Abstract
Background
Several new treatments appear to have higher success rates than previous therapies for the treatment of vitiligo, and targeted phototherapy is an alternative that may prove to be time-efficient and an effective therapeutic option for the management of this condition.
Objective
The aim of this study was to evaluate the efficacy of targeted broadband UVB phototherapy for the treatment of localized vitiligo.
Methods
Fifty-three vitiliginous patches on thirty-five patients (16 males, 19 females) were treated using a targeted broadband UVB phototherapy device. Treatment was started at 70% of the minimal erythema dose, and then gradually increased. Lesions were treated twice a week for a maximum of 60 treatment sessions.
Results
Subjects tolerated treatment well. Forty-one of the fifty-three patches (77.4%) achieved repigmentation on ≤75% of the treated areas. Best results were obtained on the face and neck; 20 of the 24 patches (83.3%) concerned achieved ≤75% repigmentation. The least response was on the hands and feet; 3 of 6 patches (50%) showed ≤75% repigmentation. The results were better for focal type than segmental type vitiligo.
Vitiligo is a disorder of cutaneous depigmentation and affects approximately 1% to 2% of the world's population with no predilection for age, sex, or racial background. Vitiliginous patches are often psychologically distressing and in some societies can lead to a loss of social status12. Various treatments have been proposed. Non-surgical modalities considered as first-line therapies, include corticosteroids (oral, topical, and intralesional), oral or topical psoralen plus ultraviolet A (PUVA), and recently, narrowband ultraviolet B (NB-UVB) therapy. Surgical modalities consist of autologous transplantation and include split-thickness epidermal grafting, epidermal blister grafting, and grafting of cultured melanocytes345.
Thanks to its relatively high efficacy and excellent tolerance, NB-UVB is now considered the best treatment for extensive vitiligo678. However, many conventional phototherapies are associated with skin burning and aging when administered long term, and thus the treatment of vitiligo covering less than 10% of the total body area with NB-UVB unnecessarily exposes healthy skin areas.
However, newer targeted phototherapy units allow lesions to be selectively treated. Several reports have shown successful results for 308-nm excimer lasers, which are costly and difficult to maintain, or using light with a wavelength that lies close to that of NB-UVB91011121314. Our purpose in this study was to examine the feasibility of a targeted UVB light source to treat localized vitiligo.
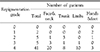
Thirty-five patients (16 men, 19 female), aged from one to sixty-two years (mean age, 22.7 years) were enrolled in this study (Table 1). Twenty-nine patients were affected by focal type vitiligo and six presented with segmental vitiligo. Fifty-three patches of vitiligo in thirty-five patients were treated with the device. All patients showed cutaneous involvement of <10% of total body area. Four of the thirty-five patients had skin photo type III, twenty-eight skin type IV, and the remaining three patients skin type V. Twenty-five patients had no history of previous treatment and the other ten patients had been treated previously using other methods. Subjects with previous treatment were enrolled after a washout period of two weeks for topical steroids, four weeks for any form of phototherapy, and eight weeks for PUVA or immunomodulating agents. Patients with a history of skin cancer, photosensitivity or a photo-mediated disorder, radiotherapy, or immunosuppressive treatments were excluded, as were pregnant or breast-feeding women.
Dua-lightTM (TheraLight Inc., Carlsbad, California) is a high-pressure mercury lamp capable of emitting either UVB or UVA. UVB with a spectral output peaking between 302 and 312 nm and an average weighted erythemal wavelength of 304 nm was used in the present study. The output was initiated using a footswitch and delivered through a fiber-optic hand piece. The final irradiated field had a size of 1.9×1.9 cm.
Treatments were directed at targeted lesions with only a slight overlap of normal surrounding skin. Starting UV doses were 70% of the predetermined minimal erythema dose (MED). MED determinations were performed on vitiligo lesions.
Vitiliginous patches were treated twice a week for a maximum of sixty treatment sessions. UV doses were increased by 10% if no erythema or discomfort occurred, and was applied at a constant level for subsequent sessions when a patient reported very mild erythema or itching. When severe erythema with pain, burning, or blistering was reported, treatment was withheld and after resolution the irradiation dose was decreased by 20%.
Complete patient histories were documented and skin examinations were performed at initial visits. Photographic records were maintained throughout the study from the first visit, throughout therapy, to final follow-up. Improvements (re-pigmentation; defined as percentage reductions in involved skin areas) versus baseline examinations were measured quantitatively using a visual scale by two independent investigators and graded as follows: Grade 0 ≤less than 1% improvement, Grade 1≤1% to 25% improvement, Grade 2=26% to 50% improvement, Grade 3=51% to 75% improvement, Grade 4≥75% improvement.
Results were analyzed using a statistical package (SAS system for Windows V.9.13, SAS Institute Inc, Cary, NC). The Wilcoxon-Rank Sum test was used to determine the effects of variables, such as, type of vitiligo, site, or prior treatment history on final outcome. Fisher's exact test was to determine the effects of variables, such as, clinical site and the presence of side effects on final outcome. The Cochran-Mantel-Haenszel test was used to analyze the relation between skin photo type and final outcome, and Spearmen's Rank Correlation was used to identify the presence of interactions between final outcome and variables, such as, cumulative dose or number of treatment sessions. Statistical significance was defined by a p value of less than 0.05.
Twenty-four of the fifty-three patches were located on the face and neck, twelve on the trunk, eleven on upper or lower limbs, and sixteen on hands and feet.
After ten sessions, five of the fifty-three subjects (9.4%) showed a grade-4 improvement, and after twenty sessions further improvement was observed, with twenty-two of fifty-three subjects (41.5%) showing a grade-4 improvement. After sixty treatment sessions, forty-one of the fifty-three patches (77.4%) showed ≥75% repigmentation (Table 2). The mean number of treatment sessions administered was 44 and the mean cumulative dose was 12.5 J/cm2.
Certain anatomic sites responded better than others (Table 3), and a significant difference was found between anatomic site and final outcome (p=0.0461). In particular, facial and neck areas responded better than hands and feet (p=0.0307); of the 20 patches treated 24 (83.3%) had showed ≥75% repigmentation (Figure 1). Lesions on face and neck tended to respond significantly better than lesions located elsewhere on the body. Repigmentation was mostly peripheral on hands and feet, while on the face and neck additional perifollicular repigmentation was observed. Three subjects had leukotrichia, and in these individuals, repigmentation occurred at macule peripheries and not around affected white hair follicles.
In patients with focal type vitiligo, forty of forty-seven patches (85.1%) showed grade 4 repigmentation, and in patients with segmental vitiligo, one of six patches (16.7%) showed grade 4 repigmentation. Cumulative dose and number of treatment sessions were lower for focal type vitiligo than for segmental vitiligo (p=0.0295, 0.0108), and side effects were more common in patients with the segmental type (p=0.0015).
Among the ten patients with a history of previous treatment, eight had received unsuccessful NB-UVB treatment (seven of these were also administered topical steroid), and two had undergone PUVA and topical steroid treatment. Nine of thirteen patches (69.2%) in ten patients with a history of previous treatment history achieved ≥75% repigmentation. No statistical relation was found between a history of previous treatment and final outcome (p=0.3660), but a statistically significant difference was found between a history of previous treatment and cumulative dose or number of treatment sessions (p=0.0113 and 0.0233, respectively). Patients with a history of previous treatment need more cumulative dose and number of treatment for treatment to be effective.
All patients tolerated the treatment well and side effects were limited to mild erythema and a stinging sensation (9 of 53, 17.0%), and localized bullae in three patches (5.7%). Each of these side effects occurred just once in different patients. Treatment was suspended according to the phototherapy protocol in these cases and resumed when symptoms resolved.
We did not observe any return of depigmentation in treated lesions over six months of follow up after discontinuing treatment.
Vitiligo is a difficult disorder to treat, and most of the currently available treatment modalities are either only slightly effective or associated with significant side effects. Although NB-UVB radiation has been shown to be most efficacious and has a low side-effect profile, reported treatment series required six to twelve months of treatment to achieve optimal results. More recently, several authors have found that microphototherapy or targeted phototherapy offers benefits91011121314151617, which include the rapid onset of repigmentation, good overall response in terms of repigmentation area, and a lower number of treatment sessions than conventional NB-UVB to achieve satisfactory results. It should also be noted that targeted phototherapy can be used to selectively irradiate vitiligo patches without involving neighboring healthy skin.
The number of patients achieving repigmentation at ≥75% in the present study was higher with a lower cumulative dose than other studies. Whether the difference in the output of the source, or differences in treatment protocols and in the distributions of skin types or lesional sites between the studies, contributed to the different response remains to be investigated. In a study by Taneja12 et al, after 40~60 treatments using 308 nm eximer laser, 38.8% (7/18 patches) of the vitiligo patches were repigmented more than 75%. However, for the lesions on the face, all participants (5 of 18 subjects) had grade 4 repigmentation.
Several studies have reported relationships between clinical response and treatment session number or duration111213, and best results were obtained in patients who received more treatment sessions. However, in the present study, Spearmann's Rank Correlation Analysis showed a negative correlation between final outcome and cumulative dose or total session number. In other words, poor responders need more treatment sessions and higher cumulative doses. Different result between the other studies previously noted can be associated with long follow up period without dropout, especially in poor responder group of our study.
Many authors9101112 have consistently reported that response to therapy is highly dependent on lesion location, a finding confirmed by the present study. It is believed that inactive melanocytes in the outer root sheath of the hair follicles are stimulated to proliferate and migrate by the irradiation and cause repigmentation181920. Hair follicle density is also believed to be important, and could explain the poor response of hand skin, which generally has low hair follicle density.
In the present study, it was observed that vitiligo type appears to be related to repigmentation. Patients with focal type vitiligo achieved better final outcomes with lower cumulative doses and treatment session numbers. Unlike NB-UVB phototherapy and PUVA, targeted phototherapy can selectively treat single vitiliginous patches, spare non-affected areas, and achieve clinical improvements faster. And treatment dosage can be adjusted at each focal patch followed by their previous response. When larger areas are treated using targeted phototherapy, two or three subsequent exposures are required. This observation suggests that focal type vitiligo is better treated by targeted phototherapy.
The possibility of a better response by darker skin types to phototherapy has been suggested101214. Hadi10 et al. showed that 53% of patients with skin photo type III or more achieved responses of ≥75%. On the other hand, no patient with skin photo type I and only 15.6% of patients with skin photo type II achieved this level of repigmentation. In the present study, no significant trend was found between final outcome and skin photo type using the Mantel-Haenszel χ2 test (p=.4387). Most of our patients were of skin photo types III~V, and most were of skin type IV. No patient with type I or II was enrolled. A study with a larger cohort and a mix of racial types should be undertaken to obtain more information on this aspect.
In the present study, no relationship was established between final outcome and a previous history of treatment. However, in recalcitrant patients longer treatment sessions and higher cumulative doses were needed. We therefore concluded that these patients are suspected to be more difficult to treat with any modalities.
The results of the present study suggest that targeted broadband UVB phototherapy is a valuable option for the treatment of stable vitiligo with focal type of lesions, especially on the face and neck. This induces more rapid repigmentation than traditional NB-UVB at lower cumulative doses. Moreover, this selective treatment of vitiliginous lesions prevented peri-lesional hyperpigmentation, and this treatment reduces the risks of photoaging and skin cancer by sparing non-affected areas.
Figures and Tables
References
1. Kent G, Al'Abadie M. Psychologic effects of vitiligo;a critical incident analysis. J Am Acad Dermatol. 1996; 35:895–898.
2. Parsad D, Pandhi R, Dogra S, Kanwar AJ, Kumar B. Dermatology Life Quality Index Score in vitiligo and its impact on the treatment outcome. Br J Dermatol. 2003; 148:373–374.

3. Njoo MD, Westerhof W, Bos JD, Bossuyt PM. The development of guidelines for the treatment of vitiligo. Arch Dermatol. 1999; 135:1514–1529.

6. Njoo MD, Spuls PI, Bos JD, Westerhof W, Bossuyt PM. Nonsurgical repigmentation therapies in vitiligo. Arch Dermatol. 1998; 134:1532–1540.

7. Scherschun L, Kim JJ, Lim HW. Narrow-band ultraviolet B is a useful and well tolerated treatment for vitiligo. J Am Acad Dermatol. 2001; 44:999–1003.

8. Njoo MD, Bos JD, Westerhof W. Treatment of generalized vitiligo in children with narrow-band (TL-01) UVB radiation therapy. J Am Acad Dermatol. 2000; 42:245–253.

9. Ostovari N, Passeron T, Zakaria W, Fontas E, Larouy JC, Blot JF. Treatment of vitiligo by 308-nm excimer laser: an evaluation of variables affecting treatment response. Lasers Surg Med. 2004; 35:152–156.

10. Hadi SM, Spencer JM, Lebwohl M. The use of the 308-nm excimer laser for the treatment of vitiligo. Dermatol Surg. 2004; 30:983–986.

11. Esposito M, Soda R, Costanzo A, Chimenti S. Treatment of vitiligo with the 308-nm excimer laser. Clin Exp Dermatol. 2004; 29:133–137.
12. Taneja A, Trehan M, Taylor CR. 308-nm excimer laser for the treatment of localized vitiligo. Int J Dermatol. 2003; 42:658–662.

13. Spencer JM, Nossa R, Ajmeri J. Treatment of vitiligo with the 308-nm excimer laser: a pilot study. J Am Acad Dermatol. 2002; 46:727–731.

14. Leone G, Iacovelli P, Paro Vidolin A, Picardo M. Monochromatic excimer light 308 nm in the treatment of vitiligo: a pilot study. J Eur Acad Dermatol Venerol. 2003; 17:531–537.

15. Lotti TM, Menchini G, Andreassi L. UV-B radiation microphototherapy. An elective treatment for segmental vitiligo. J Eur Dermatol Venerol. 1999; 13:102–108.

16. Menchini G, Tsoureli-Nikita E, Hercogova J. Narrow-band UV-B micro-phototherapy: a new treatment for vitiligo. J Eur Dermatol Venerol. 2003; 17:171–177.

17. Asawanonda P, Charoenlap M, Korkij W. Treatment of localized vitiligo with targeted broadband UVB phototherapy: a pilot study. Photodermatol Photoimmunol Photomed. 2006; 22:133–136.

18. Ongenae K, van Geel N, Naeyaert JM. Evidernce of an autoimmune pathogenesis of vitiligo. Pigment Cell Res. 2003; 90–100.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download