Abstract
Leukemia cutis is the cutaneous involvement of leukemic neoplastic cells. It is an uncommon feature of systemic leukemia, and is associated with a poor prognosis. A 20-year-old man presented with a solitary, 2 cm domeshaped, firm, erythematous nodule on the right medial malleolus that was present for 3 months. The patient had a history of venous catheter insertion at the right medial malleolus area 3 months previously. The history was significant for acute lymphoblastic leukemia (ALL) for 4 years; an allogenic bone marrow transplantation was performed 3 years earlier. The histologc examination of the lesion revealed diffuse infiltration of leukemic cells in the dermis and subcutis. Herein we report a case of leukemia cutis at the site of a prior catheter insertion in a patient with ALL.
Leukemia cutis is a specific cutaneous eruption caused by infiltration of malignant hematopoietic cells. It is uncommon in patients with acute lymphoblastic leukemia (ALL) compared to other types of leukemia. The clinical features of leukemia cutis are variable, including papules, macules, plaques, nodules, ecchymoses, palpable purpura, and ulcerative lesions1. The lesions may be localized or disseminated, and can occur at any site on the skin. However, there are some reports of leukemia cutis at sites of previous trauma, burns, and herpetic infections2-5. To date, only three cases of leukemia cutis at a site with prior trauma have been reported in patients with acute leukemia (Table 1). Herein we report a case of leukemia cutis at the site of a prior catheter insertion in a patient with ALL.
A 20-year-old man with ALL was referred to our clinic for evaluation of a skin nodule on the right medial malleolus area. The patient was previously diagnosed with ALL in July 2004, and received an allogenic bone marrow transplantation in December 2004. Four months later, the ALL relapsed and a donor peripheral blood stem cell transplant was performed. However, since then the patient has had multiple extramedullary relapses in the cervical spine, ribs, pelvic bones, and muscles. In addition, radiation therapy and chemotherapy treatments have been provided.
In January 2008, the patient presented to the dermatology clinic with an erythematous nodule in the right medial malleolus area (Fig. 1). Previously, a venous catheter had been inserted at the same area, but removed due to the development of a hematoma. The hematoma persisted without resorption. Because a hematoma was suspected at the site, we attempted an incision and drainage. However, no blood clot or purulent discharge was observed. Thus, a skin biopsy was performed. On the histologic examination, the hematoxylin-eosin-stained sections showed diffuse infiltration into the dermis and subcutis (Fig. 2A). The infiltrating cells were small, polymorphic, and atypical with hyperchromatic nuclei (Fig. 2B). The atypical cells were negative for CD3 and CD20, and positive for terminal deoxynucleotidyl transferase (TdT) and CD79a (Fig. 3). The immunophenotyping findings showed the infiltrating cells were precursor B-cells. The patient was diagnosed with skin involvement of the ALL. Chemotherapy with IFN-α, mercaptopurine and methylprednisolone was continued, but the patient died 2 months later after diagnosis of leukemia cutis.
Metastasis of cancer from its primary site to secondary sites occurs by dislodging of cancer cells from the primary tumor, penetrating through lymphatic and blood vessels, and establishing new growth at a new site in normal tissue. Leukemia cutis is defined as cutaneous infiltration by circulating neoplastic leukocytes through blood vessels and can cause specific and non-specific skin lesions. The specific skin lesions caused by leukemic neoplastic cells are characterized by generalized erythema, exfoliation, macules, nodules, papules, ulcers, and plaques, with or without hemorrhagic manifestations. On histologic findings, most types of leukemic skin infiltrates show a perivascular or diffuse infiltrate involving the dermis and subcutis with sparing of the upper papillary dermis. Mycosis fungoides, cutaneous T- and B-cell lymphomas, multiple myeloma, and malignant reticulosis should be differentiated.
Leukemia cutis can be found in 10% to 50% of patients with monocytic leukemia, but is less common in patients with lymphocytic leukemia, ranging from 1.3% to 3%.6,7. This difference is due to the distinct biologic characteristics of the leukemia. Lichtman and Weed8 reported that leukemic monocytes were more adhesive, phagocytic, and readily deformable compared to leukemic myeloblasts. As a result, leukemic monocytes are better able to adhere to the vascular wall, and to traverse small gaps between the endothelial cells. Therefore, monocytes can easily invade extravascular areas and form cutaneous tumors8. This is a possible explanation for the high incidence of leukemia cutis in monocytic leukemia, in contrast to the other forms of leukemia.
Leukemia cutis in ALL commonly presents as single or multiple, red-to-violaceous papules or nodules on the head and neck7. Although leukemia cutis often presents as disseminated lesions, localization to sites of minor trauma, scars, as well as Hickman catheter sites have rarely been reported, thus the incidence is not known2-4. Also, in solid organ cancers, such as head and neck cancer, thymic cancer, or lung cancer, tumor metastasis to the sites of gastrostomy or needle biopsy tracts have been reported. However, the overall reported incidence of tumor dissemination in the needle tract is <1%9. Among the cases of leukemia cutis related to catheter insertion, two cases occurred in patients with acute myelomonocytic leukemia. Since the incidence of leukemia cutis in patients with ALL is lower than other types of leukemia, only one case of leukemia cutis at a trauma site has been reported in a patient with Burkitt leukemia, a rare form of ALL (Table 1). The case reported herein is the second case reported of leukemia cutis at the site of trauma in a patient with ALL.
An explanation for the predilection of tumor cells for trauma sites has been offered. Fisher et al10 reported that mechanical, chemical, or surgical trauma causes increased adherence of tumor cells to vessel walls as a result of endothelial damage and increased blood flow to the inflammatory site. They also suggested that substances from granulation tissue may attract tumor cells and promote the localization of tumor cells to the trauma site10. Sanz et al11 hypothesized that a major disruption of a vessel wall and leakage of sufficient amounts of soluble growth factors and cell mediators into the subcutaneous tissue might provide a protected environment in which viable atypical tumor cells could survive and proliferate. Another possible explanation reported by Rosenblum et al12 involved trauma-specific and subcutaneous-specific tumor cell migration. Preferential expression of specific chemokine receptors on leukemic cells may account for the migration of these cells to specific sites. It is possible that tumor cell subclones expressing specific chemokine receptors may have been selected for by chemotherapy, resulting in the preferential trafficking of the leukemic cells to the trauma sites12. However, further study is needed to confirm the above possibilities.
Conventional chemotherapy is recommended for leukemia cutis. Small lesions may be treated with surgical removal or local radiotherapy13. The prognosis of leukemia cutis is poor. According to Su et al1, 37 of 42 leukemia cutis patients (88%) died within 1 year. The patient reported herein died 2 months after the diagnosis of leukemia cutis.
In conclusion, this is a rare case of leukemia cutis in a patient with ALL. The skin lesion developed at a prior catheter insertion site. The disease had a rapid progression and poor prognosis.
Figures and Tables
 | Fig. 1Asymptomtic, solitary, domeshaped, firm, erythematous nodule on the right medial malleolus area. |
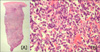 | Fig. 2(A) The skin biopsy specimen of the nodule showed diffuse infiltration in the dermis and subcutis (H&E, ×40). (B) The infiltrated cells were small, polymorphic, atypical cells having hyperchromatic nuclei (H&E, ×400). |
References
1. Su WP, Buechner SA, Li CY. Clinicopathologic correlations in leukemia cutis. J Am Acad Dermatol. 1984. 11:121–128.

2. Koizumi H, Kumakiri M, Ishizuka M, Ohkawara A, Okabe S. Leukemia cutis in acute myelomonocytic leukemia: infiltration to minor traumas and scars. J Dermatol. 1991. 18:281–285.

3. Baden TJ, Gammon WR. Leukemia cutis in acute myelomonocytic leukemia. Preferential localization in a recent Hickman catheter scar. Arch Dermatol. 1987. 123:88–90.

4. Burns CA, Scott GA, Miller CC. Leukemia cutis at the site of trauma in a patient with Burkitt leukemia. Cutis. 2005. 75:54–56.
5. Kim JE, Kim MY, Kim HO, Park YM. Plasma cell leukaemia cutis preferentially localized to recent puncture sites. Br J Dermatol. 2004. 151:237–238.

6. Braverman IM. Skin signs of systemic disease. 1981. 3rd ed. Philadelphia: Saunders;179–196.
7. Su WP. Clinical, histopathologic, and immunohistochemical correlations in leukemia cutis. Semin Dermatol. 1994. 13:223–230.
8. Lichtman MA, Weed RI. Peripheral cytoplasmic characteristics of leukocytes in monocytic leukemia: relationship to clinical manifestations. Blood. 1972. 40:52–61.

9. Matsumoto K, Ashizawa K, Tagawa T, Nagayasu T. Chest wall implantation of thymic cancer after computed tomography-guided core needle biopsy. Eur J Cardiothorac Surg. 2007. 32:171–173.

10. Fisher B, Fisher ER, Feduska N. Trauma and the localization of tumor cells. Cancer. 1967. 20:23–30.

11. Sanz MA, Larrea L, Sanz G, Martin G, Sempere A, Gomis F, et al. Cutaneous promyelocytic sarcoma at sites of vascular access and marrow aspiration. A characteristic localization of chloromas in acute promyelocytic leukemia? Haematologica. 2000. 85:758–762.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download