Abstract
Tinnitus is an auditory phantom characterized by the perception of sound without the presence of an external acoustical source. The peripheral auditory system is considered to contribute to the initiation of tinnitus but only explains the severity and distress level to a limited degree. The neuropsychological models of tinnitus have been developed to explain the pathophysiology of tinnitus as a malfunctioning feedforward/feedback signal in the central neural system including the auditory brainstem, limbic system, auditory cortices, and other anatomical features. Functional neuroimaging techniques have been introduced in recent decades and have provided non-invasive tools to assess the working human brain in vivo. Researchers have found these techniques valuable in examining the neural correlates of tinnitus and have been able to not only support the neuropsychological model but to expand it. Though neuroimaging studies on tinnitus only began in 1990s, they have been increasing exponentially in number. In this review, we investigate the current state of functional neuroimaging studies on tinnitus in humans. The characteristics of commonly used functional neuroimaging techniques including positron emission tomography (PET), functional magnetic resonance imaging (fMRI), electroencephalography (EEG) and magnetoencephalography (MEG) are also discussed. We briefly review recent studies on the tinnitus-brain relationship that have used those research tools.
Tinnitus is an auditory phantom characterized by the perception of sound without an external acoustical source [1]. A number of people unknowingly experience tinnitus in their daily lives, since most of the time it appears as a mild and temporary state. But some experience persistent tinnitus that gradually increases in intensity, leading to discomfort in their daily lives and disturbances in carrying out routine tasks for those who suffer from it. Chronic tinnitus occurs in 6-20% of adults, and 1-3% of these patients suffer from severe damage to their quality of life; such patients require treatment from an otologic specialist [23]. An aging population and industrialization in Korea have attributed to the increase in the proportion of the population who are exposed to and affected by increased background noise. This increased environmental noise is believed to be the primary cause for the rising trend in tinnitus patients. In 2014, a large-scale cohort study showed that the prevalence of tinnitus was around 21.4% in adults, of whom 7.3% had severe tinnitus; the chief complaints among these patients were reported to be psychological symptoms such as sleep disturbance and depression [4].
Tinnitus is classified into two sub-types: objective tinnitus and subjective tinnitus. Patients with objective tinnitus perceive a real acoustical source from their body, which is commonly discerned as pulsatile blood flow or as abnormal muscle movements. This means that, although objective tinnitus rarely occurs, given that its cause is known, it can be completely treated [56]. Subjective tinnitus occurs more commonly than objective tinnitus, and only the patients themselves can perceive the sound, making an objective assessment of the condition difficult. It is equally difficult to delineate the cause and the etiology of objective and subjective tinnitus. Since sound perception in patients with subjective tinnitus has no correlation with an external acoustical source, we presume that the central auditory system, rather than the peripheral auditory system, is closely related to the phenomena seen in subjective tinnitus.
The results of many studies that have investigated the etiology of tinnitus support the hypothesis that tinnitus begins as the loss in functions of the peripheral auditory system. Yet, tinnitus was seen to have persisted despite transections of the eighth cranial nerve, which shows that a dysfunctional peripheral auditory system alone cannot be the sole etiological factor. Some have advocated a neurophysiological model of tinnitus that is based on the central auditory system, rather than peripheral models [789]. In animal studies, tinnitus elicited through exposure to ototoxic drugs or to background noise in mice showed an increase in the spontaneous firing rates within the brainstem and the auditory cortex [10]. Auditory afferent information decreases with peripheral hearing loss, which is transmitted through the central auditory system. Conversely, the spontaneous nerve activity increases in the central auditory system, which is believed to induce tinnitus. In a separate study, tonotopic map reorganization of the auditory cortex was reported in a tinnitus-induced animal model [11]. However, one must be cautious because data from animal studies may not be generalizable to humans.
Functional neuroimaging takes an in vivo measurement of CNS function and is widely used in clinical and scientific research. The representative methods of functional imaging are positron emission tomography (PET), functional magnetic resonance imaging (fMRI), electroencephalography (EEG), and magnetoencephalography (MEG). Functional neuroimaging techniques for tinnitus emerged in the late 90s. The approach at the initial stages was delineation of the anatomical regions of the brain that were affected by tinnitus. In recent times, research interests have expanded beyond this to look at clinical markers such as sidedness, duration, and perception of tinnitus and correlation of these clinical markers with neuronal function and connectivity. To interpret studies on tinnitus that have used functional neuroimaging techniques, an understanding of the protocols and relative benefits and limitations of each technique is required. An interpretation should be drawn while taking these points into consideration. In this review, we describe the representative functional neuroimaging techniques used in tinnitus research and evaluate the scientific achievement derived from these tools.
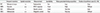
We reviewed the representative functional neuroimaging methods, their relative advantages and disadvantages, and the literature concerning the studies that had been carried out using each technique on tinnitus. The general characteristics of each method have been summarized in Table 1.
Positron emission tomography is used in the clinical context to diagnose diseases, but its use also extends to the research field, being one of the most widely used neuroimaging tools alongside fMRI. In PET, a radioactive tracer is injected intravenously into the bloodstream, and then the regional cerebral blood flow (rCBF) or metabolic changes are measured. The region of the cerebrum responsible for the response to a certain stimulus or action exhibits neuronal hyperactivity and focalized increases in blood flow. The increased blood circulation indicates that energy and oxygen are being supplied to these regions. The injected tracer, according to its physiological characteristic, is metabolized in specific regions of the brain where it is needed, and as the isotope decays, it emits a positron. This positron is combined with an electron circling the nucleus and is annihilated, resulting in the formation of two gamma rays traveling in opposite directions. After detection of the gamma ray through a PET scanner, the transmitted signal is computerized into a 3-dimensional image depicting the in vivo position and distribution of the tracer. This PET 3D image provides spatial information regarding the activated neuronal cells. The commonly used isotopes in PET are C-11, N-13, O-15, and F-18. The physical half-life differs among the isotopes, and its biochemical and physical characteristics may change according to the element with which it forms a compound. Isotopes are selected in light of the purpose and design of each study. The most commonly used radioactive tracer in functional neuroimaging is H215O, which has a relatively short half-life of 123 seconds. Taking a PET scan using an isotope with short half-life allows us to capture the swift response that appears when a patient is concentrating on a certain task. Besides this, 18fluorodeoxyglucose (18F-FDG) is also widely used, but since its half-life is around two hours in the brain, it is often used to investigate brain activity during the resting state.
Limitations of positron emission tomography include the in vivo injection of a radioisotope; this leads to issues of radiation exposure. Other drawbacks of PET are the low spatial resolution (4-8 mm), making it difficult to discriminate specific anatomical locations and a low temporal resolution, which is lower than that of EEG or MEG [12]. However, PET has lower background noise compared to fMRI, making it an appropriate method of choice when performing studies that involve auditory tasks. It also has the advantage that it can be used for studies on patients with cochlear implants who are sensitive to magnetic fields [1314].
A FDG-PET study in 1996 reported that, tinnitus patients showed greater metabolism than controls at the primary auditory cortex (PAC) of the left hemisphere during a resting state. Since the extent of the increase was significantly correlated with the subjective tinnitus distress, it was presumed to be a tinnitus-induced change in the central auditory system [20]. Using the same approach, changes in the auditory cortex were used to calculate the extent of symmetry between the left and right hemispheres. They found that tinnitus patients showed a strong asymmetry, and in agreement with previous studies, the left hemisphere showed a greater metabolism rate than the right hemisphere [2122]. Most studies using H215O as a tracer have measured increased CBF associated with auditory tasks. They have reported that tinnitus patients, compared to controls, showed increased neural activity in the auditory cortex and the limbic areas. Functional connectivity between those two areas also increased; altogether this evidence supports the neurophysiological model of tinnitus [232425]. Recently, repetitive transcranial magnetic stimulation (rTMS) was carried out as a mode of treatment, to determine whether the exaggerated response to sound seen in tinnitus patients can be controlled. Intriguingly, neuronal activity in the auditory cortex was shown to decrease with rTMS.
Functional magnetic resonance imaging is based on the same underlying principle as PET; activity in the brain induces the movement of various metabolites, and this metabolism is calculated indirectly in fMRI. When a neuronal mass is active, the level of oxygen intake into the area increases. To make up for the oxygen consumption, blood flow into the region increases accordingly. In fMRI, the brain region responsible to perform specific functions for a given task shows intensified neuronal activity and an increase in blood flow from its immediate surroundings, leading to a relative accumulation of oxygenated hemoglobin compared to its surroundings, which correlates with an intensified signal on fMRI. This is called a blood oxygen level-dependent (BOLD) signal, which reaches its maximal point in around 6-10 seconds following activation.
Functional MRI is superior in terms of safety, because there is no risk of radioactive exposure, unlike PET, which means that examinations can be performed repeatedly. Among the four imaging techniques described in this review, fMRI has the highest spatial resolution (1.5-3 mm), allowing anatomical positions of the brain to be located and mapped accurately and functional aspects of each brain region to be analyzed individually. A limitation of fMRI is its low temporal resolution compared to EEG and MEG, which measures electrical activity; thus, it is inappropriate for use in assessing very rapid changes in nerve activity in response to a stimulus [1516]. The drawbacks of fMRI are especially evident when it is used to assess brain activity in response to auditory-related tasks, as there are loud scanner noises during image acquisition (the internal coil can cause a noise level of 110-130 dB SPL). This is disadvantageous when test subjects have sustained auditory impairments, and such individuals are most likely to have metallic implants in their body (e.g., cochlear implants, hearing aids). This means that not only safety concerns prevent the use of MRI, but also the noise arising from the device during imaging can have a bearing on the results. When planning an fMRI experiment with auditory tasks, one must take into consideration the noise level and stimulation level.
Most early studies of fMRI investigating tinnitus used auditory stimulation. In 2000, pathologic signal patterns at the contralateral inferior colliculus (IC) were examined while patients perceived tinnitus sounds [26]. Subsequent studies showed that the pathologic patterns associated with tinnitus were not only seen in the IC but also in the medial geniculate body of the thalamus and the auditory cortices of the bilateral hemisphere. Therefore, studies have demonstrated neural evidence of auditory phantom perception, thereby demonstrating the capacity of fMRI to objectively assess tinnitus [1527]. As with the results of studies on PET, those of fMRI have shown increased connectivity in the auditory-limbic system in patients with tinnitus. Not only were there tinnitus-dependent changes in functional connectivity but also changes in the structure of the ventromedial prefrontal cortex [28]. At resting state, studies using fMRI showed that tinnitus-induced emotional changes are associated with the posterior cingulate and the insula regions, and in chronic tinnitus, changes in the default mode network (DMN) were also examined [29]. Individuals with higher tinnitus distress were shown to have a more enhanced fronto-parietal-cingulate network than those with lower distress [30]. As such, the focus of investigation has been directed towards how tinnitus-induced alterations in various regions of the brain or how the changes in connectivity of each brain region correlate to the clinical characteristics of the disease rather than on tinnitus-induced focalized changes in the auditory pathway.
In electroencephalography (EEG), electrical impulses fired from the neuronal mass within the brain are measured at the brain surface. Here, we aim to describe specifically quantitative EEG (QEEG) in greater detail. A standardized, routine method is used to measure brain waves, and the resulting data are modeled by a computer. The modeling of EEG data tended to be restricted to Fourier transformation, but now other methods such as Hilbert transformation, wavelet transformation, independent component analysis (ICA), or source analysis have been used to quantify the data. The reformatted data is superimposed against a cerebral model already embedded in the analysis program to give a localized assessment of brain activity.
Unlike the evoked potentials (EPs) method that measures the evoked brain waves by stimulation, QEEG can measure the electrical signals continuously while the recipient of QEEG is conscious, which means that QEEG data can be obtained relatively easily, compared to other imaging tools. Unlike PET and fMRI, neither bulky measurement devices nor stimulation-delivery instruments are needed. Further, for clinical analysis, since a normative database already exists, standardized analytical techniques can be easily used for statistical analyses. A drawback of QEEG is its relatively low spatial resolution in comparison to those imaging techniques described above. Since the measurements are performed on the surface of the head, neuronal signals may be diminished or distorted while traveling through the skull, and scalp, resulting in a compromised current; this means that assessing deep brain structure may be difficult by this method [1718]. However, a favorable temporal resolution can be obtained through QEEG because it is the electrical signal that is measured.
When tinnitus studies began using QEEG in the early 2000s, the results of these studies confirmed those of previous studies that reported tinnitus-dependent changes in the temporal auditory regions and the temporo-frontal regions of the brain. These studies have again corroborated that not only were neuronal changes observed in the temporal regions but also in the frontal regions. This phenomenon has been explained as the effect of tinnitus-induced depression, which is prevalent in tinnitus patients with high distress [3132]. Some EEG studies have confirmed that an increased gamma frequency range in the temporal regions has been proven by MEG measurement. Therefore, EEG has proved to be sensitive to measuring such a small change that had been presumed to be measurable only using MEG. This comparable sensitivity is an advantage of EEG, given that it is much more accessible than MEG [183334]. In another study, it has been observed that tinnitus patients have a reduced alpha coupling network but an enhanced gamma coupling network [35]. Recent studies have used LORETA analysis, which enhances spatial resolution, to show that different regions were hyperactivated depending on the level of subjective tinnitus distress; it was found that the greater the index of subjective distress, the stronger its association was with alpha and beta signals of the dorsal anterior cingulate cortex of the limbic system [363738]. A recent study that co-analyzed the results of voxel-based morphometry (VBM) and of QEEG found that changes in neuronal signals in the regions of the dorsal cingulate gyrus, the hippocampus, and the parahippocampus were associated with tinnitus-induced distress and with the duration of tinnitus [39]. Recently, novel analytical approaches have been developed to enhance the validity of EEG in order to improve the measurement of signals from sub-cortical sources.
Magnetoencephalography measures neuromagnetic signals using extracorporeal sensors. Since these neuromagnetic signals are extremely weak, superconducting quantum interference devices (SQUIDS) are required for their detection. The neuromagnetic signals, generated by neuronal activity, are quantified in a real-time manner, and an MEG helmet with around 300 SQUIDS bathed in liquid helium and arrayed in its inner surface is worn by the patient during the measurement [19].
Since EEG is a measure of neuronal impulses that have come to the surface after penetrating several layers of tissue, spatial distortion of information may occur. Unlike EEG, MEG is known for its excellent spatial resolution because magnetic fields can penetrate the head without distortion, allowing for a homogenous distribution of magnetic waves. Furthermore, because MEG is completely non-invasive, its measurements are made outside the head independently of its source of magnetic field. No electrical probes are needed, and the non-invasive quality of MEG allows repeated measurements within a short period of time in an individual. Its drawbacks include a high cost as depicted by the fact that only 20 machines exist in the US and only 2 in Korea; this severely limits the accessibility of this approach. It is used clinically for the pre-surgical brain mapping of patients with a brain tumor or epilepsy. In scientific research, MEG has been used to investigate psychological conditions such as dementia and schizophrenia but also clinical conditions related to sensory function (auditory, vision, language disorders, or pain); the literature shows that the topics encompassed by MEG studies are widening [17].
Studies using MEG have showed a markedly decreased level of the slow alpha band and relatively increased delta power in the auditory cortices of tinnitus patients, which is similar to previous EEG studies [40]. The region of hyperactivity differs depending on the sidedness of the tinnitus; unilateral tinnitus induces hyperactivity in the contra-lateral auditory cortex, whereas bilateral tinnitus induces hyperactivity in both hemispheres [41]. Recently, connectivity analysis among brain regions in tinnitus patients was made to explain changes in the context of a global network. The authors of this study found that the gamma band of the global networks, comprising the prefrontal cortex, orbitofrontal cortex, and parieto-occipital region, differed between controls and tinnitus patients. They also found that the changes in connectivity in tinnitus patients were related to their subjective distress [42]. The gamma band of the right auditory cortex was shown to be increased not only in chronic tinnitus patients but also in those who had temporary tinnitus. In addition, the experience of tinnitus itself was shown to lead to the oscillatory alterations of the cerebral cortex [4344].
Here, we reviewed how functional neuroimaging can be used to understand tinnitus-related changes in the human central nervous system. We explored the studies that had been performed using each type of functional neuroimaging method by comparatively analyzing their research protocols and the results. Recent neuroimaging studies on tinnitus are aiming at not only the detection of functional changes but also its therapeutic implications by combining neuroimaging with neuromodulation techniques such as transcranial magnetic stimulation. As much as functional imaging has the potential to have strong clinical and scientific significance, its current significance as a clinical tool remains weak as these are time-consuming and costly. However, future research would increase the accuracy and the objectivity of functional imaging to diagnose tinnitus and assess the treatment outcomes.
Figures and Tables
ACKNOWLEDGMENTS
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean Government (NRF-2013R1A1A3006802).
References
1. Jastreboff PJ. Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res. 1990; 8:221–254.

2. Axelsson A, Ringdahl A. Tinnitus—a study of its prevalence and characteristics. Br J Audiol. 1989; 23:53–62.

3. Shargorodsky J, Curhan GC, Farwell WR. Prevalence and characteristics of tinnitus among US adults. Am J Med. 2010; 123:711–718.

4. Park RJ, Moon JD. Prevalence and risk factors of tinnitus: the Korean National Health and Nutrition Examination Survey 2010-2011, a cross-sectional study. Clin Otolaryngol. 2014; 39:89–94.

7. House JW, Brackman DE. Tinnitus: surgical treatment. Ciba Found Symp. 1981; 85:204–216.
8. Brackmann DE, Barrs DM. Assessing recovery of facial function following acoustic neuroma surgery. Otolaryngol Head Neck Surg. 1984; 92:88–93.

9. Rachakonda T, Shimony JS, Coalson RS, Lieu JEC. Diffusion tensor imaging in children with unilateral hearing loss: a pilot study. Front Syst Neurosci. 2013; 8:87–87.

10. Noreña AJ, Eggermont JJ. Changes in spontaneous neural activity immediately after an acoustic trauma: implications for neural correlates of tinnitus. Hear Res. 2003; 183:137–153.

12. Weber B, Späth N, Wyss M, Wild D. Quantitative cerebral blood flow measurements in the rat using a beta-probe and H215O. J Cereb Blood Flow Metab. 2003; 23:1455–1460.

13. Johnsrude IS, Giraud AL, Frackowiak RS. Functional imaging of the auditory system: the use of positron emission tomography. Audiol Neurootol. 2002; 7:251–276.

14. Lee HJ, Giraud AL, Kang E, Oh SH, Kang H, Kim CS, et al. Cortical Activity at Rest Predicts Cochlear Implantation Outcome. Cerebral Cortex. 2006; 17:909–917.

15. Lanting CP, de Kleine E, Bartels H, van Dijk P. Functional imaging of unilateral tinnitus using fMRI. Acta Otolaryngol. 2008; 128:415–421.

16. Lanting CP. Functional Magnetic Resonance Imaging of Tinnitus. 2010. 5:p. 1–176.
17. Lystad RP, Pollard H. Functional neuroimaging: a brief overview and feasibility for use in chiropractic research. J Can Chiropr Assoc. 2009; 53:59–72.
18. Viirre ES. Quantitative electroencephalography for tinnitus--a means for data collection, analysis, and translation. Int Tinnitus J. 2009; 15:149–153.
19. Hansen P, Kringelbach M, Salmelin R. MEG: an introduction to methods. 2010.
20. Arnold W, Bartenstein P, Oestreicher E, Römer W, Schwaiger M. Focal Metabolic Activation in the Predominant Left Auditory Cortex in Patients Suffering from Tinnitus: a PET Study with [18F]Deoxyglucose. ORL J Otorhinolaryngol Relat Spec. 1996; 58:195–199.

21. Langguth B, Eichhammer P, Kreutzer A, Maenner P, Marienhagen J, Kleinjung T, et al. The impact of auditory cortex activity on characterizing and treating patients with chronic tinnitus--first results from a PET study. Acta Otolaryngol Suppl. 2006; 56:84–88.
22. Wang H, Tian J, Yin D, Jiang S, Yang W, Han D, et al. Regional glucose metabolic increases in left auditory cortex in tinnitus patients: a preliminary study with positron emission tomography. Chin Med J. 2001; 114:848–851.
23. Lockwood AH, Salvi RJ, Coad ML, Towsley ML, Wack DS, Murphy BW. The functional neuroanatomy of tinnitus: evidence for limbic system links and neural plasticity. Neurology. 1998; 50:114–120.
24. Giraud AL, Chery-Croze S, Fischer G, Fischer C, Vighetto A, Grégoire MC, et al. A selective imaging of tinnitus. Neuroreport. 1999; 18:1.

25. Plewnia C, Reimold M, Najib A, Brehm B, Reischl G, Plontke SK, et al. Dose-dependent attenuation of auditory phantom perception (tinnitus) by PET-guided repetitive transcranial magnetic stimulation. Hum Brain Mapp. 2007; 28:238–246.

26. Melcher JR, Sigalovsky IS, Guinan JJ, Levine RA. Lateralized tinnitus studied with functional magnetic resonance imaging: abnormal inferior colliculus activation. J Neurophysiol. 2000; 83:1058–1072.

27. Smits M, Kovacs S, De Ridder D, Peeters RR, Van Hecke P, Sunaert S. Lateralization of functional magnetic resonance imaging (fMRI) activation in the auditory pathway of patients with lateralized tinnitus. Neuroradiology. 2007; 49:669–679.

28. Leaver AM, Renier L, Chevillet MA, Morgan S, Kim HJ, Rauschecker JP. Dysregulation of limbic and auditory networks in tinnitus. Neuron. 2011; 69:33–43.

29. Carpenter-Thompson JR, Schmidt SA, Husain FT. Neural Plasticity of Mild Tinnitus: an fMRI Investigation Comparing Those Recently Diagnosed with Tinnitus to Those That Had Tinnitus for a Long Period of Time. Neural Plast. 2015; 1:1–11.

30. Golm D, Schmidt-Samoa C, Dechent P, Kröner-Herwig B. Neural correlates of tinnitus related distress: an fMRI-study. Hear Res. 2013; 295:87–99.

31. Shulman A, Avitable MJ, Goldstein B. Quantitative electroencephalography power analysis in subjective idiopathic tinnitus patients: a clinical paradigm shift in the understanding of tinnitus, an electrophysiological correlate. Int Tinnitus J. 2006; 12:121–131.
32. Shulman A, Goldstein B. Quantitative electroencephalography: preliminary report--tinnitus. Int Tinnitus J. 2002; 8:77–86.
33. Ashton H, Reid K, Marsh R, Johnson I, Alter K, Griffiths T. High frequency localised "hot spots" in temporal lobes of patients with intractable tinnitus: a quantitative electroencephalographic (QEEG) study. Neurosci Lett. 2007; 426:23–28.

34. Weisz N, Müller S, Schlee W. The neural code of auditory phantom perception. J Neurosci. 2007; 27:1479–1484.

35. Schlee W, Hartmann T, Langguth B, Weisz N. Abnormal resting-state cortical coupling in chronic tinnitus. BMC Neurosci. 2009; 10:11.

36. Vanneste S, Plazier M, Loo der EV, de Heyning PV, Congedo M, De Ridder D. The neural correlates of tinnitus-related distress. Neuroimage. 2010; 52:470–480.

37. Song JJ, De Ridder D, Schlee W, Van de Heyning P. "Distressed aging": the differences in brain activity between early-and late-onset tinnitus. Neurobiol Aging. 2013; 34:1853–1863.

38. Song JJ, Vanneste S, Schlee W. Onset-related differences in neural substrates of tinnitus-related distress: the anterior cingulate cortex in late-onset tinnitus, and the frontal cortex in early-onset tinnitus. Brain Struct Funct. 2015; 220:571–584.

39. Vanneste S, Van De Heyning P, De Ridder D. Tinnitus: a large VBM-EEG correlational study. PLoS ONE. 2015; 10:e0115122.

40. Weisz N, Moratti S, Meinzer M, Dohrmann K, Elbert T. Tinnitus perception and distress is related to abnormal spontaneous brain activity as measured by magnetoencephalography. PLoS Med. 2005; 2:e153.

41. Seidman MD, Ridder DD, Elisevich K, Bowyer SM, Darrat I, Dria J, et al. Direct Electrical Stimulation of Heschl's Gyrus for Tinnitus Treatment. Laryngoscope. 2008; 118:491–500.

42. Schlee W, Mueller N, Hartmann T, Keil J, Lorenz I, Weisz N. Mapping cortical hubs in tinnitus. BMC Biol. 2009; 7:80.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download