Abstract
Purpose
This study aimed to evaluate the effectiveness of continuous nutritional education and oral mucositis management on the nutritive status of patients who received hematopoietic stem cell transplantation (HSCT).
Methods
After randomly allotting 72 patients who received HSCT to either an experimental group or a control group, intensive and continuous care for preventing malnutrition was conducted in the experimental group while usual routine care was conducted in the control group. The changes of the body scale, blood chemistry profile, oral intake calories, nausea and vomitus, and oral stomatitis scores were measured at three points during their hospitalization using a oral assessment guide and nutrition analysis program: admission, HSCT, and discharge day. The differences between the scores of two groups were analyzed by repeated measures analysis of covariance.
Results
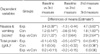
The number of total lymphocytes was significantly improved in the experimental group after transplantation (p<.001). Nausea and vomiting score was significantly decreased in the experimental group during the conditioning regimen (p<.001).
Conclusion
It was found that continuous nutritional education and oral mucositis control is an effective intervention by improving immune condition. Further investigations concerning direct examination of oral intake with controlling the effect of the chemotherapy are needed to ultimately discern the impact of varying oral nutrition patterns during HSCT.
Figures and Tables
References
1. Korean HSCT Nurses Association. Current status of HSCT in Korea. J Korea Stem Cell Transplant Nurs Assoc. 2005. 7:8–13.
2. Psiachou E, Hann IM, Morgan G, Chessells JM. Early deaths in children under going marrow ablative therapy and bone marrow transplantation. Bone Marrow Transplant. 1994. 14:975–980.
3. Cunningham BA, Lenssen P, Aker SN, Gittere KM, Cheney CL, Hutchison MM. Nutritional consideration during marrow transplantaion. Nurs Clin North Am. 1983. 18:585–596.
4. Carol PR. Nutrition support of blood or marrow transplant recipients: how much do we really know? Nutritional Issues In Gastroenterology Series #26. Pract Gastroenterol. 2005. 84–97.
5. Randolph SR. Bone marrow transplant therapy in the home. Caring. 1992. 11:68–71.
6. Koretz RL, Lipman TO, Klein S. AGA Technical Review on Parenteral Nutrition. Gastroenterology. 2001. 121:970–1001.

7. Stern JM, Bruemmer B, Moinpour CM, Sullivan KM, Lenssen P, Aker SN. Impact of a randomized, controlled trial of liberal vs conservative hospital discharge criteria on energy, protein, and fluid intake in patients who received marrow transplants. J Am Diet Assoc. 2000. 100:1015–1022.

8. Smith LH, Besser SG. Dietary restrictions for patients with neutropenia: a survey of institutional practices. Oncol Nurs Forum. 2000. 27:515–520.
9. Bok JN, Kim GS, Choi SE, Song BE. Continuous telephone follow-up for HSCT patients. J Korea Stem Cell Transplant Nurs Assoc. 2003. 5:55–61.7.
10. Rosenberg SW. Oral care of chemotherapy patients. Dent Clin North Am. 1990. 34:239–250.
11. So HS. Assessment of appetite and nutritional status in cancer patients undergoing radiation therapy: a prospective study. J Korean Acad Nurs. 1999. 29:1179–1191.

12. Yang YH, Ghun SJ, Kim CI. The nutritional status of the patients with cancer during the chemotherapies. J Korean Acad Nurs. 2001. 31:978–987.

13. Graham KM, Pecoraro DA, Vontura M, Meyer CC. Reducing the incidence of Stomatitis using a quality assessment and improvement approach. Cancer Nurs. 1993. 16:117–122.

14. Cho GJ. The nutritional evaluation of oncology inpatients receiving chemotherapy [dissertation]. 1993. Daejeon: Chung Nam Univ..
15. Hong JI, Jang UJ. The relationship between the period of engraftment and the nutritional status in patients undergoing allogenic bone marrow transplantation for acute myelogenous leukemia (AML). Korean J Community Nutr. 2002. 7:578–584.
16. Ernest JS, Rosenbaum H, Andrews A, Dollbaum CM, Ignoffo RJ. Clinical practice guidelines for the prevention and treatment of cancer therapy-induced oral and gastrointestinal mucositis. Int Society for Oral Onco. 2004. 100:9 Suppl. 2026–2046. Available at http://www.cancersupportivecare.com/mucositishandout.php.

17. Nutrition Department. Clinical manuals for nutrition part. 2000. 3rd ed. Seoul: Saint Mary's Hospital, Catholic University of Korea.
18. Andersson PR, Lena RH, Ingalill R, Steran R. Testing an oral assessment guide during chemotherapy treatment in a Swedish care setting: a pilot study. J Clin Nurs. 1999. 8:150–158.

19. Shin KY, Song MS. Efficacy progressive muscle relaxation training reducing nausea and vomiting, anxiety and symptom distress of cancer chemotherapy. J Nurs Acad Soc. 1987. 17:195–203.

20. Brodie DA, Eston RG. Body fat estimations by electrical impedance and infrared interaction. Int J Sports Med. 1992. 13:319–325.

21. Kim SH, Shin HS, Im WK. A study on the dietary nutrient intakes and blood profiles of smoking teenage girls living in a rural community in Korea. Korean J Nutr. 2001. 34:338–347.
22. McWhirter JP, Penningtion CR. Incidence and recognition of malnutrition in hospital. BMJ. 1994. 308:945–948.

23. Lipkin EW, Bell S. Assessment of nutritional status: the clinician's perspective. Clin Lab Med. 1993. 13:329–352.

24. Papas AS, Clark RE, Martuscelli G, O'Loughlin KT, Johansen E, Miller KB. A prospective, randomized trial for the prevention of mucositis in patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplantation. 2003. 31:705–712.

25. Lee RD, Nieman DC. Nutritional Assessment. 1996. 2nd ed. Chicago: Mosby Press.
26. Park HJ. Nutritional status of patients undergoing hematopoietic stem cell transplantation [dissertation]. 2000. Seoul: Catholic Univ..
27. Nieweg R, Poelhuis EK, Abraham IL. Nursing care for oral complication ompociated with chemotherapy. Cancer Nurs. 1992. 15:313–321.
28. Yang YH, Lee DS. The relationship of anorexia, nausea, vomiting, oral intake and nutritional status in patients receiving chemotherapy. J Korean Acad Nurs. 2000. 30:720–730.

29. Picou D, Waterlow JC. The effect of malnutrition on the metabolism of plasma albumin. Clin Sci. 1962. 22:459–468.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download