Abstract
Sweet's syndrome is a reactive dermatosis characterized clinically by fever, leukocytosis, and multiple, erythematous, painful plaques. Histopathologic examination reveals a band-like dense dermal inflammatory infiltrate composed mainly of neutrophils with papillary dermal edema, and no features of vasculitis. We report a case of a 56-year-old female diagnosed with cervical cancer, who underwent surgery and concurrent chemoradiation therapy. Approximately 3 years after completing treatment, she presented with erythematous plaques, principally within the radiation field; the skin biopsy showed features consistent with Sweet's syndrome.
Sweet's syndrome can be subdivided into the following several broad groups: classic or idiopathic, malignancy-associated, and drug-induced1. A few cases of Sweet's syndrome in the literature have been associated with radiotherapy, but most of those patients had malignancies with signs of recurrence or developed in the skin lesion during the course of radiotherapy2-5. Only one case presented with skin lesions of Sweet's syndrome that corresponded with the irradiated area 1 year previously without recurrence of the cancer6. We report a case of localized Sweet's syndrome 3 years after chemoradiation therapy in a 56-year-old female who was diagnosed with cervical cancer with no evidence of relapse or distant metastasis of the cancer.
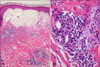
A 56-year-old woman was diagnosed with cervical carcinoma and clinically staged as Ib1 by the FIGO staging system. She underwent a radical hysterectomy with bilateral para-aortic lymph node dissection. Subsequently, she received 4 cycles of chemotherapy with cisplatin and 5-FU, and external beam radiation therapy targeting the right side of cervical area in 54 fractions. Approximately 3 years after completing treatment, she was referred for a dermatology consultation because of a 3-day history of asymptomatic erythematous plaques with overlying vesicles on the right side of the trunk. She complained of a 5-day history of fever and general weakness. Her body temperature was 38.1℃ and the blood pressure was 120/80 mmHg. Her medications at that time were lozartan and clinidipine for hypertension. The physical examination revealed several erythematous plaques with overlying vesicles, principally within the previously irradiated field that also extended over onto untreated skin of the left thigh (Fig. 1). The lesions were warm and painless. A hematologic evaluation demonstrated neutrophilic leukocytosis (white blood count, 11.4×103/µl with 88.1% neutrophils), increased erythrocyte sedimentation rate and elevated C-reactive protein level. The results of blood and wound cultures were negative. A skin biopsy showed dense infiltrates composed mostly of neutrophils with histiocytes and lymphocytes in the upper dermis. Edema of the papillary dermis and vesicle formation in the upper dermis were also seen and no evidence of true vasculitis was noticed (Fig. 2). Based on the physical examination and radiologic evaluation (chest x-ray and computed tomography of the abdomen and pelvis), there was no evidence of recurrence or metastasis of the cervical cancer. Based on the histopathologic findings and the clinical history, Sweet's syndrome was diagnosed. The lesions resolved spontaneously over the next 2 weeks.
A patient presenting with erythematous plaques and overlying vesicles in a localized area must be differentiated from allergic contact dermatitis, radiation dermatitis, radiation recall dermatitis, and herpes zoster. Asymptomatic lesions and no history of exposure to certain materials could exclude allergic contact dermatitis and herpes zoster. Radiation dermatitis is graded as acute, consequential, or chronic by the time of onset and the histopathologic features of each grade are specific7. The lesions of the case described herein developed 3 years after radiotherapy, but the histopathologic features did not correspond to chronic radiation dermatitis. Radiation recall dermatitis represents the development of an inflammatory reaction throughout a previously irradiated area, precipitated by the administration of certain drugs, such as cytotoxics or various stimuli, and usually occurs on first exposure to a particular recall triggering drug6,7. Our patient, however, had no inciting agent recalling a previous dermatitis and no history of Sweet's syndrome before the radiation therapy.
Acute febrile neutrophilic dermatosis was first described by Sweet in 1994 and the pathogenesis of Sweet's syndrome is not well understood. The disease is thought to be a hypersensitivity reaction, which can be triggered by multiple stimuli1. These stimuli may include malignancies, autoimmune diseases, infections, inflammatory bowel diseases, medications, or other miscellaneous conditions. Approximately 10% to 20% of cases of Sweet's syndrome occur in patients with underlying malignancies, especially acute myeloid leukemia1. In contrast with idiopathic Sweet's syndrome, patients with malignancyassociated Sweet's syndrome tend to develop more severe skin lesions with involvement of the mucous membranes or other extracutaneous sites, neutrophilia is typically absent, anemia and abnormal platelet counts are frequent, and there is a high rate of recurrence8,9.
There have been few reports of Sweet's syndrome associated with radiation for the treatment of malignancies (Table 1). In most patients, Sweet's syndrome developed in the irradiated field during the course of radiotherapy and spread to non-irradiated fields (cases 1, 2, 3, and 5)2-5. Therefore, we could not exclude malignancies and radiation as triggering factors in the development of skin lesions. But there has only been one case who presented with Sweet's syndrome corresponding with the irradiated area 1 year previously without recurrence of the cancer (case 4)6. The authors in that case thought that the localization of the irradiated lesion seemed to be explained well by the locus minoris resistentae ("a place of less resistance")6. It may be caused by compromised integrity and an impaired barrier function of the irradiated skin. Similarly, the skin lesions in our patient were localized to the previously irradiated area with no evidence for recurrence or metastasis. Hence, in the case presented herein, it is also unlikely that malignancy was the pathogenic factor in the localization of the lesion. We excluded the immediate effect of the radiation due to the 3-year interval after radiotherapy. We suggest that the radiotherapy induced cell damage and consequently a decreased threshold to the stimuli may have induced Sweet's syndrome to localize to the irradiated area. Further, the skin lesions in our patient extended to the untreated skin of the right lower extremity, which may be explained by a microcirculatory phenomenon4.
Some cases of Sweet's syndrome in the area of postmastectomy lymphedema have also been reported10, and most patients were treated by mastectomy with concurrent chemotherapy and radiotherapy. The pathophysiology of this lesion remains unknown, but inadequate lymphatic drainage may disrupt the regularity of cell trafficking. Several factors, such as type of cancer, mode of surgery, dissection of lymph nodes, and radiotherapy are involved in developing lymphedema after cancer treatment. Radiation-related lymphedema appears to be caused by lymph node sensitivity to radiation. Delayed soft tissue fibrosis after radiation is a main factor which decreases the filter function of lymph nodes and alters immune function. The incidence of lymphedema after radiotherapy is uncertain. In one study of gynecologic cancer, cervical cancer survivors had a 3.5-fold higher odds of developing lymphedema if they had radiotherapy than if they did not11. In our case, there was no evidence of lower extremity lymphedema, but lymphedema induced by radiation may be considered a triggering factor to develop localized Sweet's syndrome.
The gold standard of the treatment in Sweet's syndrome is systemic corticosteroids and the lesions of our patient resolved spontaneously over 2 weeks without any therapeutic intervention. Taken together, we report an unusual clinical feature of Sweet's syndrome localized to a previously irradiated area without evidence of recurrence or metastasis for malignancy.
Figures and Tables
Fig. 1
(A) Well-demarcated erythematous and edematous plaques on the right flank and lower abdomen. (B) Multiple overlying vesicles on the erythematous plaques.

References
1. Cohen PR, Kurzrock R. Sweet's syndrome: a neutrophilic dermatosis classically associated with acute onset and fever. Clin Dermatol. 2000. 18:265–282.

2. van der Meij EH, Epstein JB, Hay J, Ho V, Lerner K. Sweet's syndrome in a patient with oral cancer associated with radiotherapy. Eur J Cancer B Oral Oncol. 1996. 32B:133–136.

3. Pertusi RM, Forman MD, Brown AC. Sweet's syndrome after splenic irradiation for chronic myelogenous leukemia. J Am Osteopath Assoc. 1996. 96:366–367.

4. Dawe SA, Phillips R, Porter W, Francis NA, Bunker CB. Sweet's syndrome as a complication of radiotherapy for squamous carcinoma of the pharynx. Br J Dermatol. 2003. 149:884.

5. Che Y, Tanioka M, Matsumura Y, Miyachi Y. Splenic irradiation-induced Sweet's syndrome associated with preceding myelofibrosis. Clin Exp Dermatol. 2008. 33:200–201.

6. Vergara G, Vargas-Machuca I, Pastor MA, Farina MC, Martin L, Requena L. Localization of Sweet's syndrome in radiation-induced locus minoris resistentae. J Am Acad Dermatol. 2003. 49:907–909.

7. Hymes SR, Strom EA, Fife C. Radiation dermatitis: clinical presentation, pathophysiology, and treatment 2006. J Am Acad Dermatol. 2006. 54:28–46.

8. Cohen PR, Talpaz M, Kurzrock R. Malignancy-associated Sweet's syndrome: review of the world literature. J Clin Oncol. 1988. 6:1887–1897.

9. Cohen PR, Holder WR, Tucker SB, Kono S, Kurzrock R. Sweet syndrome in patients with solid tumors. Cancer. 1993. 72:2723–2731.

10. Garcia-Rio I, Perez-Gala S, Aragues M, Fernandez-Herrera J, Fraga J, Garcia-Diez A. Sweet's syndrome on the area of postmastectomy lymphoedema. J Eur Acad Dermatol Venereol. 2006. 20:401–405.

11. Beesley V, Janda M, Eakin E, Obermair A, Battistutta D. Lymphedema after gynecological cancer treatment: prevalence, correlates, and supportive care needs. Cancer. 2007. 109:2607–2614.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download