Abstract
Background
Although rosacea is a chronic cutaneous inflammatory disorder that's commonly seen in adults, the etiology and pathogenesis of the illness remain unclear. A well established diagnostic classification and grading system may play a critical role in performing research and it would serve as a diagnostic reference in the clinical field.
Objective
We sought to classify the patients with the new standard classification and grading system and we wanted determine the peculiar features and relationships of each subtype. We also analyzed the relationships between the degree of sun exposure and each subtype.
Methods
We reviewed the medical records and clinical photos of 168 patients who were diagnosed with rosacea from 2002 to 2007 at our hospital. The standard classification and grading system suggested by the National Rosacea Society (NRS) Expert Committee was adopted to evaluate each patient's subtype and the severity.
Results
The male:female ratio was 1:2.29. The mean age at the time of diagnosis was 47.8 years. The mean duration of disease was 3.5 years. Sun exposure and hot baths/exercise were the two most common precipitating factors, while the majority of patients did not have any specific factor that relieved their symptoms. According to the NRS classification and grading system, the patients were classified into four subtypes. One hundred sixty two (96.4%) patients were diagnosed with the erythematotelangiectatic subtype irrespective of severity. Eighty five (50.6%) patients had the papulopustular subtype and 24 (14.3%) patients had ocular rosacea. Eight (4.8%) patients displayed mild phymatous change. The degree of sun exposure had significant correlation with the development and severity of the erythematotelangiectatic subtype (p<0.05), while it had no correlation with the papulopustular, ocular and phymatous subtypes.
Conclusion
Although the erythematotelangiectatic subtype was the most common subtype of rosacea, many patients also had other subtypes of rosacea simultaneously. Based on our results, we proved that ocular rosacea is an extension of the clinical spectrum of erythematotelangiectatic rosacea. In addition, the results of our study particularly suggest that sun exposure has a different influence on each subtype of rosacea.
Rosacea is a chronic inflammatory disease of skin and it is commonly observed in middle-aged women1. It shows various manifestations such as intermittent or persistent erythema, telangiectasia, papules and pustules, ocular findings with or without cutaneous symptoms, and phymatous change. Although the pathogenesis of rosacea remains unclear, it has been suggested that recurrent dilatation of cutaneous vessels followed by impairment of their regulatory function, invasion of inflammatory cells, changes in the perivascular tissue and infestation by microorganisms may play critical roles1-3. Many trigger or aggravating factors have also been reported. It has generally been accepted that sun exposure may play a role in developing or aggravating rosacea, and especially in fair skinned people1,4-6. However, their relationships with the development or the progression of rosacea have not yet been evaluated in an Asian population.
There have been several attempts by western researchers and clinicians to establish a proper classification and severity grading system for rosacea; however, it was not easy to set up a unified standard classification and grading system due to this disease's variable clinical manifestations and the lack of definite diagnostic methods2,7,8. Therefore, the National Rosacea Society (NRS) Expert Committee suggested a new classification and severity grading system in 2002 and 2004, respectively9,10. To the best of our knowledge, there has been no prior clinical study in the medical English literature with using the new NRS classification and grading system for rosacea in any type of population. We surveyed the clinical features in Korean patients with rosacea and who visited our department during the recent 5 years and we classified them by the new classification and grading system. We also statistically determined if there was any correlation between each subtype or between the clinical features and the subtypes, and also between the degree of sun exposure and each subtype.
One hundred sixty eight patients who were diagnosed with rosacea from March 2002 through February 2007 were enrolled in this study. Each patient's Fitzpatrick's skin type was determined by their experience of skin reactions to sun exposure and the clinician's inspection. The patient's medical records and clinical photos were reviewed. Age, gender, the duration of symptoms, the past history, the triggering or aggravating factors, the relieving factors, the area of living and the degree of daily sun exposure were analyzed. The primary features of rosacea (flushing, nontransient erythema, papules, pustules and telangiectasia), as suggested by the NRS, were adopted as a diagnostic tool. The patients with at least one of the primary features were considered as having rosacea. The secondary features such as burning or stinging, a dry appearance, edema, ocular manifestations, a peripheral location and phymatous changes were also checked. The four subtypes of rosacea were classified by a physician's global assessment; the erythematotelangiectatic, papulopustular, phymatous and ocular types. The new classification system defines the potential overlap of subtypes; therefore, a patient may have two or more subtypes. The characteristics of each subtype are described in Table 1.
With using the standard grading system suggested by the NRS in 2004, the severity of the primary and secondary features and each subtype were graded as absent, mild, moderate or severe (0~3). The Berg-Liden classification system6 was used for the erythematotelangiectatic subtype: erythema on the nose and perinasal area or cheeks only was regarded as mild; erythema with or without telangiectasia on both the nose and cheeks with a relatively light hue was regarded as moderate; erythema with or without telangiectasia on almost the entire face or a deeper hue was regarded as severe. The extent or number of lesions and the confluence and grade of the inflammation were all considered in grading the papulopustular subtype. The ocular subtype was clinically graded by the severity of the subjective symptoms or the clinical findings. Finally, the phymatous subtype was clinically graded by the extent and severity of the thickening, irregularity and nodularity.
We statistically examined if there was any correlation between each subtype and the incidence or severity. Moreover, we found significantly frequent clinical features in the individual subtypes. Finally, the relationship between the degree of sun exposure and each subtype was analyzed.
Pearson's chi-square tests and linear by linear association analysis were conducted to evaluate the correlation between the severity of each subtype and the degree of sun exposure. The correlation between each subtype and the correlation between the clinical features and the subtypes were analyzed. A p-value of <0.05 was considered statistically significant.
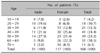
Of the 168 rosacea patients, the male:female ratio was 1:2.29 (51 men and 117 women). There was a female predominance in all age groups except for the 2nd and 3rd decades. Ninety five (56.5%) patients had Fitzpatrick's skin type III, 55 (32.7%) patients had type IV, 12 (7.1%) had type V and 6 (3.6%) had type II. The peak decades for the age at presentation were the 4th (41 patients, 24.4%) and 5th decades (39 patients, 23.2%) (Table 2) and the mean age of the patients was 47.8±14.9 years (42.8±15.3 for the men and 50.0±14.2 for the women). The patients had their skin complaints for an average of 3.5 years (3.2 years for the men and 3.6 years for the women). One hundred twenty two patients (72.6%) were from urban areas and 46 (27.4%) patients were from rural areas.
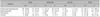
Sun exposure (42 patients, 25%) and hot bath/exercise (41 patients, 24.4%) were the two most common precipitating factors. However, 37 (22%) patients had no precipitating or aggravating factor (Table 3). Alcohol ingestion was related as a precipitating factor for the men rather than for the women (p<0.05), while sun light-induced aggravation was more commonly documented for the women (p<0.05).
Eighteen (10.6%) patients experienced improvement of symptoms by resting and going to an environment with a cooler temperature. However, the majority of patients (125, 74.4%) did not find any particular relieving factors (Table 3).
Among the four primary features, persistent erythema was the most common feature (143 patients, 85.1%). Transient erythema, telangiectasia and papulopustules were observed in 121 (72%), 103 (61.3%) and 92 (54.8%) patients, respectively (Table 4).
The most common secondary feature was burning or stinging (117 patients, 69.6%). Sixty six (39.3%) and 21 (12.5%) patients exhibited a dry appearance and ocular manifestations, respectively. Edema, a peripheral location, plaques and phymatous change were observed or documented in 13 (7.8%), 10 (6%), 7 (4.2%) and 7 (4.2%) patients, respectively (Table 4).
According to the physicians' rating the patients by subtype, each patient was classified and graded for their severity. One hundred sixty two (96.4%) and 85 (50.6%) patients were diagnosed with erythematotelangiectatic rosacea and papulopustular rosacea, respectively. There were eight (4.8%) and 24 (14.3%) cases of the phymatous and ocular subtypes, respectively.
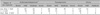
For the erythematotelangiectatic subtype, 85 (50.6%) patients were graded as mild, 73 (43.5%) were graded as moderate and 4 (2.4%) were graded as severe. For the papulopustular type, 54 (32.1%) patients were graded as mild, 24 (14.3%) were graded as moderate and 7 (4.2%) were graded as severe. Twenty one (12.5%) patients out of the 24 patients with the ocular subtype were graded as mild, and the remaining three were graded as moderate. All the patients with the phymatous subtype had hypertrophy and nodularity to a mild degree (Table 5). The grade of the erythematotelangiectatic subtype increased with age (p=0.001), while that of the other subtypes did not.
There was significant correlation between the severity of erythematotelangiectatic rosacea and the development of ocular rosacea (p=0.019). However, no correlation was found between the severity of erythematotelangiectatic rosacea and the development of other subtypes. Also, there was no correlation between the severity of the papulopustular subtype and the development of the other subtypes.
For the secondary features, only burning/stinging had significant correlation with erythematotelangiectatic rosacea (p=0.013), while plaque and edema had correlation with papulopustular rosacea (p=0.045, p=0.012). The development of ocular rosacea was significantly increased with the increased grade of burning/stinging and ocular manifestations (p=0.008, p<0.001).
The objects were asked about their daily sun exposure time and then they were classified into three groups (less than 1 hour, 1~3 hours, more than 3 hours). The severity of the erythematotelangiectatic subtype was correlated with the degree of sun exposure (p<0.05). In contrast, no such correlation was observed for the papulopustular, ocular and phymatous subtypes (Table 6).
In this study, we classified and graded Korean patients with rosacea by using the new NRS classification and grading system. We also derived the characteristics of each subtype and the relationships between them. Interestingly, we found that there was a close relationship between sun exposure and the erythematotelangiectatic subtype of rosacea.
The concept of rosacea has recently been changed so that it allows the overlap of variable manifestations with different severity. The new classification and severity grading system suggested by the NRS strongly reflects this tendency. Therefore, one patient may have more that one overlapping subtype simultaneously with different severity grades. The new system seems more proper and convenient when evaluating the patients with rosacea. It would also be helpful for treating rosacea patients because of the system's more realistic understanding of this disease.
The existence of a wide clinical spectrum and various subtypes causes clinicians to assume that many factors appear to contribute differently to the development or aggravation of rosacea. Impairment of vascular reactivity and homeostasis, changes or degenerations of dermal structures, inflammatory processes, pilosebaceous unit abnormalities and infestations of microorganisms such as Demodex and Helicobacter pyroli may directly or indirectly influence the development of rosacea2,3,11-14.
The incidence of rosacea varies among different studies. Although rosacea affects all races, it has generally been accepted that the disease more commonly develops in Caucasians and fair-skinned populations1,4,5,7. However, our study suggests that chronic sun exposure can also be a causative factor for rosacea in an Asian population.
The male:female ratio of 1:2.29 in our study was not much different from that of the other studies. The mean age of the patients was 47.8 years and the peak age of incidence was in the 40s to 60s, which was slightly older than what has been previously reported. As peoples' life expectancy is prolonged, the proportion of elderly patients with rosacea in our clinic may have increased. Another possibility may be the effect of long-term sun damage in elderly persons.
Though there are many factors in the development or aggravation of rosacea, sun exposure and hot bath/exercise were revealed in this study to be the two most common precipitating factors, followed by alcohol ingestion and a warm environment. Sun damage has been accepted to be a critical factor in the development of rosacea since the distribution of erythema is most prominent on the facial convexities5. In addition, solar elastosis is a frequent histologic finding in the lesions of rosacea12. In contrast, some studies have demonstrated that the incidence of rosacea was not higher for the groups of patients with chronic sun exposure. Some studies have also focused on the fact that sun exposure to non-facial areas did not induce the disease10,15,16. These findings could support the hypothesis that sun exposure may not be an independent factor for the development of this disease. From the assumption that chronic sun exposure may induce or aggravate rosacea, we analyzed the correlation between the degree of sun exposure and the development of each subtype. It's interesting that the severity of the erythematotelangiectatic subtype had correlation with the degree of sun exposure. However, such a relationship was not found for the papulopustular, ocular and phymatous subtypes. Altogether, our result suggests that sun exposure has a different influence on each subtype.
Hot baths, exercise and alcohol ingestion can induce rosacea, as these things all dilate cutaneous vessels due to an increased core temperature. This phenomenon is especially seen in the facial area, where the vasculature is prominent as well as having a shallow distribution in relation to the skin surface17,18.
The majority of our patients had the erythematotelangiectatic subtype, which has been considered to be an initial phase of rosacea. In our study, we found that grade of this subtype increased with the duration of disease. It was notable that the grade of erythematotelangiectatic rosacea had correlation with the development of ocular rosacea, while no clinical correlation was found between the grade of erythematotelangiectatic rosacea and the papulopustular and phymatous subtypes of rosacea. This result highlights the fact that ocular rosacea is an extension of the clinical spectrum of erythematotelangiectatic rosacea, while the other subtypes are not related to ocular rosacea.
About half of our patients had papulopustular rosacea. This result was relatively higher than the general consensus from other studies. Since the NRS system permits overlapping of the subtypes, clinicians do not need to select one particular subtype. Accordingly, this change in classification system is postulated as the cause for a higher rate of the incidence of the papulopustular subtype. In addition, our study revealed several characteristics of papulopustular rosacea. First, a burning or stinging sensation, which was the most common secondary feature, had no correlation with the development of the severity of this subtype, while a strong correlation was found with the erythematotelangiectatic and ocular rosacea. Second, edema (as a secondary feature) had correlation with the severity of the subtype. These results are in close agreement with those of several authors19,20.
Twenty four (14.3%) patients had ocular rosacea, including 21 cases with a mild grade. The reported incidence of ocular rosacea is variable according to the researcher, and it has ranged from 6% to 50%. This variable incidence of ocular rosacea is considered to be partly due to the condition's subjective nature, and it is partly due to the absence of definite diagnostic criteria. Some controversy exists concerning the casual relationship between the ocular and cutaneous manifestations21-23. In this study, we speculated that the development of ocular rosacea increased with the aggravation of cutaneous manifestations, and especially flushing and telangiectasia.
All eight patients diagnosed with the phymatous type had a mild degree of rhinophyma. Since this subtype is considered as late rosacea, it always accompanied the other subtypes in this study. Even though the nose was the only involved site in our study, lesions can occur on the cheeks (gnathophyma; zygophyma), forehead (metophyma), eyelids (blepharophyma) and ears (otophyma)24.
There have been few reported clinical studies that have used the new classification and grading system. There have been four previous studies in the Korean medical literature that have investigated the clinical spectrum of rosacea25-28. Among them, Shin and Kim28 adopted the new NRS classification and grading system. Although they reported overall results that were similar to our results, Shin and Kim's study did not accept the potential overlap of each subtype. This new system is useful in analyzing the subjective symptoms and cutaneous manifestations of each subtype. A well established consensus on rosacea in an Asian population is necessary since this disease has become more common. In addition, sun exposure should be considered as a critical factor in the development and aggravation of rosacea in Asian people.
Figures and Tables
Table 1
Subtypes of rosacea and their characteristics*

*Table from National Rosacea Society Expert Committee standard classification of rosacea, 20029
References
1. Pelle MT. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Rosacea. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;703–709.
3. Crawford GH, Pelle MT, James WD. Rosacea: I. Etiology, pathogenesis, and subtype classification. J Am Acad Dermatol. 2004. 51:327–341.

5. Berg M. Epidemiological studies of the influence of sunlight on the skin. Photodermatol. 1989. 6:80–84.
7. Plewig G, Kligman AM, Jansen T. Acne and rosacea. 2000. 3rd ed. Berlin, London: Springer;455.
8. Berg M, Liden S. An epidemiological study of rosacea. Acta Derm Venereol. 1989. 69:419–423.
9. Wilkin J, Dahl M, Detmar M, Drake L, Feinstein A, Odom R, et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol. 2002. 46:584–587.

10. Wilkin J, Dahl M, Detmar M, Drake L, Liang MH, Odom R, et al. Standard grading system for rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol. 2004. 50:907–912.

11. Sobye P. Aetiology and pathogenesis of rosacea. Acta Derm Venereol. 1950. 30:137–158.
13. Sibenge S, Gawkrodger DJ. Rosacea: a study of clinical patterns, blood flow, and the role of Demodex folliculorum. J Am Acad Dermatol. 1992. 26:590–593.

16. Nunzi E, Rebora A, Hamerlinck F, Cormane RH. Immunopathological studies on rosacea. Br J Dermatol. 1980. 103:543–551.

17. Hertzman AB, Randall WC. Regional differences in the basal and maximal rates of blood flow in the skin. J Appl Physiol. 1948. 1:234–241.

20. Chen DM, Crosby DL. Periorbital edema as an initial presentation of rosacea. J Am Acad Dermatol. 1997. 37:346–348.

21. Quarterman MJ, Johnson DW, Abele DC, Lesher JL Jr, Hull DS, Davis LS. Ocular rosacea. Signs, symptoms, and tear studies before and after treatment with doxycycline. Arch Dermatol. 1997. 133:49–54.

22. Akpek EK, Merchant A, Pinar V, Foster CS. Ocular rosacea: patient characteristics and follow-up. Ophthalmology. 1997. 104:1863–1867.
23. Michel JL, Cabibel F. Frequency, severity and treatment of ocular rosacea during cutaneous rosacea. Ann Dermatol Venereol. 2003. 130:20–24.
24. Jansen T, Plewig G. Clinical and histological variants of rhinophyma, including nonsurgical treatment modalities. Facial Plast Surg. 1998. 14:241–253.

25. Koo BS, Kwon HJ, Kim BC, Lee KS, Song JY. A clinical study of 133 patients with rosacea. Korean J Dermatol. 1997. 35:405–410.
26. Kim TH, Hwang SM, Lee WS, Ahn SK, Choi EH. A clinical study of rosacea. Korean J Dermatol. 2000. 38:583–588.
27. Lee SY, Choi JH, Sung KJ, Moon KC, Koh JK. A clinical study of 112 patients with rosacea. Korean J Dermatol. 2001. 39:636–642.
28. Shin JB, Kim IH. A clinical study of 90 patients with rosacea. Korean J Dermatol. 2007. 45:1161–1169.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download