Abstract
A 28-year-old woman presented with multiple, asymptomatic, erythematous to bluish papules located on the chest. Histopathologically, three round, well defined cystic structures were seen on the upper and lower dermis. The first cyst was milia, the second was apocrine hidrocystoma and the other, largest cyst was an eruptive vellus hair cyst (EVHC). A diagnosis of multiple pilosebaceous cysts combined with apocrine hidrocystoma was made. Since the milia and EVHC originate from the pilosebaceous unit, and the apocrine duct opens to the pilosebaceous orifice, we suggest that they can occur simultaneously in the same unit.
It is well established that each of the three parts of the hair follicle, namely, infundibulum, isthmus and the inferior portion originate from different types of cuteneous cyst1. Especially Milia and EVHC can be considered as a subtype of a multiple pilosebaceous cyst and apocrine hidrocystoma is regarded as an adenomatous cystic proliferation of the apocrine glands. We report a case of two pilosebaceous cysts with apocrine hidrocystoma in one biopsy site.
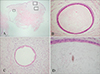
A 28-year-old woman was evaluated for a 6-year history of multiple, asymptomatic papules located on the chest. Clinical examination revealed smooth surfaced, slightly erythematous, bluish papules on the chest (Fig. 1). The patient had noted gradual progression of the lesions over time on the same area. She had no notable past or family history. The histological examination revealed three round, well defined cystic structures on the upper and lower dermis (Fig. 2A). The first cystic lesion was composed of several squamous and granular layers. The cyst was filled with horny material arranged in laminated layers. These findings were consistent with milia (Fig. 2B). The second cyst was lined columnar epithelium and characteristically showed decapitation of cytoplasm of the luminal border, typical of apocrine secretory activity (Fig. 2C). The lower largest cyst was lined stratified squamous cell epithelium and the lumen contained vellus hair shaft, which indicated EVHC (Fig. 2D).
Milia is a small dermal cyst which may arise from the pilosebaceous apparatus or eccrine sweat ducts2. Histologically, the small cysts are lined by several layers of stratified squamous epithelium with central keratinous material, resembling a small epidermal cyst. They may be connected to a vellus hair follicle or eccrine sweat duct3.
EVHC mostly develop as a consequence of occlusion of the infundibulum of vellus hairs with resultant cystic dilatation and retention of keratinous debris and vellus hairs. The characteristic histology is that of a mid-dermal cyst containing laminated keratin and many vellus hairs4.
Although milia and EVHC are distinct from one another, in our case, milia and EVHC were revealed at one biopsy site. Patrizi et al5 suggested that milia and EVHC may represent an early sign of multiple pilosebaceous cystic disease and can be considered as a subtype of a multiple pilosebaceous cyst.
On the one hand, apocrine hidrocystoma is generally thought to arise by cystic dilatation of apocrine glands normally present in the skin. The lining epithelium is composed of uniform cuboidal apocrine cells that demonstrate decapitation secretion and frequently have papillary projections6. In our case, even though the lining epithelium was not totally composed of cuboidal apocrine epithelium, the cyst demonstrated decapitation secretion and was consistent with apocrine hidrocystoma.
The review of correlation between pilosebaceous cyst and apocrine hidrocystoma is limited. But Anderson et al7 presented a combination of apocrine hidrocystoma and epidermal inclusion cyst. He reported four unusual cutaneous cysts in which apocrine epithelium is juxtaposed with keratinizing squamous epithelium and suggested that these cysts arise at the junction of glandular and keratinizing squamous epithelium, accounting for the mixture of lining cells seen histologically. It is also possible that squamous metaplasia within an apocrine hidrocystoma accounts for the mixture of lining epithelium. Finally, he suggested these cysts represent collision lesions in which an apocrine hidrocystoma has fused with an epidermal inclusion cyst.
Takeda et al8 presented cases of hybrid cysts in Japan. The most frequent histological type was the combination of infundibular and trichilemmal cyst and one case was a combination of infundibular cyst and apocrine hidrocystoma. In our case, even though the cysts do not exactly correspond to hybrid cysts, the pilosebaceous cyst and apocrine hidrocystoma were close to each other and showed within one biopsy site.
Pilosebaceous cysts such as milia and EVHC and apocrine hidrocystoma are distinct entities. But these three conditions may show an overlap of histologic features and share many clinical similarities. As we know, most of the apocrine duct opens to the pilosebaceous orifice. At this point in time, we can make an assumption of the possibility of a correlation between pilosebaceous cysts and apocrine hidrocystoma. That is to say, these two entities are not distinct cysts but can be the same unit, namely "piloseboapocrine unit".
In summary, we report a rare case of multiple pilosebaceous cysts with apocrine hidrocystoma which occurred on the same biopsy site and that can be the same piloseboapocrine unit. Further studies, such as multiple biopsy specimens or serial sections from the patient with either milia, EVHC, or apocrine hidrocystoma and more similar cases are required to clarify the pathomechanism of these conditions.
Figures and Tables
Fig. 1
Smooth surfaced, slightly erythematous, bluish papules on the chest; inset: close up view of the papule.

Fig. 2
(A) Histologic examination of the lesion showed round, well defined multiple cystic structures on the upper and lower dermis (H&E, × 12.5). (B) The upper cyst is composed of several layers of squamous and granular layer and filled with horny material arranged in laminated layers (H&E, × 200). (C) The cyst wall is lined by secretory cells showing decapitation secretion (H&E, × 200). (D) The cyst wall is lined by stratified squamous cell epithelium and the lumen contains vellus hair shaft (H&E, × 200).
References
1. Requena L, Sanchez-Yus E. Follicular hybrid cysts. An expanded spectrum. Am J Dermatopathol. 1991; 13:228–233.
2. Iacobelli D, Hashimoto K, Kato I, Ito M, Suzuki Y. Clobetasol induced milia. J Am Acad Dermatol. 1989; 21:215–217.
3. Weedon D. Cysts, sinuses and pits. Skin pathology. 2nd ed. London: Churchill Livingstone;2002. p. 508.
4. Sanchez-Yus E, Aguilar-Martinez A, Cristobal-Gil MC, Urbina-Gonzalez F, Guerra-Rodriguez P. Eruptive vellus hair cyst and steatocystoma multiplex: two related conditions? J Cutan Pathol. 1988; 15:40–42.

5. Patrizi A, Neri I, Guerrini V, Costa AM, Passarini B. Persistent milia, steatocystoma multiplex and eruptive vellus hair cyst: variable expression of multiple pilosebaceous cysts within an affected family. Dermatology. 1998; 196:392–396.

6. Kurban SR, Bhawan J. Cutaneous cysts lined by nonsquamous epithelium. Am J Dermatopathol. 1991; 13:228–233.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download