Abstract
Healthcare personnel (HCP) face a wide range of occupational hazards, including needle-stick injuries, back injuries, latex allergy, violence, and stress. In particular, occupational exposures to infectious agents, such as human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV),or tuberculosis, are devastating to the victims. The World Health Organization (WHO) estimates the global burden of disease from occupational exposure to be 40% of hepatitis B and C virus infections and 2.5% of the HIV infections among HCP. Infectious disease cases for which compensation is given by the Korean Occupational Safety and Health Agency are increasing, and tuberculosis is the most common infectious disease compensated by KOSHA for HCP in Korea. While viral respiratory infections are common in health care settings, systematic surveillance has not been established yet in Korea. Infection control programs for HCP, such as engineering control in medical facilities, immunization, post exposure prophylaxis, and use of personal protective equipment need to be improved in Korea. This article describes the epidemiologic characteristics of occupational infectious diseases among HCP in Korea, especially focusing on needle-stick injuries and airborne infections. Also brief commentary is offered concerning effective measures for the control and prevention of occupational infectious disease transmission among HCP.
Figures and Tables
 | Fig. 1Proportion of infectious diseases among 307 healthcare personnel compensated by the Korea Labor Welfare Corporation between 1998 and 2004. *Epidemic keratoconjunctivitis (2), Cellulitis (2), Meningitis (1), Encephalitis (1), Purulent otitis media (1), Epidemic hemorrhagic fever (1), Septicemia with pseudomonas (1), Poststreptococcal glomerulonephritis (1), Choroiditis (1). |
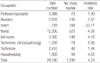
 | Fig. 2Occupational groups of healthcare personnel exposed to infectious diseases; a total of 307 cases compensated by the Korea Labor Welfare Corporation between 1998 and 2004. |
References
1. Korean Medical Association [Internet]. c2009. cited 2011 May 22. Seoul (KR): Korean Medical Association;Available from: http://www.kma.org/contents/board/mboard.asp?exec=view&strBoardID=report&intSeq=3449.
2. Wilburn SQ, Eijkemans G. Preventing needlestick injuries among healthcare workers: a WHO-ICN collaboration. Int J Occup Environ Health. 2004. 10:451–456.

3. Occupational Safety and Health Research Institute. Evaluation of infectious disease in health care workers, focusing on management control of occupational safety and health system. 2006. Incheon: OSHRI;Report No. 2005-115-594: 4.
4. Ahn YS, Lim HS. Occupational infectious diseases among Korean health care workers compensated with industrial accident compensation insurance from 1998 to 2004. Ind Health. 2008. 46:448–454.

6. Panlilio AL, Orelien JG, Srivastava PU, Jagger J, Cohn RD, Cardo DM. Estimate of the annual number of percutaneous injuries among hospital-based healthcare workers in the United States, 1997-1998. Infect Control Hosp Epidemiol. 2004. 25:556–562.

7. International Healthcare Worker Safety Center. EPINet report: 2007 percutaneous injury rates. 2009. Charlottesville (VA): IHWSC;1–4.
8. Occupational Safety and Health Resarch Institute. Development of needle-stick injury surveillance system for health care personnel. 2010. Incheon: OSHRI;Report No. 2010-OSHRI-1102: 17.
9. Seo JM, Jeong IS. Post-exposure reporting of needlestick and sharp-object injuries among nurses. Korean J Nosocomial Infect Control. 2010. 15:26–35.
10. Centers for Disease Control and Prevention. Workbook for designing, implementing, and evaluating a sharps injury prevention program [Internet]. c2010. cited 2011 Jun 2. Atlanta (GA): CDC;Available from: http://www.cdc.gov/sharpssafety/pdf/sharpsworkbook_2008.pdf.
11. Park MR, Kim JE, Park ES, Choi JS, Jung SY, Song YG, et al. A Multicenter Descriptive Study of Bloodborne Exposures among Health Care Workers in Seoul and Gyeonggi-Do. Korean J Nosocomial Infect Control. 2003. 8:35–45.
12. Oh HS, Choe KW. Descriptive Study of Reported Bloodborne Exposures in Health Care Workers in a University Hospital. Korean J Nosocomial Infect Control. 2002. 7:51–64.
13. Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HBV, HCV, and HIV and Recommendations for Postexposure Prophylaxis. MMWR Recomm Rep. 2001. 50:1–52.
14. Beltrami EM, Williams IT, Shapiro CN, Chamberland ME. Risk and management of blood-borne infections in health care workers. Clin Microbiol Rev. 2000. 13:385–407.

15. Jeong S, Yim HW, Bae SH, Lee WC. Changes of hepatitis B surface antigen seroprevalence in Korea, 1998-2005. Korean J Epidemiol. 2008. 30:119–127.

16. Pruss-Ustun A, Rapiti E, Hutin Y. Sharps injuries: global burden of disease from sharps injuries to healthcare workers. 2003. Geneva, Switzerland: World Health Organization;17–19. Report No. WHO Environmental Burden of Disease Series, No. 3.
17. Kwon JH, Bae SH. Current status and clinical course of hepatitis C virus in Korea. Korean J Gastroenterol. 2008. 51:360–367.
18. Alter MJ, Kruszon-Moran D, Nainan OV, McQuillan GM, Gao F, Moyer LA, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999. 341:556–562.

19. Centers for Disease Control and Prevention. Recommendations for follow-up of health-care workers after occupational exposure to hepatitis C virus. MMWR Morb Mortal Wkly Rep. 1997. 46:603–606.
20. Choi JY. Prevention of HIV infection in health care setting. Korean J Nosocomial Infect Control. 2008. 13:64–68.
21. Choi SM, Lee JY, Oh HS, Park ES, Kim SW, Kim YR, et al. Servey of HIV exposure and postexposure prophylaxis among health care workers in Korea. Korean J Nosocomial Infect Control. 2002. 7:65–73.
22. Korea National Tuberculosis Association. Tuberculosis [Internet]. c2011. cited 2011 Jun 3. Seoul: KNTA;Available from: https://www.knta.or.kr/inform/sub_03_01.asp.
23. Jo KW, Woo JH, Hong Y, Choi CM, Oh YM, Lee SD, et al. Incidence of tuberculosis among health care workers at a private university hospital in South Korea. Int J Tuberc Lung Dis. 2008. 12:436–440.
24. Centers for Disease Control and Prevention. Public health core functions--Alabama, Maryland, Mississippi, New Jersey, South Carolina, and Wisconsin, 1993. MMWR Morb Mortal Wkly Rep. 1994. 43:13–15.
25. Choi HJ. Recommended immunization for the healthcare workers in Korea. Korean J Nosocomial Infect Control. 2008. 13:7–15.
26. Kweon OM, Lee DS, Park ES, Kim CO, Han SH, Kim KH, et al. Management of healthcare workers and patients on exposure to pandemic influenza A (H1N1 2009) virus in a hospital. Korean J Nosocomial Infect Control. 2010. 15:96–102.
27. Bernstein HH, Starke JR. Policy statement--recommendation for mandatory influenza immunization of all health care personnel. Pediatrics. 2010. 126:809–815.

28. Cheong HJ, Sohn JW, Choi SJ, Eom JS, Woo HJ, Chun BC, et al. Factors influencing decision regarding influenza vaccination: a survey of healthcare workers in one hospital. Infect Chemother. 2004. 36:213–218.
29. Cha KS, Yoo SY, Kim KM, Wie SH, Shin WS. Healthcare workers' knowledge and attitude about influenza vaccination at the University hospital. Korean J Nosocomial Infect Control. 2005. 10:87–95.
30. Hardelid P, Fleming DM, McMenamin J, Andrews N, Robertson C, SebastianPillai P, et al. Effectiveness of pandemic and seasonal influenza vaccine in preventing pandemic influenza A(H1N1)2009 infection in England and Scotland 2009-2010. Euro Surveill. 2011. 16:pii: 19763. Available online:http://www.eurosur veillance.org/ViewArticle.aspx?ArticleId=19763.

31. Nakano T, Ihara T, Kamiya H. Measles outbreak among non-immunized children in a Japanese hospital. Scand J Infect Dis. 2002. 34:426–429.

32. Park HC, Park EY, Cho SH, Choi YJ, Ki HK, Jung YH, et al. Measles outbreak among institutional infants after hospital infection. Korean J Epidemiol. 2001. 23:50–58.
33. Lee J, Song JY, Seo YB, Kim SR, Cheong HJ, Kim WJ. Measles outbreaks and infection control in a tertiary hospital. Korean J Nosocomial Infect Control. 2008. 13:24–31.
34. Lee J, Song JY, Seo YB, Kim SR, Cheong HJ, Kim WJ. Measles outbreaks and infection control in a tertiary hospital. Korean J Nosocomial Infect Control. 2008. 13:24–31.
35. Shin HS, Oh HS, Kim SM, Kim NJ, Choi HJ, Oh MD, et al. Prevalence of measles, rubella and varicella-zoster antibodies in hospital personnel. Korean J Infect Dis. 1997. 29:29–32.
36. De Serres G, Shadmani R, Duval B, Boulianne N, Dery P, DouvilleFradet M, et al. Morbidity of pertussis in adolescents and adults. J Infect Dis. 2000. 182:174–179.

37. The Korean Society of Infectious Diseases. Vaccination for adults [Internet]. c2007. cited 2011 Jun 2. Seoul: The Korean Society of Infectious Diseases;Available from:http://www.ksid.or.kr/data/sub01.html.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download