Abstract
A 49-year-old woman presented with a 30-year history of asymptomatic plaque on her right temple. The histological examination revealed nests of nevus cells throughout the entire dermis. Bony spicules were seen just beneath the nevus cell nests in the lower dermis. Cutaneous ossification is an unusual event. Herein, we present a case of intradermal melanocytic nevus with unusual ossification (nevus of Nanta). To the best of our knowledge, this is the first such case report in the Korean literature.
Ossification within the skin may occur in a variety of conditions, including pilomatricoma, basal cell carcinoma, appendageal and fibrous proliferation, inflammation and trauma12. The occurrence of ossification within a melanocytic nevus is an unusual event345.
Herein, we present a case of intradermal melanocytic nevus with unusual ossification (nevus of Nanta). To the best our knowledge, this is the first such case report in the Korean literature.
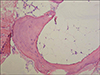
A 49-year-old woman presented with a 30-year history of asymptomatic plaque on her right temple. Dermatological examination revealed a 1.5 cm in diameter, erythematous to flesh colored, flat topped plaque with hairs (Fig. 1). She had no history of drug intake or medical illness. The histological examination showed a dense proliferation of benign nevus cells in the upper dermis. They were arranged in nests surrounding the hair follicles (Fig. 2). Bony spicules were seen in the lower dermis, underneath the nevus cell nests. Some of them were compact while others were surrounded by mature fatty tissue (Fig. 3).
Bone formation within the skin may be a primary or secondary phenomenon. Primary cutaneous ossification can occur in Albright's hereditary osteodystrophy and as primary osteoma cutis. Secondary metaplastic ossification occurs in association with a wide variety of conditions, including pilomatricoma, basal cell carcinoma, acne, melanocytic nevi, cellular blue nevus, scar, cutaneous mixed tumor, cylindroma, a cutaneous nodule of mixed connective tissue disease, dermatofibroma, ossifying plexiform tumor, pyogenic granuloma, cutis laxa-like pseudoxanthoma elasticum, congenital plate-like osteoma cutis, organoid nevi, epidermal cyst and at the site of trauma or injection6. The melanocytic nevus with secondary ossification is referred to as 'nevus of Nanta'7. Melanocytic nevus with bone was first described by Heidingsfeld in 1908. Ever since Nanta reported on it in detail in 1911, it has been called osteo-nevus of Nanta7. The histopathology of nevus of Nanta is characterized as ossification within or just beneath the nevus cell nests7.
To the best of our knowledge, the nevus of Nanta has not been reported on in the Korean medical literature, but there have been reports of large series in the international literature367. Both Conlin et al6 and Moulin et al3 reported that the nevus of Nanta was the most frequent cause of secondary ossification of the skin. The occurrence of nevus of Nanta was variable between 1.4%7 to 26%6 of all cutaneous ossifications.
The origin of the ossification within the melanocytic nevus is not precisely known. Many different theories have been proposed to explain this somewhat unusual finding. Burgdorf and Nasemann1 have suggested two mechanisms by which cutaneous ossification may occur: 1) transformation of primitive mesenchymal cells into osteoblasts that produce bone or 2) metaplastic transformation of other undetermined dermal cells that's stimulated by the appropriate cellular milieu. Keida et al8 suggested the involvement of transforming growth factor-β and connective tissue growth factor in the ossification of nevus of Nanta. Conlin et al6 reported that women were more commonly affected than men and they hypothesized there was an estrogenic effect on osteoblasts. Yet the exact reason why osteoma formation occurs remains to be determined.
In our case, the patient denied any preceding inflammation or trauma on the nevus, but it is difficult to exclude the possibility of previously unrecognized trauma or inflammation. We recommended getting an operation because there has been a reported case of malignant melanoma arising in a nevus of Nanta9, but the patient refused.
Figures and Tables
Fig. 1
A 1.5 cm in diameter, slightly erythematous to flesh colored, flat-topped hairy plaque on the right temple of the face.

References
1. Burgdorf W, Nasemann T. Cutaneous osteomas:a clinical and histopathologic review. Arch Der-mato Res. 1977; 260:121–135.
2. Elder DE, Elenitsas R, Johnson BL Jr, Murphy GF. Lever's Histopathology of the skin. 19th ed. Philadelphia: Lippincott Williams & Wilkins;2005. p. 1089–1093.
3. Moulin G, Souquet D, Balme B. Pigmented nevus and cutaneous ossifications. Apropos of 125 cases of osteonevi. Ann Dermatol Venereol. 1991; 118:199–204.
4. Kanitakis J, Claudy A. Mummified ossified melanocytic naevus. Eur J Dermatol. 2000; 10:466–467.
6. Conlin PA, Jimenez-Quintero LP, Rapini RP. Osteomas of the skin revisited: a clinicopathologic review of 74 cases. Am J Dermatopathol. 2002; 24:479–483.
7. Sasaki S, Mitsuhashi Y, Ito Y. Osteo-nevus of Nanta: a case report and review of the Japanese literature. J Dermatol. 1999; 26:183–188.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download