Abstract
Atrophia maculosa varioliformis cutis (AMVC) is a type of idiopathic noninflammatory macular atrophy that occurs in young individuals. It is clinically characterized by shallow, sharply demaracated depressions of various shapes. Considering that atrophia maculosa varioliformis cutis can be mistaken as scarring and artifact dermatitis, it is important for physicians to distinguish this condition and to diagnose it correctly.
Atrophia maculosa varioliformis cutis (AMVC)was first described by Heidingsfield in 1918 as a rarely reported form of idiopathic macular atrophy on the cheek1. It is clinically characterized by shallow, sharply demarcated depressions of various shapes. We report here on a 42-year-old woman whose clinical and pathological findings suggested the diagnosis of AMVC. AMVC has rarely been reported in Korean medical literature.
A 42-year-old Korean woman presented with a few months history of unusual pitted scars on her left chin. On the physical examination, the facial scars were slightly hyperpigmented and the shape varied from linear and rectangular to round (Fig. 1). They were well demarcated shallow pits that approximately ranged from 0.2 to 1.3 cm in length, and they were 0.2 cm in width and 0.1 cm in depth. The lesions occurred spontaneously without any preceding trauma or inflammation.
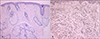
Skin biopsies were taken from both the atrophic lesion and normal skin on the chin. The lesion specimen showed normal epidermis with sparse inflammation in the dermis. There were no signs of fibrosis in the dermis (Fig. 2A). Multiple small areas of diminished and fragmented elastic tissue were seen with Verhoeff van Gieson elastic tissue staining (Fig. 2B). The patient was diagnosed with AMVC and she was treated with 0.025% retinoic acid ointment, but with little effect.
AMVC is clinically characterized by spontaneous presentation in young individuals with linear and punctate scars on the cheeks and forehead without any inflammatory changes. The etiology of AMVC is unknown, although a familial occurrence has previously been reported23, which suggests that AMVC is an inherited disorder rather than a response to an environmental insult. Cases associated with extrahepatic biliary atresia4 and pachydermodactyly5 have been described, but these associations may be coincidental.
The diagnosis of AMVC is mainly made on a clinical basis, with patients having facial atrophic lesions with sharply defined edges and an absence of erythema, induration, pigmentary changes or a honeycombed pattern. The histological features are nonspecific, with a relatively normal dermis, a slight decrease or fragmentation of the elastic fibers, an absence of fibrosis and little or no inflammation below the shallow depression of the epidermis67.
The differential diagnosis includes conditions such as scarring following acne or trauma, factitial disease and atrophoderma vermiculata. The absence of a history of any preceding inflammatory condition or of dermal fibrosis histologically rules out the above-described clinical situations. In atrophoderma vermiculata, which is now regarded as a part of the keratosis pilaris syndrome, the keratotic lesions on the face are followed by atrophic "pitted scars", while vermiculate atrophy only rarely occurs on the body8.
No specific therapeutic options have been suggested for the management of AMVC. Collagen injections, dermabrasion or laser resurfacing techniques may theoretically help improve the facial scarring. Since no follow-up data is available from the previous cases of AMVC, it may be helpful for physicians to reassure these AMVC patients of the benign and non-progressive nature of this unusual condition.
Figures and Tables
References
1. Heidingsfeld ML. Atrophia maculosa varioliformis cutis. J Cutan Dis. 1918; 36:285–288.
3. Gordon PM, Doherty VR. Familial atrophia maculosa varioliformis cutis. Br J Dermatol. 1996; 134:982–983.

4. Venencie PY, Foldes C, Cuny M, Samuel D, Bismuth H. Atrophia maculosa varioliformis cutis with extrahepatic biliary atresia. J Am Acad Dermatol. 1989; 21:309.

5. Callot V, Wechsler J, Hovnanian A, Revuz J. Pachydermodactyly and atrophia maculosa varioliformis cutis. Dermatology. 1995; 190:56–58.

6. Kolenik SA, Perez MI, Davidson DM, Morganroth GS, Kohn SR, Bolognia JL. Atrophia maculosa varioliformis cutis. Report of two cases and review of the literature. J Am Acad Dermatol. 1994; 30:837–840.
7. Nakayama H, Mihara M. Atrophia maculosa varioliformis cutis. Acta Derm Venereol. 1995; 75:252.
8. Fisher AA, Wolf M. Keratosis pilaris atrophicans faciei (Brocq). Arch Dermatol Syphilol. 1954; 69:111.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download