Abstract
In the early postnatal period, prematurely born infants, especially those born at the earliest limits of viability, face a nutritional crisis. A lack of essential nutrients may result in substantial developmental morbidity. In particular, because this period is crucial to proper neurodevelopment, a central concern must be providing essential nutrition for proper neurodevelopment, and the prevention of long-term neuro-deficits. Therefore, providing appropriate nutrition for growth and development is one of the most essential concerns in the care of preterm infants. The optimal goal for providing nutrition in the preterm infant is to achieve a postnatal growth rate approximating that of the normal fetus at the same gestational age. However, extra-uterine growth restriction develops during the course of care for most very low birth weight infants admitted to the neonatal intensive care unit. Herein, the optimal nutrient requirements and most recently recommended total parenteral and enteral feeding strategies are reviewed to provide neonatal clinicians with current guidelines for nutritional care that can improve neurodevelopmental outcomes in preterm infants during and after treatment in the neonatal intensive care unit.
Figures and Tables
Table 1
Fluid and Macronutrient Guidelines for Parenterally Fed Premature Infants by the European Society of Paediatric Gastroenterology, Hepatology and Nutrition and European Society for Clinical Nutrition and Metabolism in 2005

Table 2
Fluid and Macronutrient Guidelines for Enterally Fed Premature Infants by ESPGHAN in 2010
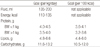
Modified from Ref. 37 with permission from Wolters Kluwer Health
References
2. American Academy of Pediatrics Committee on Nutrition. Nutritional needs of low-birth-weight infants. Pediatrics. 1985. 75:976–986.
3. Denne SC, Poindexter BB. Evidence supporting early nutritional support with parenteral amino acid infusion. Semin Perinatol. 2007. 31:56–60.

4. Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, et al. Trends in neonatal morbidity and mortality for very low birth weight infants. Am J Obstet Gynecol. 2007. 196:147.e1–147.e8.
5. Stephens BE, Walden RV, Gargus RA, Tucker R, McKinley L, Mance M, et al. First-week protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics. 2009. 123:1337–1343.

6. Koletzko B, Goulet O, Hunt J, Krohn K, Shamir R. 1. Guidelines on Paediatric Parenteral Nutrition of the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) and the European Society for Clinical Nutrition and Metabolism (ESPEN), Supported by the European Society of Paediatric Research (ESPR). J Pediatr Gastroenterol Nutr. 2005. 41:Suppl 2. S1–S87.
7. Rivera A Jr, Bell EF, Bier DM. Effect of intravenous amino acids on protein metabolism of preterm infants during the first three days of life. Pediatr Res. 1993. 33:106–111.

8. Thureen PJ, Anderson AH, Baron KA, Melara DL, Hay WW Jr, Fennessey PV. Protein balance in the first week of life in ventilated neonates receiving parenteral nutrition. Am J Clin Nutr. 1998. 68:1128–1135.

9. Thureen PJ, Melara D, Fennessey PV, Hay WW Jr. Effect of low versus high intravenous amino acid intake on very low birth weight infants in the early neonatal period. Pediatr Res. 2003. 53:24–32.

10. Ridout E, Melara D, Rottinghaus S, Thureen PJ. Blood urea nitrogen concentration as a marker of amino-acid intolerance in neonates with birthweight less than 1250 g. J Perinatol. 2005. 25:130–133.

11. Roberts SA, Ball RO, Filler RM, Moore AM, Pencharz PB. Phenylalanine and tyrosine metabolism in neonates receiving parenteral nutrition differing in pattern of amino acids. Pediatr Res. 1998. 44:907–914.

12. Wykes LJ, House JD, Ball RO, Pencharz PB. Aromatic amino acid metabolism of neonatal piglets receiving TPN: effect of tyrosine precursors. Am J Physiol. 1994. 267:E672–E679.

13. Zlotkin SH, Bryan MH, Anderson GH. Cysteine supplementation to cysteine-free intravenous feeding regimens in newborn infants. Am J Clin Nutr. 1981. 34:914–923.

14. Parimi PS, Kalhan SC. Glutamine supplementation in the newborn infant. Semin Fetal Neonatal Med. 2007. 12:19–25.

15. Denne SC, Kalhan SC. Glucose carbon recycling and oxidation in human newborns. Am J Physiol. 1986. 251:E71–E77.

16. Hertz DE, Karn CA, Liu YM, Liechty EA, Denne SC. Intravenous glucose suppresses glucose production but not proteolysis in extremely premature newborns. J Clin Invest. 1993. 92:1752–1758.

17. Cowett RM, Farrag HM. Selected principles of perinatal-neonatal glucose metabolism. Semin Neonatol. 2004. 9:37–47.

19. Stonestreet BS, Rubin L, Pollak A, Cowett RM, Oh W. Renal functions of low birth weight infants with hyperglycemia and glucosuria produced by glucose infusions. Pediatrics. 1980. 66:561–567.

20. Hays SP, Smith EO, Sunehag AL. Hyperglycemia is a risk factor for early death and morbidity in extremely low birth-weight infants. Pediatrics. 2006. 118:1811–1818.

21. Kairamkonda VR, Khashu M. Controversies in the management of hyperglycemia in the ELBW infant. Indian Pediatr. 2008. 45:29–38.
22. Binder ND, Raschko PK, Benda GI, Reynolds JW. Insulin infusion with parenteral nutrition in extremely low birth weight infants with hyperglycemia. J Pediatr. 1989. 114:273–280.

23. Ditzenberger GR, Collins SD, Binder N. Continuous insulin intravenous infusion therapy for VLBW infants. J Perinat Neonatal Nurs. 1999. 13:70–82.

24. Poindexter BB, Karn CA, Denne SC. Exogenous insulin reduces proteolysis and protein synthesis in extremely low birth weight infants. J Pediatr. 1998. 132:948–953.

25. Beardsall K, Vanhaesebrouck S, Ogilvy-Stuart AL, Vanhole C, Palmer CR, van Weissenbruch M, et al. Early insulin therapy in very-low-birth-weight infants. N Engl J Med. 2008. 359:1873–1884.

26. Sinclair JC, Bottino M, Cowett RM. Interventions for prevention of neonatal hyperglycemia in very low birth weight infants. Cochrane Database Syst Rev. 2011. CD007615.

27. Carlson SE. Docosahexaenoic acid and arachidonic acid in infant development. Semin Neonatol. 2001. 6:437–449.

28. Carlson SE, Werkman SH, Tolley EA. Effect of long-chain n-3 fatty acid supplementation on visual acuity and growth of preterm infants with and without bronchopulmonary dysplasia. Am J Clin Nutr. 1996. 63:687–697.

29. Carlson SE, Werkman SH, Rhodes PG, Tolley EA. Visual-acuity development in healthy preterm infants: effect of marine-oil supplementation. Am J Clin Nutr. 1993. 58:35–42.

30. Sunehag AL. The role of parenteral lipids in supporting gluconeogenesis in very premature infants. Pediatr Res. 2003. 54:480–486.

31. Simmer K, Rao SC. Early introduction of lipids to parenterally-fed preterm infants. Cochrane Database Syst Rev. 2005. CD005256.

33. Simon JN. Gastrointestinal function and its ontogeny: how should we feed the preterm infant? Semin Neonatol. 1996. 1:59–66.

34. Hay WW Jr. Nutritional needs of the extremely low-birth-weight infant? Semin Perinatol. 1991. 15:482–492.
35. Stoddart RW, Widdowson EM. Changes in the organs of pigs in response to feeding for the first 24 h after birth. III. Fluorescence histochemistry of the carbohydrates of the intestine. Biol Neonate. 1976. 29:18–27.

36. Heird WC, Schwarz SM, Hansen IH. Colostrum-induced enteric mucosal growth in beagle puppies. Pediatr Res. 1984. 18:512–515.

37. Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T, et al. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010. 50:85–91.

38. Lucas A, Bloom SR, Aynsley-Green A. Gut hormones and 'minimal enteral feeding'. Acta Paediatr Scand. 1986. 75:719–723.

39. Tyson JE, Kennedy KA. Minimal enteral nutrition for promoting feeding tolerance and preventing morbidity in parenterally fed infants. Cochrane Database Syst Rev. 2000. CD000504.
40. Tyson JE, Kennedy KA. Trophic feedings for parenterally fed infants. Cochrane Database Syst Rev. 2005. CD000504.

41. Jeon GW, Park SE, Choi CW, Hwang JH, Chang YS, Park WS. The effects of early enteral feeding in extremely low birth-weight infants. Korean J Pediatr. 2005. 48:711–715.
42. Lee HY, Lee GY, Kim MJ, Jeon GW, Shim JW, Chang YS, et al. The effect of early enteral trophic feeding within 24 hours after birth in extremely low birth weight infants of 26 weeks and less, and birth weight below 1,000 g. J Korean Soc Neonatol. 2007. 14:59–65.
43. Kosloske AM. Breast milk decreases the risk of neonatal necrotizing enterocolitis. Adv Nutr Res. 2001. 10:123–137.
45. Lucas A, Fewtrell MS, Morley R, Lucas PJ, Baker BA, Lister G, et al. Randomized outcome trial of human milk fortification and developmental outcome in preterm infants. Am J Clin Nutr. 1996. 64:142–151.

46. Corvaglia L, Aceti A, Paoletti V, Mariani E, Patrono D, Ancora G, et al. Standard fortification of preterm human milk fails to meet recommended protein intake: bedside evaluation by Near-Infrared-Reflectance-Analysis. Early Hum Dev. 2010. 86:237–240.

47. Lawrence RA. Breastfeeding in the premature infant. J Arab Neonatal Forum. 2005. 2:43–49.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download