Abstract
Background
Rosacea is a common skin condition, but the currently available treatments are not satisfactory.
Objective
We wanted to assess the efficacy and safety of photopneumatic therapy (PPx), which delivers pneumatic energy and broadband light (400~1,200 nm), for the treatment of erythematotelangiectatic rosacea.
Methods
Twenty two patients with erythematotelangiectatic rosacea were treated 3~5 times with PPx. Three independent dermatologists evaluated the efficacy of PPx by comparing the photographs taken before and after treatment. Patient self-assessment was also done by interviews.
Results
The photographic assessment by the dermatologists of the improvement showed that >50% improvement occurred in 64% (14/22) of the patients. The specific categories of improvement were as follows: poor (<25% improvement), 1 patient; fair (25~50% improvement), 7 patients; good (50~75% improvement), 11 patients; and excellent (>75% improvement), 3 patients. Based on the patients' self-assessment, 20 patients (91%) acknowledged an improvement.
Rosacea is a chronic skin disease that primarily affects the central face1. There are four subtypes of rosacea: the erythematotelangiectatic, papulopustular, phymatous and ocular subtypes2,3. Although various treatment modalities, including systemic antibiotics and topical metronidazole or tretinoin, are used for the treatment of rosacea, such treatments are not usually successful for erythematotelangiectatic rosacea4. Vascular laser and intense pulsed light (IPL) may be useful for treating all the subtypes of rosacea, and especially erythematotelangiectatic rosacea5-7.
Photopneumatic therapy (PPx), which irradiates the skin on contact with broadband light and concurrent vacuum suction, has recently been shown to have results that are equivalent to those obtained with using conventional vascular laser and IPL for the treatment of vascular and pigmented lesions8. Therefore, PPx may be useful for the treatment of erythema and telangiectasias, which are the primary signs of rosacea. However, there have been no reported clinical studies with using PPx for the treatment of rosacea. We determined the efficacy and safety of using PPx for the treatment of the redness, the flushing and the telangiectasias associated with rosacea.
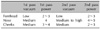
The clinical data was collected from 22 patients who were diagnosed with erythematotelangiectatic rosacea (8 men and 14 women) according to the US National Rosacea Society guidelines3 (Table 1). The patients had Fitzpatrick skin types II~IV, they ranged in age from 18 to 53 years, they had no significant concurrent illnesses and they gave their informed consent for PPx treatment. Those patients using other therapies for rosacea such as topical metronidazole, tretinoin, systemic antibiotics and other laser treatments were excluded. All the treatments were carried out with using a portable photopneumatic device (Aesthera Co., Pleasanton, CA, USA). Three to 5 treatments were performed at 2~4 week intervals without the use of topical anesthetic agents or cooling gels. Among the 22 patients, 3 patients were initially treated on only one side of the face (the face was divided into 2 areas) and the untreated area served as a control. When the patients noticed an improvement on the treated site after 2~3 sessions of treatment, they were then treated with PPx on the entire face. We usually used a large tip (15×30 mm) for the cheeks, a medium (10×20 mm) tip for the forehead and a small tip (6×12 mm) for the nose. The patients were treated with PPx at power settings of 2~4 (approximately equivalent to 4~10 J/cm2), depending on the subject's tolerance. The vacuum setting was set at low-to-high (levels 1~3) according to the treatment area, the skin type and the subject's tolerance. For vulnerable sites such as the forehead, the vacuum level was set on low (level 1) and the initial energy had a power setting of 3 or it was reduced to 2. For the other sites, the vacuum level was medium-to-high (levels 2~3) and the starting energy was a power setting of 4 or it was changed to 3 or 5. We usually treated the patients with 2 passes on each treatment session. The usual treatment settings are shown in Table 2.
At each visit, clinical photographs were taken with maintaining uniformity of the patient's position, the lighting and the camera set-up. At the end of the treatment sessions, the overall efficacy of PPx was objectively assessed from the clinical photographs by a panel that consisted of three dermatologists who reviewed the photographs independently according to the following categories: poor ≤25% improvement, fair=25% to 50% improvement, good=50% to 75% improvement and excellent ≥75% improvement. The patients were interviewed by the physicians for their self-assessment of the improvement of rosacea according to the following categories: aggravation, no change and improvement. The patients were also asked to note the presence of any other side effects or adverse events.
Review of the photographs before and after treatment revealed that 64% (14/22) of the patients had >50% improvement, as judged by three independent evaluating physicians. Among the 22 patients, 5% of the patients had poor (1% to 25%) improvement, 32% of the patients had fair (26% to 50%) improvement, 50% of the patients had good (51% to 75%) improvement and 14% of the patients had excellent (76% to 100%) improvement (Fig. 1). Three patients, who were initially treated on one side of the face (face-split), noticed a greater improvement on the treated site after 2~3 treatments than that on the untreated site. Subsequently, they were treated with PPx on the entire face and they also noticed an improvement on the subsequently-treated site. The clinical photographs of the improved patients are presented in Fig. 2, 3, 4. The subjective data was obtained by the patients' self-assessment of the improvement of their rosacea. Among the 22 patients, 20 patients (91%) noted an improvement and 2 patients claimed there was no change, but no patients experienced any aggravation after PPx treatment. Specifically, the patients noted an improvement in both their baseline erythema and tendency for flushing, and nearly all of the patients also noted improved skin texture, a brighter skin tone and reduced sebum secretion. Six patients with associated acne showed great improvement or nearly complete remission of the acne and there was no significant relapse during the treatment. The complications were limited to purpura that developed in 5 patients due to the pneumatic pressure, and the purpura resolved within 1 week (Fig. 5). The pain during treatment was mostly tolerable, so topical anesthesia was usually not necessary.
Vascular laser and intense pulsed light may be useful for treating all subtypes of rosacea, and especially erythematotelangiectatic rosacea5,6. A pulsed dye laser at 585 nm has been used to treat rosacea, and good-to-excellent improvement of the telangiectasia and erythema was noted following 1~3 sessions7. In addition, inflammatory lesions were also improved in 60% of these patients. However, with the pulsed dye laser, there is unsightly purpura that lasts 1~2 weeks, and sometimes crusting and scabbing can develop. Hyperpigmentation can also develop, which can take weeks or months to resolve9. IPL is also an effective means of treating erythematotelangiectatic rosacea with long-lasting results10-12. Its main advantage over traditional pulsed dye laser is the lack of purpura so that patients can return to work sooner.
PPx, which is the first and only therapy to effectively combine broadband light with pneumatic energy, has recently been introduced and it has been reported to be successful for the treatment of unwanted hair, photorejuvenation and acne7,13,14. PPx light from 400~1,200 nm with a peak absorption at 440~550 nm, including wavelengths in the blue light region, has been used to treat rosacea13.
PPx differs from other laser and light-based treatments in that it is highly efficient in delivering energy to the targeted treatment areas. Using a proprietary pneumatic (vacuum) hand piece, the treatment area is gently elevated and stretched to increase its translucence and this also brings the desired target closer to the surface of the skin and it also reduces the concentration of the competing normal epidermal constituents. When the light is emitted to the skin at the end of the pneumatic sequence, the elevated targets and the dispersed competing chromophores allow 4 to 5 times more photons to impact the melanin and hemoglobin with greatly reduced energies. As a result of its highly efficient delivery, PPx produces excellent clinical outcomes with no pain, extreme safety and no thermal compromise to the surrounding normal tissues13-15. Thus, patients undergoing PPx do not require pre-treatment with topical anesthetics or cooling gels, and this also reduces the treatment time.
In a recent study7, the results of the treatment of vascular and pigmented lesions with PPx were equivalent to the results obtained with conventional lasers and broadband IPL at 3 months, and the patients experienced no pain and the treatment time was reduced. In addition, all the patients who were treated with PPx had no adverse effects or complications. In our study, PPx showed a beneficial effect on the burning, flushing, erythema and overall discomfort of erythematotelangiectatic rosacea. Among 22 patients, 14 patients (64%) showed >50% improvement. Three patients, who were initially treated on only one side of the face (the face was divided into 2 areas), noticed a greater improvement on the treated site after 2~3 treatments than on the untreated site. Based on our results, we suggest that PPx is an efficient treatment option for erythematotelangiectatic rosacea. However, there have been no clinical studies comparing the efficacy between PPx and other lasers for the treatment of rosacea. Additional studies are needed that will focus on comparing the efficacy between other lasers and PPx. The complications of our patients were minimal, with only one incident of purpura due to pneumatic pressure and this resolved within 1 week. Purpura may develop if the setting of the pneumatic pressure is medium or high on vulnerable sites such as the periocular area, the forehead and the bridge of the nose. Therefore, it is recommended to reduce the pneumatic pressure to a low level when treating these areas.
PPx has also been shown to be effective in improving photodamaged skin, fine wrinkles and laxity7. A recent study16 showed increased synthesis of dermal collagen in the histologically-examined skin after treatment with pulsed dye laser (585 nm) and IPL (500~1,200 nm). This supports the role of PPx for dermal collagen remodeling and improving the skin texture because PPx and these lasers overlap in the wavelength range. The exact etiology of rosacea is unclear, but a main pathogenic factor of rosacea appears to be loose dermal connective tissue that allows for passive dilation of the vessels and so this manifests as erythema and telangiectasia, and the extravascular leakage of inflammatory mediators causes inflammatory papules and pustules1,6,17,18. Therefore, PPx can improve rosacea by effectively ablating abnormal vessels and it might also improve the dermal extracellular matrix abnormalities and elastotic degeneration by stimulating remodeling of the dermal collagen. This would likely improve the erythema and telangiectasias of the patients with rosacea, and it could possibly be followed by a reduction in the size and number of papules and pustules.
Moreover, PPx is the only laser treatment that's been approved by the Food & Drug Administration (FDA) for the treatment of the four different types of acne. The superior efficacy of PPx for the treatment of acne is probably due to the killing of P. acne by blue light, the reduced sebum secretion and extruding the plugged sebum and keratins out of the follicles13-15. Although the age distribution of rosacea showed a peak incidence in the fifth decade, rosacea often develops in the young age groups19-21. Therefore, patients with rosacea frequently complain of associated acne and greasiness that are due to excessive sebum secretion and dilated pores. According to our favorable results for the 6 rosacea patients with associated acne, PPx is, in our opinion, the convincing treatment of choice for the patients with both rosacea and acne.
In conclusion, our data suggests that PPx is a safe and effective option for the treatment of erythematotelangiectatic rosacea, and especially for those patients with associated acne. However, there remains a great need for additional clinical studies with using larger randomized methods. Moreover, another limitation of our study is that we obtained only the short-term results of PPx's efficacy and safety. Therefore, long-term studies are needed to determine the long-term results of using PPx for the treatment of erythematotelangiectatic rosacea.
Figures and Tables
Fig. 1
Percentage of the patients showing different degrees of improvement based on independent photographic evaluation.

Fig. 2
The clinical pictures of patient 2. (A) Before treatment, (B) 3 weeks after 2 sessions of treatment (right side only [the face was divided into 2 areas]) and (C) 3 months after 5 sessions of treatment to the entire face.

Fig. 3
The clinical pictures of patient 9. (A) Before treatment, (B) 3 weeks after 2 sessions of treatment (right side only [the face was divided into 2 areas]) and (C) 4 months after 5 sessions of treatment to the entire face.

Fig. 4
The clinical pictures of patient 15. (A) Before treatment, (B) 1 month after 1 session of treatment and (C) 1 month after 2 sessions of treatment to the perinasal area.

References
1. Plewig G, Jansen T. Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Rosacea. Fitzpatrick's dermatology in general medicine. 2003. 6th ed. New York: McGraw-Hill;688–696.
2. Wilkin J, Dahl M, Detmar M, Drake L, Feinstein A, Odom R, et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol. 2002. 46:584–587.

3. Wilkin J, Dahl M, Detmar M, Drake L, Liang MH, Odom R, et al. Standard grading system for rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol. 2004. 50:907–912.

6. Papageorgiou P, Clayton W, Norwood S, Chopra S, Rustin M. Treatment of rosacea with intense pulsed light: significant improvement and long-lasting results. Br J Dermatol. 2008. 159:628–632.

7. Lowe NJ, Behr KL, Fitzpatrick R, Goldman M, Ruiz-Esparza J. Flash lamp pumped dye laser for rosacea-associated telangiectasia and erythema. J Dermatol Surg Oncol. 1991. 17:522–525.
8. Narurkar VA. Noble photopneumatic therapy delivers high-efficiency photons to dermal targets. Cosmet Dermatol. 2005. 18:115–120.
9. West TB, Alster TS. Comparison of the long-pulse dye (590-595 nm) and KTP (532 nm) lasers in the treatment of facial and leg telangiectasias. Dermatol Surg. 1998. 24:221–226.

10. Schroeter CA, Haaf-von Below S, Neumann HA. Effective treatment of rosacea using intense pulsed light systems. Dermatol Surg. 2005. 31:1285–1289.

11. Mark KA, Sparacio RM, Voigt A, Marenus K, Sarnoff DS. Objective and quantitative improvement of rosacea-associated erythema after intense pulsed light treatment. Dermatol Surg. 2003. 29:600–604.

12. Taub AF. Treatment of rosacea with intense pulsed light. J Drugs Dermatol. 2003. 2:254–259.
13. Omi T, Munavalli GS, Kawana S, Sato S. Ultrastructural evidence for thermal injury to pilosebaceous units during the treatment of acne using photopneumatic (PPX) therapy. J Cosmet Laser Ther. 2008. 10:7–11.

14. Gold MH, Biron J. Efficacy of a novel combination of pneumatic energy and broadband light for the treatment of acne. J Drugs Dermatol. 2008. 7:639–642.
15. Shamban AT, Enokibori M, Narurkar V, Wilson D. Photopneumatic technology for the treatment of acne vulgaris. J Drugs Dermatol. 2008. 7:139–145.
16. Zelickson B, Kist D. Effect of pulsed dye laser and intense pulsed light source on the dermal extracellular matrix remodeling. Lasers Surg Med. 2000. 12:17.
17. Neumann E, Frithz A. Capillaropathy and capillaroneogenesis in the pathogenesis of rosacea. Int J Dermatol. 1998. 37:263–266.

18. Gupta AK, Chaudhry MM. Rosacea and its management: an overview. J Eur Acad Dermatol Venereol. 2005. 19:273–285.

19. Shin JB, Kim IH. A clinical study of 90 patients with rosacea. Korean J Dermatol. 2007. 45:1161–1169.
20. Lee SY, Choi JH, Sung KJ, Moon KC, Koh JK. A clinical study of 112 patients with rosacea. Korean J Dermatol. 2001. 39:636–642.
21. Kim TH, Hwang SM, Lee WS, Ahn SK, Choi EH. A clinical study of rosacea. Korean J Dermatol. 2000. 38:583–588.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download