Abstract
Background
Congenital melanocytic nevi may have various shapes according to the anatomic location. Therefore, it is desirable to apply proper surgical designs to the diverse forms considering the characteristics of the sites as well as the shape and size.
Objective
The purpose of this article is to introduce a new scar-saving flap design for semicircular defects after removing congenital melanocytic nevi without excising additional normal skin.
Methods
In most cases to excise semicircular nevi, normal skin should be excised to prevent dog ear, resulting in the long length of the scar. So we use a new scar-saving flap design by borrowing a partial length from the opposite side.
Results
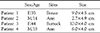
We used this new technique for 4 cases of large semicircular skin defects. In all cases, this method had some advantages from this perspective: (1) it does not require excision of normal adjacent skin to convert a semicircular defect into a crescent shape or to remove dog-ears (2) the final suture line is not much longer than the diameter of the original defect and (3) it makes the removal of a much larger volume possible in one procedure rather than using the classic serial excision technique, which consists of a central elliptical excision within the confines of the nevus. In this way the frequency of procedures and discomfort to the patient can be reduced.
Congenital melanocytic nevi (CMN) are tissue malformations of the neuroectoderm that are mainly comprised of melanocytes1, that are present at birth or appear within the first few months of life2. There are a variety of treatment options for managing CMN according to the size, thickness, location, patient age and risk of developing melanoma1. These reconstructive options include serial excision,serial expansion with a tissue expander, full-thickness or split-thickness skin grafting, dermabrasion, curettage, and Er:YAG laser ablation with a cultured epithelial autograft23.
Serial excision is a surgical technique which is the preferred treatment modality for medium-sized nevi that can be excised in two or three procedures without distorting adjacent structures4. Small to medium-sized CMN are usually round or oval, but may have various shapes, such as a fan or semicircular shape according to the anatomic location. However, to excise such semicircular CMN, normal skin should be excised for appropriate edging. Skin grafts can often result in a dissatisfactory cosmetic outcome, and traditional skin flaps have a limited role.
Therefore, to prevent excising additional normal skin, we developed a new flap design by borrowing a partial length from the opposite side to close a skin defect so as to decrease the length of the scar. In this article, our new flap design, which we named "scar saving flap", is introduced and its effectiveness is evaluated in 4 clinical cases.
The principle of a scar-saving flap for a semicircular skin defect is shown schematically in Fig. 2A The diameter (d) of the semicircle is the straight line from point A through the center C to point B, and the radius (r) is half the diameter. The circumference of a semicircle is (π×d)/2 or πr. Simple interrupted suturing of a semicircular skin defect can make a longer scar because the length of one side is πr and that of the other is 2r. Therefore, we need to find the two points on a curved line that result in two sides of equal length. Assume that points X and Y are on the curved line and are located equal distances from points A and B, respectively. If the arc length from point A to point X is χ, we get the following linear equation:
Moreover, two additional points, a and b, are distance χ from points X and Y.
After these points are identified, the skin is undermined in all directions. When two single-pronged skin hooks holding the tissues at points X and Y are pulled in opposite directions, the skin defect is transformed into a hat shape. At this time, curves XA and YB, which previously formed the semicircle, are folded inward. As the length of arc XY now equals the total length of XABY, there is no problem suturing the hat-shaped wound. After making key stitches at aA and bB, the hat-shaped wound can be sutured using buried, interrupted, dermalsubdermal sutures and a running continuous suture. The final suture line is shown in Fig. 2B
We checked the results of the four patients by photographs and compared the results with previous photographs.
In all patients using our new technique for closing a large semicircular skin defect, we can save the normal adjacent skin because this method dose not need to convert a semicircular defect into a crescent shape or to remove dog-ears. In addition, the final suture line is not much longer than the diameter of the original defect, so we can reduce the entire scar length, resulting in a short broken line scar instead of a long linear scar. Also, it can make the removal of a much larger volume possible in one procedure rather than using the classic serial excision technique, so that the frequency of procedures and discomfort to the patient can be reduced Fig. 1.
Through this new method, we can gain good cosmetic results as well as the treatment effect due to reducing the large volumes. The total patients were also satisfied the results after the operation.
CMN is defined as a melanocytic nevus present at birth or one that appears within the first few months of life2. Usually CMNs are classified according to their size, or the size they are predicted to attain at adulthood. Roughly, one can estimate that a CMN on the head will increase in size by a factor of 1.5 and on the rest of the body by a factor of 3. In adulthood, CMNs that are less than 1.5 cm in greatest diameter are classified as small; those measuring between 1.5 and 19.9 cm are classified as medium; and those that measure at least 20 cm in greatest diameter are classified as large. Very large CMNs measuring at least 50 cm in diameter are sometimes referred to as "giant nevi"1. The optimal management depends on the size of the CMN, the anatomic area, and the histopathologic type. Many treatment options have been postulated for CMN, including dermabrasion6, CO2 laser ablation7, phenol chemical peels8, curettage9, excision and skin grafting10, use of expanded full-thickness skin grafts11, serial excision12, tissue expansion13, and free tissue transfer14, especially depending on the size15.
For the management decisions for patients with CMN, two main problems need to be considered. First, these lesions have the potential for malignant transformation. Second, we should make an effort to optimize the cosmetic and functional outcomes, particularly for giant lesions and those located on the head and neck. Therefore, it is important to find a balance point between decreasing the risk of developing melanoma through prophylactic removal, and achieving acceptable cosmetic results. This balance point will be different for each patient1.
Serial excision is a surgical technique in which successive advancement flaps composed of adjacent normal skin are gradually stretched over a defect created by incremental excision of a lesion. It is not a difficult process to perform and has far fewer potential complications than those of tissue expansion15. Usually it is the preferred treatment modality for medium-sized nevi that can be excised in two or three procedures without distorting adjacent structures. Small to medium-sized CMN are usually round or oval, but may have various shapes, such as a fan or semicircular shape according to the anatomic location Fig. 1. Crescent-shaped skin defects can be sutured using the "rule of halves" to ensure that the tension on closure is evenly distributed and that dog-ears do not form at the ends. In a semicircular defect, however, one side is too much longer than the other to apply the "rule of halves", especially for lesions located on the back, which have minimal redundancy, and arms and shoulder, which have three-dimensional cylindrical shape. In such cases, to excise semicircular CMN, normal skin should be excised for appropriate edging. Skin grafts can often result in a dissatisfactory cosmetic outcome, and traditional skin flaps have a limited role. A few flaps for closing semicircular skin defects have been described in the literature. A small defect is often changed into a crescent form by excising additional normal skin, but this method is impracticable for larger defects.
Therefore, we performed a new scar-saving flap design by borrowing a partial length from the opposite side to close a skin defect without excising additional normal skin. Our new technique for closing a large semicircular skin defect has some advantages from this perspective: (1) it does not require excision of normal adjacent skin to convert a semicircular defect into a crescent shape or to remove dog-ears; (2) the final suture line is not much longer than the diameter of the original defect; and (3) it makes the removal of a much larger volume possible in one procedure rather than using the classic serial excision technique, which consists of a central elliptical excision within the confines of the nevus, so that the frequency of procedures and discomfort to the patient can be reduced. Additionally this method results in short broken line scars instead of long straight scars. When mechanical forces work on scars, the long straight scar is easily strained and fibroblasts are stimulated to result in hypertrophic changes. However, our new flap technique can modify the scar to be a irregular shape, making it less conspicuouscompared with long linear scars and it can disrupt wound contracture with its irregular pattern like W-plasty161718.
We have applied this idea to skin defects in which the two sides are of different lengths. Although we occasionally needed to remove dog-ears, the final outcome was satisfactory. Understanding the concept of borrowing a flap from the opposite side may help reduce the length of the scar, allowing beginners to modify the stereotypic elliptical excision
Figures and Tables
Fig. 1
Fan-shaped or ovalshaped congenital melanocytic nevi were present in 4 patients. Details including the sites of CMN were shown on Table 1. (a,b=patient 1, c,d=patient 2, e,f=patient 3, g,h=patient 4) The designed excision is semicircular. Using this new method, we can reduce the large volume of CMN after the excision and gain short broken line scars rather than long linear scars.

References
1. Tromberg J, Bauer B, Benvenuto-Andrade C, Marghoob AA. Congenital melanocytic nevi needing treatment. Dermatol Ther. 2005; 18:136–150.

2. Whang KK, Kim MJ, Song WK, Cho S. Comparative treatment of giant congenital melanocytic nevi with curettage or Er:YAG laser ablation alone versus with cultured epithelial autografts. Dermatol Surg. 2005; 31:1660–1667.

3. Gosain AK, Santoro TD, Larson DL, Gingrass RP. Giant congenital nevi: a 20-year experience and an algorithm for their management. Plast Reconstr Surg. 2001; 108:622–636.

4. Altchek ED. A technical consideration in the serial excision of a nevus. Plast Reconstr Surg. 1980; 66:849–850.

5. Rhodes AR, Albert LS, Weinstock MA. Congenital nevomelanocytic nevi: proportionate area expansion during infancy and early childhood. J Am Acad Dermatol. 1996; 34:51–62.

6. Rompel R, Moser M, Petres J. Dermabrasion of congenital nevocellular nevi: experience in 215 patients. Dermatol. 1997; 194:261–267.

7. Reynolds N, Kenealy J, Mercer N. Carbon dioxide laser dermabrasion for giant congenital melanocytic nevi. Plast Reconstr Surg. 2003; 111:2209–2214.

8. Hopkins JD, Smith AW, Jackson IT. Adjunctive treatment of congenital pigmented nevi with phenol chemical peel. Plast Reconstr Surg. 2000; 105:1–2.

9. DeRaeve LE, Roseeuw DI. Curettage of giant congenital Melanocytic nevi in neonates. Arch Dermatol. 2002; 138:943–948.

10. Bauer BS, Vicari FA. An approach to excision of congenital giant pigmented nevi in infancy and early childhood. Plast Reconstr Surg. 1988; 82:1012–1021.

11. Bauer BS, Vicari FA, Richard ME, Schwed R. Expended full-thickness skin grafts in children: case selection, planning, and management. Plast Reconstr Surg. 1993; 92:59–69.
13. LoGiudice J, Gosain AK. Pediatric tissue expansion: indications and complications. J Craniofac Surg. 2004; 14:866–872.

14. Margulis A, Bauer BS, Fine NA. Large and giant congenital pigmented nevi of the upper extremity: an algorithm to surgical management. Ann Plast Surg. 2004; 52:158–167.

15. Arneja JS, Gosain AK. Giant congenital melanocytic nevi of the trunk and an algorithm for treatment. J Craniofac Surg. 2005; 16:886–893.

16. Rodgers BJ, Williams EF, Hove CR. W-plasty and geometric broken line closure. Facial Plast Surg. 2001; 17:239–244.

17. Park SS. Scar revision through W-plasty. Fac Plast Clin North Am. 1998; 6:157–161.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download