Abstract
Angiolymphoid hyperplasia with eosinophilia (ALHE) is a subcutaneous angioproliferating tumor with a characteristic inflammatory infiltrate that consists mainly of lymphocytes and eosinophils. A 24-year-old man presented with a firm single asymptomatic erythematous papule on the lower eyelid. Histopathological findings showed a proliferation of blood vessels lined with epithelioid cells and perivascular infiltration of lymphocytes and eosinophils. We report a case of ALHE occurring on an unusual site.
Angiolymphoid hyperplasia with eosinophilia (ALHE), first described by Wells and Whimster1 in 1969, usually manifests as firm erythematous to brownish papules on the head and neck area, especially on the periauricular area of young adults. It can appear as a single or multiple lesions. The trunk, extremities, and perineal area can be involved2. Lesions on the oral mucosa3, upper lip4, and inner canthus5 of the face have been reported. We report a patient suffering from ALHE which developed as a single papule on the lower eyelid making diagnosis difficult. ALHE on the lower eyelid has never been reported before.
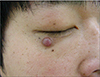
A 24-year-old man presented with an asymptomatic firm single erythematous papule on the lower eyelid. The lesion had started as a tiny papule 1 year earlier, and enlarged slowly. There was no history of trauma to the eyelid. He had been taking medication for nephrotic syndrome due to mesangioproliferative glomerulonephritis for 5 years. The family history was noncontributory. Laboratory tests including blood cell count and blood chemistry were within normal limits. On physical examination, a single shiny firm erythematous 5-mm sized, round papule was noted on the right lower eyelid (Fig. 1). There were no palpable lymph nodes. Clinically, our differential diagnosis included dermatofibroma, keloid scar, or granuloma pyogenicum. The histopathologic examination revealed dense multiple lobular infiltrations of inflammatory cells with central vessels throughout the dermis. Inflammatory cells included many eosinophils and lymphocytes (Fig. 2A). There was no lymphoid follicle formation. Vascular proliferation with prominent endothelial cells was characteristic. The endothelial cells had a hobnail appearance, protruding into the vascular lumen, and endothelial vacuoles were present (Fig. 2B, C). Immunohistochemistry revealed that the endothelial cells were positive for CD34 and well-developed pericytes were strongly positive for smooth muscle actin. Interstitial inflammatory cells were positive for vimentin and S100. The patient was diagnosed with ALHE, and treated with total excision. In the 6 months since the mass was excised, no recurrence has been observed.
ALHE is characterized by persistent, recurrent dermal or subcutaneous nodules primarily in the hand and neck area6. Although there is a predilection for the periauricular area, involvement of other skin surfaces as well as the oral mucous membranes, pharynx, and orbital has been reported7. The lesions, which are often pruritic or painful, may coalesce into confluent plaques that are chronic with little propensity for spontaneous resolution. In some cases, peripheral blood eosinophilia is present.
The etiology of ALHE remains unknown. But there are several cases of ALHE in the literature that have been associated with pregnancy, and thus, sex hormones. High prevalence of the disease among women and occurrence of the disease associated with sex hormones are two important observations that sex hormones may play role in the pathogenesis of ALHE8. Clinical presentation is very spread out, and the main differential diagnosis lies in the vascular tumors. The most important clinicopathological differential diagnosis of ALHE is Kimura's disease9. These two conditions are very similar in that they occur in the head and neck region, particularly the periauricular area. Kimura's disease mainly occurs in young Oriental males presenting with single or multiple large asymptomatic masses involving the subcutaneous tissue or salivary glands. It is often accompanied by regional lymph node enlargement, peripheral blood eosinophilia, an elevated serum IgE level, and nephrotic syndrome. By contrast, ALHE occurs in young to middle-aged females of any race, presenting with multiple small pruritic erythematous dermal papules or nodules without lymphadenopathy or laboratory abnormalities.
Histopathologically, in Kimura's disease, multiple lymphoid follicles with germinal centers and massive eosinophilic infiltration with eosinophilic abscesses are very characteristic, but vascular proliferation is minimal. By contrast, in ALHE, diffuse lymphoid and eosinophilic infiltrations without lymphoid follicles or eosinophilic abscesses are observed. Endothelial proliferation is very prominent. The thickwalled blood vessels are lined with hypertrophic "epithelioid" or "histiocytoid" endothelial cells which protrude into the vascular lumen, occasionally resulting in a "cobblestone" appearance. There is no consistently effective treatment for this disease. Intralesional injections of glucocorticoid, interferon alpha-2a, and cytotoxic agents may be effective. Although surgical excision can be curative, recurrences are common. Destructive techniques such as cryotherapy and electrodesiccation may be attempted. In addition, pulse-dye lasers have been used to selectively target the vasculoproliferative component of dis orders10.
The most common location of ALHE is head and neck, especially on the scalp, although it can be seen other areas (trunk, extremities, groin). To date, 8 cases of ALHE have been reported in the Korean literature11121314151617, but only 1 case has reported ALHE occurring on the face. Our patient had a single asymptomatic papule on the lower eyelid. The skin biopsy showed vascular proliferation, with prominent endothelial cells with lymphocyte and eosinophil infiltration, which suggested ALHE. The entire lesion was excised.
In conclusion, ALHE may be seen as one of the differential diagnoses of a lesion involving a single erythematous papule on the lower eyelid in a young adult.
Figures and Tables
Fig. 2
Histopathologic examination reveals dense multiple lobular infiltrations of lymphocytes and eosinophils with central proliferation of vessels throughout the dermis (A: H&E, ×200). The endothelial cells have a hobnail appearance, protruding into the vascular lumen (B) and some endothelial cells have vacuoles in the cytoplasm (C) (B and C: H&E, ×400).

References
1. Wells GC, Whimster IW. Subcutaneous angiolymphoid hyperplasia with eosinophilia. Br J Dermatol. 1969; 81:1–15.

2. Zeitouni NC, Hanna S, Loree TR, Brooks J, Cheney RT. Angiolymphoid hyperplasia with eosinophilia: a classic clinical presentation with histologic features of angiosarcoma. Dermatol Surg. 2002; 28:772–775.

3. Tsuboi H, Fujimura T, Katsuoka K. Angiolymphoid hyperplasia with eosinophilia in the oral mucosa. Br J Dermatol. 2001; 145:365–366.

4. Suzuki H, Hatamochi A, Horie M, Suzuki T, Yamazaki S. A case of angiolymphoid hyperplasia with eosinophilia (ALHE) of the upper lip. J Dermatol. 2005; 32:991–995.

5. Mariatos G, Gorgoulis VG, Laskaris G. Epithelioid hemangioma (angiolymphoid hyperplasia with eosinophilia) in the inner canthus. J Eur Acad Dermatol Venereol. 2001; 15:90–91.

6. Leiferman KM, Peters MS, Gleich GJ. Eosinophils in cutaneous disease. In : Freederg IM, Eisen AZ, Wolff K, editors. Dermatology in general medicine. 6th ed. New York: McGraw-Hill;1999. p. 959–965.
7. Olsen TG, Helwig EB. Angiolymphomatoid hyperplasia with eosinophilia. J Am Acad Dermatol. 1985; 12:781–796.
8. Zerrin-Kameh N, Cooper SM, Dawber RP, Millard P. Angiolymphomatoid hyperplasia with eosinophilia associated with pregnancy. Arch Pathol Lab Med. 2005; 129:1168–1171.
9. Chong WS, Thomas A, Goh CL. Kimura's disease and angiolymphoid hyperplasia with eosinophilia: two disease entities in the same patient. Case report and review of the literature. Int J Dermatol. 2006; 45:139–145.

10. Rohere TE. Angiolymphoid hyperplasia with eosinophilia successfully treated with a long-pulsed turntable dye laser. Dermatol Surg. 2000; 26:211–214.
11. Mok HS, Kwon KS, Chung TA. A case of angiolymphoid hyperplasia with eosinophilia. Korean J Dermatol. 1985; 23:526–530.
12. Park YL, Whang KU, Kim YK. Two cases of epitheloid hemangioma. Angiolymphoid hyperplasia with eosinophilia. Korean J Dermatol. 1992; 30:727–736.
13. Jhun BJ, Lee MH. A case of angiolymphoid hyperplasia with eosinophilia associated with arteriovenous malformation. Korean J Dermatol. 1999; 37:78–81.
14. Shin SS, Lee JB, Lee SC, Won YH. A case of angiolymphoid hyperplasia with eosinophilia. Korean J Dermatol. 2000; 38:836–838.
15. Lee JH, Kim HJ, Lee SY, Lee JS, Whang KY. A case of angiolymphoid hyperplasia with eosinophilia with rapid response to steroid intralesional injection. Korean J Dermatol. 2000; 38:1253–1256.
16. Kim SW, Yoo JM, Oh ST, Jang IG, Cho BK. A case of angiolymphoid hyperplasia with eosinophilia. Korean J Dermatol. 2000; 38:1499–1502.
17. Kim SE, Kim CY, Oh CW. An usual case of angiolymphoid hyperplasia with eosinophilia: chronic ulcerative lesion on the lower lip. Korean J Dermatol. 2001; 39:1181–1183.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download