Abstract
The acral regions of the limbs of Asians are predisposed to develop malignant melanoma, but giant-sized acral melanoma has not been previously reported in the Asian population. Giant-sized melanoma implies aggressive tumor invasion and so it is more difficult to achieve a therapeutic cure. A 56-year-old woman presented with a giant acral melanoma of the left thumb with concomitant bone destruction and axillary lymph node metastasis. The initial lesion was a subungual black macule on the left thumb that had grown into a giant 7.0×4.0×3.5 cm-sized melanoma over a 3 year period. The left thumb was amputated and the axillary lymph nodes were completely dissected. During the ensuing 3 months, she underwent adjuvant treatment with interferon-alpha-2a. The interesting feature of this case is that the large melanoma mass of this patient, which was accompanied with adjacent bone destruction and lymph node metastasis, had developed rapidly from a small black macule in the nail matrix, and this black macule was suspected to be a subungual melanoma.
Malignant melanoma that presents as a giant mass has only very rarely been described in the medical literature, and especially with regard to acral lesions. The tumor size itself is not included in the melanoma staging system. Yet a large melanoma size, and particularly larger than 5 cm in diameter, implies a thicker depth of tumor invasion and more difficulties for achieving a therapeutic cure. We describe here a female patient with a giant acral melanoma of the left thumb that had destroyed the adjacent bones and the tumor had metastasized to the axillary lymph nodes.
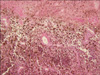
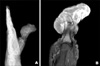
A 56-year-old woman presented with a black ulcerated tumor surrounding her left thumb; the tumor dimensions were 7.0×4.0×3.5 cm (Fig. 1). She had first noticed a black subungual macule under the thumb nail 3 years previously, but she did not consult a doctor because the lesion was asymptomatic. However, the lesion grew rapidly and it became painful and the patient visited our hospital on April, 2008. Malignant melanoma was diagnosed after a histological examination that revealed atypical epithelioid melanocytes that were positive for S-100, Melan A and HMB-45 (Clark's level V). The Breslow's depth, which was obviously over 4 mm, could not be calculated because the punch biopsy contained only a portion of the tumor (Fig. 2). X-ray and MRI analyses revealed that the dorsal radial aspect of the proximal phalanx along with most of the distal phalanx was destroyed (Fig. 3). Since a palpable left axillary lymph node was present, a metastatic workup that employed a chest computed tomography (CT) scan and a positron emission tomography/CT (PET/CT) scan was also performed. The CT scan revealed a 7.5×5.8 cm-sized enhancing mass in the left axilla, and the mass showed increased glucose metabolism on the PET/CT scan. However, there were no signs of distant metastases. The laboratory analyses revealed the patient had elevated lactate dehydrogenase (LDH) levels in her blood (547 IU/L).
In cooperation with the orthopedists and breast surgeons in our Malignant Melanoma Study Group, the left thumb was amputated at the proximal one-third of the metacarpal bone and the left axillary lymph nodes were completely dissected. Histological examination of the lymph nodes confirmed the diagnosis of metastasis of malignant melanoma, and one of the 17 harvested lymph nodes showed a nodal macrometastatic mass that exhibited gross extracapsular extension. Starting one month after surgery, interferon-alpha-2a was given subcutaneously at a dose of 17 MIU 3 times weekly for 3 months.
In the melanoma staging system, thickness and ulceration are primarily used in the T category instead of the tumor size itself. However, a large tumor size implies a thick tumor invasion depth and it is obviously more difficult to completely remove a melanoma if it is giant-sized, and particularly if it is larger than 5 cm in diameter. Large melanoma masses have rarely been reported in the literature, mainly because patients tend to come for treatment early before the tumor enlarges and practitioners are well aware of the catastrophic consequences of neglecting such tumors1. In the available literature, we found ten reports of malignant melanoma that presented as a giant mass1-10. Of these, three cases were nodular melanomas1-3, two were giant congenital melanocytic nevi4,5 and one was a metastatic melanoma6. However, there has been only one report of a giant acral melanoma; in that case, the tumor occurred on the palmoplantar area7. The patient we present here is quite unique because her giant melanoma developed from a small subungual macule that is suspected to have been a subungual melanoma. Furthermore giant acral melanoma in an Asian has not been previously reported. It is also interesting that in the case described here, wide-spread destruction of the adjacent bones accompanied the melanoma, which has also been rarely reported.
With regard to our patient, there were no signs of distant metastasis despite the giant size of the primary tumor. Since surgery, she has been undergoing adjuvant therapy with interferon-alpha-2a and this has continued up to the time of writing. We will follow her closely for signs of locoregional and distant recurrence.
Figures and Tables
 | Fig. 1A melanoma measuring 7.0×4.0×3.5 cm is surrounding the left thumb. Ulceration and spontaneous bleeding can be observed. |
References
1. Benmeir P, Neuman A, Weinberg A, Sucher E, Weshler Z, Lusthaus S, et al. Giant melanoma of the inner thigh: a homeopathic life-threatening negligence. Ann Plast Surg. 1991. 27:583–585.

2. Pai RR, Kini H, Kamath SG, Kumar S. Giant hanging melanoma of the eyelid skin. Indian J Ophthalmol. 2008. 56:239–240.

3. Panajotovic L, Dordevic B, Pavlovic MD. A giant primary cutaneous melanoma of the scalp--can it be that big? J Eur Acad Dermatol Venereol. 2007. 21:1417–1418.
4. Marano SR, Brooks RA, Spetzler RF, Rekate HL. Giant congenital cellular blue nevus of the scalp of a newborn with an underlying skull defect and invasion of the dura mater. Neurosurgery. 1986. 18:85–89.

5. Schneiderman H, Wu AY, Campbell WA, Forouhar F, Yamase H, Greenstein R, et al. Congenital melanoma with multiple prenatal metastases. Cancer. 1987. 60:1371–1377.

6. Morita K, Kudo H, Fujii K, Okamoto H, Matsubara K, Kanauchi H, et al. Giant metastatic malignant melanoma with an unknown primary site. J Dermatol. 1994. 21:442–446.

7. Zeebregts CJ, Schraffordt Koops H. Giant melanoma of the left thumb. Eur J Surg Oncol. 2000. 26:189–190.

8. De Giorgi V, Massi D, Carli P. Giant melanoma displaying gross features reproducing parameters seen on dermoscopy. Dermatol Surg. 2002. 28:646–647.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download