Abstract
Congenital leukemia is a rare condition diagnosed at birth to 6 weeks of life with an estimated incidence of 4.7 per million live births. In a review, about 25~30% of cases were well documented as leukemia cutis. We report a case of a 3-month-old infant presented with asymptomatic multiple erythematous to bluish patches and nodules, which had developed about two months ago. Biopsy of the cutaneous lesions revealed immature cells which are overall monotonous with large kidney shaped nucleus, prominent nucleoli and moderate cytoplasm. These atypical cells stained positive for leukocyte common antigen, lysozyme and CD68. With this result, a congenital leukemia cutis was diagnosed. Six months later, she underwent cord blood stem cell transplantation. Seven months after the cord blood stem cell transplantation, the bone marrow examination revealed a normal result. Leukemia can be presented in the skin, the eruption may be nonspecific and it may precede systemic involvement. The recognition is important because early diagnosis can lead to appropriate treatment, followed by better prognosis.
Congenital leukemia cutis is rarely reported in the dermatologic literature despite various authors citing 25~30% of infants with congenital leukemia having skin involvement. It is presented as firm erythematous to violaceous to blue macules, papules, and nodules with the result of infiltrating leukemic cells in the skin. We report a case of a 3 month-old infant with congenital acute myeloid leukemia whose cutaneous disease completely resolved with cord blood stem cell transplantation.
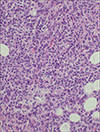
A 3 month-old girl presented with asymptomatic multiple erythematous to bluish patches and nodules on right eyelid, scalp, trunk, right arm and left thigh, which had developed about two months ago (Fig. 1). There were no specific findings on past history and family history. The remainder of physical examinations was unremarkable. On laboratory examination, there were no abnormal findings with complete blood cell count, peripheral blood smear and urinary analysis. A biopsy specimen taken from the skin of the left flank showed immature cells which are overall monotonous with large kidney shaped nucleus, prominent nucleoli and moderate cytoplasm (Fig. 2). On immunohistochemical staining, the specimen showed positive findings on LCA, the antigen of leukocytes. It also showed positive findings on lysozyme and CD68, the antigen of monocytes (Fig. 3). It stained negative for CD3, UCHL1, CD20, CD79a, myeloperoxidase and toluidine blue. This lesion was interpreted as acute monocytic leukemia.
On iliac bone marrow aspiration smears and iliacbiopsy section, there were many monoblasts, with large nuclear-cytoplasmic ratio, kidney-shaped nucleus and moderate cytoplasm without eosinophilic granules. After considering all those results, she was diagnosed as congenital leukemia cutis. She was transferred to pediatric hemato-oncology department, and was started on induction chemotherapy for AML with Idarubicin and Behenoyl-ara-C (BHACBHAC). After the remission, she underwent consolidation therapy with BH-AC, Mitox, IT Ara-C, and the leukemic cutaneous infiltrates resolved completely. Three months later, she underwent cord blood stem cell transplantation. Periodic examination during follow-up revealed no recurrence. Seven months after the cord blood stem cell transplantation, the bone marrow examination revealed a normal result. At the time of writing this report the infant was continuing to grow and develop normally.
Congenital leukemia is a rare condition diagnosed at birth to 6 weeks of life with an estimated incidence of 4.7 per million live births1. In a review, about 25~30% of cases are well documented as leukemia cutis2. Leukemia cutis usually develops several months after the diagnosis of systemic leukemia, although it occasionally precedes it. The most common varieties of congenital leukemia are of the myelocytic (M4) or monocytic (M5) FAB subtypes and rarely of lymphoblastic subtypes3.
Diagnosis of congenital leukemia cutis may be difficult, because most patients present with asymptomatic clinical manifestations. The commonest skin presentation is multiple papules, nodules or infiltrated plaques4. Byrd et al5. found that 47% of confirmed cases with extramedullary leukemia were initially misdiagnosed, often as lymphoma.
The diagnosis is made by suspicion and verified by skin biopsy, immunophenotyping, and B or T cell receptor rearrangement studies. Hematologic studies with complete analysis of bone marrow aspirate and peripheral blood smear are then needed to confirm the diagnosis6. Both acute and chronic forms of myeloid progenitors in the bone marrow cells are histochemically positive for myeloperoxidase, Sudan black B, chloroacetate esterase, and naphthol-ASD-chloroacetate esterase (Leder) stains. Myeloid cells do not express B-lineage or T-lineage markers, but may show immunohistochemical staining for the myeloid markers CD13, CD33, CD15, CD117 or megakaryoblastic antigens C41 and CD617.
In our patients, at first, we considered a diagnosis of cutaneous mastocytosis, lymphoma or leukemia. To differentiate, we performed a biopsy on left abdomen. From the results of immunohistochemical stains, we could exclude lymphoma from the fact that it showed negative findings on CD3, UCHL, CD20, CD79a, which are the markers for lymphocytes. And we could also rule out mastocytosis from the negative findings on giemsa and toluidine blue stains. It showed negative on myeloperoxidase, the markers for granulocytes and positive on CD 68 stain, the markers for monocytes. After considering all those results, she was diagnosed as acute monocytic leukemia M5B.
Accurate identification is important in scheduling adequate management of patients with leukemia, particularly in cases where skin lesions are the first clinical sign of the disease. Most reports demonstrated that local irradiation alone is ineffective in preventing subsequent development of overt leukemia and the outcome is dismal. Conventional chemotherapy regimens are advocated in leukemia cutis. In our case, she underwent a successful cord blood stem cell transplantation after systemic chemotherapy.
Whereas leukemia cutis is associated with a poor prognosis in adult leukemics, the natural history of congenital leukemia is not altered by leukemia cutis8. The natural history of congenital leukemia is nearly universally lethal if not treated, with almost all infants dying by 2 months9. The survival rate of congenital AML is reported to be as low as 26%, compared with older children who have an improved survival rate of 40% to 60%10. Its early recognition is important, because early diagnosis can lead to appropriate treatment, followed by a better prognosis. We, herein, report a case of congenital leukemia cutis treated successfully with cord blood stem cell transplantation.
Figures and Tables
References
1. Landers MC, Malempati S, Tilford D, Gatter K, White C, Schroeder TL. Spontaneous regression of aleukemia congenital leukemia cutis. Pediatr Dermatol. 2005; 22:26–30.

2. Ferandez RC, Median A, Martin NA, Rios E, Sosa R, Plaza E, et al. A new case of congenital leukemia with leukemia cutis. Sangre (Barc). 1995; 40:513–516.
3. Bresters D, Reus AC, Veerman AJ, van Wering ER, van der Does-van den Berg A, Kasper GJ. Congenital leukemia: the Dutch experience and review of the literature. Br J Haematol. 2002; 117:513–524.
4. Wilkins R, Janes S. Aleukemic leukemia cutis: case report and review of the literature. Clin Lab Haematol. 2004; 26:73–75.

5. Byrd JC, Edenfield WJ, Shields DJ, Dawson NA. Extramedullary myeloid cell tumors in acute nonlymphocytic leukemia: a clinical review. J Clin Oncol. 1995; 13:1800–1816.

6. Wolff K, Johnson RA, Suurmond D. Fitzpatrick's color atlas & synopsis of clinical dermatology. 5th ed. New York: McGraw-Hill;2005. p. 512–514.
7. Murphy GF, Schwarting R. Cutaneous lymphomas and leukemias. . In : Elder DE, Elenitsas R, Hohnson BL, Murphy GF, editors. Lever's histopathology of the skin. 9th ed. Philadelphia: Lippincort;2005. p. 925–978.
8. Resnik KS, Brod BB. Leukemia cutis in congenital leukemia. Analysis and review of the world literature with report of an additional case. Arch Dermatol. 1993; 129:1301–1306.

9. Ro YS, Moon DG, Lee CW, Han HG, Lee H, Choi JK. A case of congenital leukemia cutis. Korean J Dermatol. 2000; 38:1089–1093.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download