INTRODUCTION
Pseudoxanthoma elasticum (PXE) is a rare, inherited, multisystemic disorder. It is characterized by progressive calcification and degeneration of elastic fibers resulting in a diagnostic pathologic picture referred to as "elastorrhexia"123. Skin lesions almost always begin on the lateral portion of the neck during early childhood and remain confined to the flexural area, except in the most advanced cases, in which the trunk, face, and extremities may be involved4. However, mild forms of the disorder can easily be overlooked2. Skin biopsy remains the best way to diagnose PXE. To date, the majority of reports have focused on the typical clinical symptoms of PXE, the associated systemic abnormalities of PXE, or perforating PXE. Localized, acquired cutaneous PXE has been proposed as a non-heritable form that is nearly identical to the heritable form4. Recently, a previously undescribed cutaneous finding (mental creases) in a patient with PXE was reported5. However, we describe a patient with localized PXE-like histologic changes who had only had an itching sensation on the chin, without any skin surface changes.
CASE REPORT
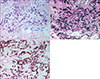
A 60-year-old female presented with a 10-year history of pruritus on the chin. She did not have a family history of PXE. Her past medical history was unremarkable. The physical examination revealed no skin lesions, but she complained of a severe itching sensation on the chin of more than 10 years duration (Fig. 1). A punch biopsy specimen from the chin showed short, irregularly thickened, basophilic fibers in the mid-dermis (Fig. 2A). Accumulations of swollen and irregularly clumped fibers stained deep black with Verhoeff's stain (Fig. 2B). Staining for calcium with von Kossa was positive in the abnormal fibers (Fig. 2C). We recommended that she see an ophthalmologist for an ocular examination, but she did not keep the follow-up visit with us.
DISCUSSION
PXE is a rare, genetic disorder primarily affecting the skin, eyes, and cardiovascular system. The inheritance is usually autosomal recessive, but may be autosomal dominant or sporadic. Cutaneous lesions usually occur in the second or third decade of life6. However, the presence of cutaneous lesions is usually not noted until adolescence or even later adulthood because of the asymptomatic nature. The primary skin lesions are small, yellowish papules in a linear or reticular pattern, tending to gradually coalesce to form plaques giving the skin a "plucked chicken" appearance127. A skin biopsy specimen is mandatory for the diagnosis of PXE to demonstrate the cardinal histologic features. PXE is characterized by degenerative changes affecting the elastic fibers of the mid-dermis. The elastic fibers are readily identifiable with hematoxylin and eosin (H&E) staining and are rather basophilic and irregular, appearing as widely dispersed granular material amidst normal collagen fibers. Fibers stain positively with the von Kossa technique, confirming the presence of calcium and phosphorous. In our case, there was no distinct skin finding, except the severeitching sensation localized to the chin of about 10 years duration. She did not have a family history of PXE. She was 60 years of age at that time of the skin biopsy, which showed PXE-like histologic changes, although she had unusual clinical features. Solar elastosis, which also exhibits abnormal elastic tissue, was easily excluded because in solar elastosis the material is located in the upper dermis and presents as dense masses rather than individual altered fibers. Moreover, these dense masses always stain negative for calcium.
Several types of localized PXE have been reported. According to Neldner and Martinez-Hernandez4, localized acquired cutaneous PXE is a non-heritable form of PXE that is nearly identical to the heritable form on the basis of the cutaneous appearance of the individual lesions, light microscopic criteria, and ultrastructural criteria. Localized acquired cutaneous PXE is distinguished from the more common syndrome by a late onset, absence of flexural clinical lesions, absence of retinopathy, a negative family history, and absence of the other expected systemic manifestations. In this report, different biochemical pathways are suggested; any condition that results in a sustained elevation of serum calcium and/or phosphate can result in cutaneous calcification that may or may not involve elastic tissue, and with specific regard to elastic tissue, different biochemical pathways can lead to the same outcome with calcified elastic fibers. Another localized form is localized acquired (periumbilical) perforating PXE. In most cases involving this type, the localized lesion occurs predominantly in middle-aged, multiparous, obese black women. Characteristically, it is an abdominal plaque located superior to the umbilicus8. In consideration of the clinical manifestations, and personal or family history, our case might belong to the former type of localized PXE.
Until now, more than 20 reports involving PXE have been published in Korea, most of which present cases with typical clinical symptoms, associated systemic abnormalities, or perforating PXE. Unlike previous reports, our patient complained of severe pruritus on a normal appearing chin without other systemic problems or a family history. Recently, Lebwohl et al5 reported a previously undescribed cutaneous finding in a patient with PXE. As a marker of PXE, mental creases are sensitive and highly specific under the age of 30 years, affecting two-thirds of patients, but not in age-matched control patients. However, there was no further description of clinical findings related to PXE. Our patient also had horizontal and oblique mental creases; however, the creases may not be specific because the development of a horizontal mental crease is not rare in individuals with advanced age. Taylor et al9 reported tumefactive lipedema with PXE-like microscopic changes. The patient could have either a subclinical form of PXE, perhaps predisposing to lipedema, or secondary elastic tissue changes resulting from the massive edema. They explained if the latter was the case, this could represent an unusual manifestation of localized acquired cutaneous PXE. Similarly, there is a possibility that PXE-like changes in our case might be secondary changes resulting from the scratching.
In summary, we present a rare case of patient who only had an itching sensation localized to the chin without typical skin surface changes of PXE or a family history, showing PXE-like histologic changes. Patients with PXE typically have a normal life span, but morbidity and mortality depend on the extent of systemic involvement. It is important to recognize the disease early in order to minimize the risk of systemic complications. Patients with PXE should receive ophthalmology and cardiology assessments on a regular basis2. Since there may be an unusual case of PXE-like conditions with only localized itching sensation, we recommend a skin biopsy in similar cases.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download