classified into the lichenoid and scleroderma-like forms3. However, the initial presentation is sometimes subtle and a variety of less common cutaneous manifestations may be prevalent such as marked xerosis, ichthyosis, morbilliform rash, psoriasiform plaques and exfoliative dermatitis10.
Creamer et al.6 anecdotally reported on cases of chronic cutaneous GVHD with the clinical features of exfoliative dermatitis. In their study, out of 254 patients who had undergone allogenic hematopoietic stem cell transplantations (HSCT), 10 patients developed exfoliative dermatitis. The histopathologic examination revealed the combined features of both eczema, as indicated by epidermal spongiosis, and GVHD, as indicated by satellite cell necrosis. Creamer et al.6 named this cutaneous manifestation as an eczematoid GVHD. In addition, Hymes et al.10 also suggested that exfoliative dermatitis is a clinical variant of chronic cutaneous GVHD. On the other hand, Cook-Norris and Weenig11 commented on the article of Creamer et al. that the eczematoid presentation may be more accurately classified as a variant of acute GVHD.
When acute cutaneous GVHD is progressing unfavorably, it can present as an exfoliative dermatitis or widespread epidermal necrolysis2. Hence, the possibility of late onset acute GVHD12, which develops during the period of chronic GVHD, must be considered in our case. However, our patient had classic exanthematous acute GVHD earlier, and this resolved completely after a short course of prednisone. On the day 115 after transplantation, she developed a measle-like papulosquamous rash that was different from the previous skin lesions and it was not easily controlled with administering systemic immunosuppressive therapy. The oral mucositis and the high levels of liver enzymes in our case may be suggestive of acute GVHD, but chronic GVHD is also accompanied by oral involvement in 90% of the cases and by extracutaneous involvement such as liver disease13. Moreover, histopathological examination showed hypergranulosis, acanthosis and mild spongiosis, which excluded the possible diagnosis of acute cutaneous GVHD. Therefore, we suggest that in our patient, the exfoliative dermatitis that was observed both clinically and histopathologically was expressed as a manifestation of chronic GVHD.
Figures and Tables
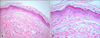
Fig. 2
The histological findings of the lesion showed basal vacuolization, necrotic epidermal cells and lymphocytes in the dermis, and this was all consistent with the diagnosis of acute cutaneous GVHD, grade II (H&E, A: ×100, B: ×200).
References
1. Andrews ML, Robertson I, Weedon D. Cutaneous manifestations of chronic graft-versus-host disease. Australas J Dermatol. 1997. 38:53–62.

2. Johnson ML, Farmer ER. Graft-versus-host reactions in dermatology. J Am Acad Dermatol. 1998. 38:369–392.

3. Hood AF, Soter NA, Rappeport J, Gigli I. Graft-versus-host reaction. Cutaneous manifestations following bone marrow transplantation. Arch Dermatol. 1977. 113:1087–1091.

4. Ollivier I, Wolkenstein P, Gherardi R, Wechsler J, Kuentz M, Cosnes A, et al. Dermatomyositis-like graft-versus-host disease. Br J Dermatol. 1998. 138:558–559.

5. Girardi M, Herreid P, Tigelaar RE. Specific suppression of lupus-like graft-versus-host disease using extracorporeal photochemical attenuation of effector lymphocytes. J Invest Dermatol. 1995. 104:177–182.

6. Creamer D, Martyn-Simmons CL, Osborne G, Kenyon M, Salisbury JR, Devereux S, et al. Eczematoid graft-vs-host disease: a novel form of chronic cutaneous graft-vs-host disease and its response to psoralen UV-A therapy. Arch Dermatol. 2007. 143:1157–1162.
7. Sehgal VN, Srivastava G, Sardana K. Erythroderma/ exfoliative dermatitis: a synopsis. Int J Dermatol. 2004. 43:39–47.
8. Jih MH, Kimyai-Asadi A, Freedberg IM. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Exfoliative dermatitis. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;225–232.
9. Rym BM, Mourad M, Bechir Z, Dalenda E, Faika C, Iadh AM, et al. Erythroderma in adults: a report of 80 cases. Int J Dermatol. 2005. 44:731–735.

10. Hymes SR, Turner ML, Champlin RE, Couriel DR. Cutaneous manifestations of chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2006. 12:1101–1113.

11. Cook-Norris RH, Weenig RH. Eczematoid graft-vs-host disease. Arch Dermatol. 2008. 144:1066. author reply 1066-1067.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download