Abstract
Primary osteoma cutis is characterized by the formation of normal bone tissue in the dermis or subcutis without any underlying tissue abnormality or pre-existing calcification. This illness is associated with Albright hereditary osteodystrophy (AHO), which is characterized by such physical features as a short stature, round face, obesity, brachydactyly and osteoma cutis. Pseudohypoparathyroidism (PHP) is an inherited metabolic disorder that's characterized by resistance to parathyroid hormone, and PHP is present in most AHO patients. An AHO phenotype without hormonal resistance is called pseudopseudohypoparathyroidism (PPHP). Osteoma cutis is less common in patients with PPHP than in patients with PHP. We present here a case of osteoma cutis as the cardinal manifestation of AHO associated with PPHP. Osteoma cutis is an important sign of AHO and its significance should not be overlooked, even if the patient has normal values on the serum biochemical tests.
Albright hereditary osteodystrophy (AHO) was first described by Fuller Albright in 1942, and AHO is a rare metabolic disorder1. It is characterized by a multitude of physical features, including a short stature, round face, obesity, brachydactyly and osteoma cutis. Mental retardation has been less frequently described in patients with AHO. AHO is often associated with pseudohypoparathyoidism, which is characterized by resistance to parathyroid hormone. Hypocalcemia, hyperphosphatemia and an increased serum concentration of parathyroid hormone (PTH) are observed in patients with AHO. Patients with an AHO phenotype and who are without hormonal resistance have a condition called pseudopseudohypoparathyroidism (PPHP). Patients with PPHP show normal levels of serum calcium, phosphorus and PTH. We present here a case of osteoma cutis in an 11-year-old girl who had the phenotypic features of AHO with normal biochemical parameters.
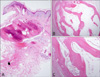
An 11-year-old girl presented with a 10 year history of several asymptomatic hard cutaneous nodules located on the palm, finger and sole of her foot. The lesions were first seen by the parents when the girl was 1 year old and the lesions had slightly increased in size since they first appeared. She was born healthy and there was no family history of similar lesions. The physical examination yielded a height of 135 cm (5th percentile for a normal Korean girl), a round face, malocclusion of teeth and shortened left 4th and 5th fingers and 4th toe (Fig. 1). The cutaneous examination showed skin-colored, hard, mildly tender nodules; there was a 2.5×2 cm sized nodule on her left sole, a 1×1 cm sized nodule on her right palm and a 0.4×0.4 cm sized nodule on her left 5th finger (Fig. 2). The laboratory studies that included a complete blood cell count, blood chemistry and urinalysis were within the normal limits. Further investigation revealed a normal parathyroid hormone level of 21.6 pg/ml (reference range: 8~76), a calcium level of 9.5 mg/dl (reference range: 8.4~10.2) and a phosphorus level of 5.5 mg/dl (reference range: 2.5~5.6). The thyroid function tests were within the normal limits. Radiologic studies demonstrated cutaneous ossification at the sites of the nodules (Fig. 3). Short 4th and 5th metacarpal bones were observed bilaterally and a short 4th metatarsal bone was observed in the left foot (Fig. 4). Histopathologic examination of the three nodules revealed small spicules to large masses of mature bone in the dermis. The bony tissue was composed of osteocytes, osteoblasts, Haversian canals and condensed mesenchyme (Fig. 5). Based on these clinical, biochemical, radiologic and histological features, we made the diagnosis of osteoma cutis in a patient with AHO associated with PPHP.
Osteoma cutis is characterized by the formation of normal bone tissue within the dermis or the subcutis2. It is an unusual condition that may be primary or secondary to inflammatory, neoplastic or traumatic processes. Secondary osteoma cutis is more common than primary osteoma cutis3. Most cases of secondary osteoma cutis are due either to tumors, such as pilomatricomas, chondroid syringomas, basal cell carcinomas, pilar cysts or naevi, or to inflammatory conditions such as scars and venous stasis4. Primary osteoma cutis rarely occurs without any underlying tissue abnormality or pre-existing calcification. There are four well described ossifying syndromes5: fibrodysplasia ossificans progressova, AHO, progressive osseous heteroplasia and plate-like osteoma cutis.
AHO is a rare syndrome that's characterized by a variety of several distinct physical features, including a short stature, obesity, round face, cutaneous ossifications, brachydactyly and other skeletal anomalies6. Some AHO patients have mental retardation. Osteoma cutis mostly appears in the periarticular regions such as the scalp, and particularly the hands and feet, but it can occur anywhere in the body7. The ossification is usually not progressive or painful. In addition, PHP is present in most AHO patients, and PHP is an inherited metabolic disorder that's characterized by end organ resistance to the action of PTH8. Resistance to PTH leads to hypocalcemia and hyperphosphatemia. AHO is observed in PHP type Ia and Ic, which are two of the four subtypes of PHP. When AHO is present with normal levels of serum calcium, phosphorus and parathyroid hormone, then it is termed PPHP. This is an inherited disorder that's caused by a mutation in the gene encoding the alpha subunit of the adenylate cyclase stimulatory G protein (GNAS), and this gene is imprinted on the paternal chromosome, whereas PHP-Ia is caused by maternally inherited mutations9. Unlike the patients with PHP-Ia, PPHP patients present only with the skeletal defects and no defects of the calcium and phosphorus homeostasis. The precise pathogenesis of osteoma cutis in the patients with PHP-Ia and PPHP is not well understood. Osteoma cutis does not seem to be due to PTH resistance9. Decreased Gsα activity has recently been directly linked to osteogenic differentiation in human mesenchymal cells10. Both PHP-Ia and PPHP patients have reduced Gs α activity because of the heterozygous inactivating mutations in the GNAS gene. Therefore, it provides a potential explanation for the development of ectopic bone in patients with Albright's hereditary osteodystrophy associated with PHP-Ia and PPHP. Osteoma cutis and obesity are observed less frequently in patients with PPHP than in those patients with PHP7,11. The frequency of osteoma cutis in patients with PPHP is unknown. In one report, cutaneous calcification was observed in 42% of the patients with PHP and in 27% of the patients with PPHP12. In the absence of biochemical abnormalities, the significance of osteoma cutis may be overlooked and the correct diagnosis of AHO may be delayed13. Furthermore, the typical phenotype of a short stature, round face and brachydactyly is less apparent in young children than in adults14. The radiologic findings of these patients can be very helpful for diagnosing AHO15. Ossification of the skin and subcutaneous tissues and shortening of the metacarpal, metatarsal and phalangeal bones, and especially the 4th metacarpal, are seen on radiography.
In our patient, osteoma cutis was the presenting cardinal sign of AHO. She also exhibited a short stature, round face and brachydactyly with shortening of the metacarpal and metatarsal bones. The serum levels of calcium, phosphorus and PTH were normal. Therefore, our patient had the typical phenotype of AHO and the biochemical features of PPHP.
We herein document an interesting case of osteoma cutis as the presenting sign of AHO associated with PPHP. AHO is a rare and unfamiliar condition to most dermatologists and some AHO cases can be difficult to diagnose. It is important for dermatologists to be aware of the phenotypic features of AHO. When multiple cutaneous ossifications are observed in a young child, then AHO should be considered and performing subsequent biochemical and radiologic studies is recommended.
Figures and Tables
Fig. 1
Photograph showing the round face (A), malocclusion of teeth (B), the shortened 4th and 5th fingers (C) and the shortened left 4th toe (D).

References
1. Albright F, Burnett CH, Smith PH, Parson W. Pseudohypoparathyroidism: an example of Seabright-Bantam syndrome. Endocrinology. 1942. 30:922–932.
2. Novak C, Siller G, Wood D. Idiopathic multiple miliary osteomas of the face. Australas J Dermatol. 1998. 39:109–111.

3. Roth SI, Stowell RE, Helwig EB. Cutaneous ossification. Report of 120 cases and review of the literature. Arch Pathol. 1963. 76:44–54.
4. Sethuraman G, Malhotra AK, Khaitan BK, Kumar R, Sharma VK, Kabra M, et al. Osteoma cutis in pseudohypoparathyroidism. Clin Exp Dermatol. 2006. 31:225–227.

5. Walsh JS, Fairley JA. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Cutaneous mineralization and ossification. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;1296–1297.
6. Kapoor S, Gogia S, Paul R, Banerjee S. Albright's hereditary osteodystrophy. Indian J Pediatr. 2006. 73:153–156.

7. Trueb RM, Panizzon RG, Burg G. Cutaneous ossification in Albright's hereditary osteodystrophy. Dermatology. 1993. 186:205–209.

8. Wilson LC, Hall CM. Albright's hereditary osteodystrophy and pseudohypoparathyroidism. Semin Musculoskelet Radiol. 2002. 6:273–283.

9. Gelfand IM, Hub RS, Shore EM, Kaplan FS, Dimeglio LA. Progressive osseous heteroplasia-like heterotopic ossification in a male infant with pseudohypoparathyroidism type Ia: a case report. Bone. 2007. 40:1425–1428.

10. Lietman SA, Ding C, Cooke DW, Levine MA. Reduction in Gsalpha induces osteogenic differentiation in human mesenchymal stem cells. Clin Orthop Relat Res. 2005. 231–238.
11. Long DN, McGuire S, Levine MA, Weinstein LS, Germain-Lee EL. Body mass index differences in pseudohypoparathyroidism type 1a versus pseudopseudohypoparathyroidism may implicate paternal imprinting of Galpha(s) in the development of human obesity. J Clin Endocrinol Metab. 2007. 92:1073–1079.

12. Eyre WG, Reed WB. Albright's hereditary osteodystrophy with cutaneous bone formation. Arch Dermatol. 1971. 104:634–642.

13. Prendiville JS, Lucky AW, Mallory SB, Mughal Z, Mimouni F, Langman CB. Osteoma cutis as a presenting sign of pseudohypoparathyroidism. Pediatr Dermatol. 1992. 9:11–18.

14. Monn E, Osnes JB, Oye I, Wefring KW. Pseudohypoparathyroidism: a difficult diagnosis in early childhood. Acta Paediatr Scand. 1976. 65:487–493.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download