Abstract
Objective
We compared the shear bond strength (SBS) of lingual retainers bonded to bovine enamel with three different resins using direct and indirect methods.
Methods
Both ends of pre-fabricated twisted ligature wires were bonded to bovine enamel surfaces using Light-Core, Tetric N-Flow, or Transbond XT. Phosphoric acid-etched enamel surfaces were primed with One-Step prior to bonding with Light-Core or Tetric N-Flow. Transbond XT primer was used prior to bonding with Transbond XT. After 24 hours in water at 37℃, we performed SBS tests on the samples. We also assigned adhesive remnant index (ARI) scores after debonding and predicted the clinical performance of materials and bonding techniques from Weibull analyses.
Results
Direct bonding produced significantly higher SBS values than indirect bonding for all materials. The SBS for Light-Core was significantly higher than that for Tetric N-Flow, and there was no significant difference between the direct bonding SBS of Transbond XT and that of Light-Core. Weibull analysis indicated Light-Core performed better than other indirectly bonded resins.
Relapses following orthodontic treatment are unpredictable.1,2 Research into these relapses has frequently centered on the lower anterior teeth segment, where relapses most often occur.3 While lingual bonded retainers are considered to be the most suitable method of retention, the effectiveness of this method is still controversial.4 Recent research suggests that long-term retention of the lower anterior segment may be necessary in order to prevent or reduce unwanted post-treatment changes.5
Fixed lingual multistrand retainers have long been available as a method of orthodontic retention6 and a number of different designs and techniques for bonding having been suggested.7,8 This type of retainer allows physiologic tooth movement while maintaining tooth alignment.6
There are two primary approaches to bonding fixed lingual retainers: direct bonding and indirect bonding. Compared with direct bonding, indirect bonding of these retainers requires less chair time, etched surfaces are less likely to become contaminated, and are easier to position correctly.9 The method, however, also has certain disadvantages, in that it is more technique-sensitive, requiring more laboratory time to fabricate the appliance than direct bonding.9 Indirect bonding also incurs some risk of adhesive leakage into gingival embrasures that results in oral hygiene problems.10
Flowable composites are low-viscosity restorative materials, differing from conventional resin composites in their filler load and resin content.11 Recently, some researchers have suggested flowable composites as bonding agents for lingual retainers.12 Because they are not very strong, using them for this purpose may result in an increased risk of breakage. Light-cured core build-up composites,13 however, are heavily filled hybrid composites that are much stronger and more fracture-resistant than flowable composites.14 These characteristics may make light-cured core build-up composites a viable option for bonding fixed lingual retainers, as these retainers require long-lasting high bonding strength.
We therefore compared the shear bond strength (SBS) of lingual retainers bonded to bovine enamel with three different resins using both direct and indirect methods. After debonding, teeth were assessed according to the adhesive remnant index (ARI). Clinical performance of the materials and bonding techniques were predicted using Weibull analyses of the SBS data.
Extracted bovine teeth were disinfected in 0.5% chloramines, stored in distilled water until use, and polished with 600-grit silicon carbide paper to expose a fresh and flat enamel surface. The teeth were washed with distilled water, and the prepared tooth specimens were embedded in an autopolymerizing resin. Embedded specimens were randomly divided into six groups, with 15 teeth in each group. Each group was assigned to a different combination of the 3 bonding materials and 2 bonding methods (direct or indirect bonding) under investigation. The 3 bonding materials tested were as follows: Light-Core (Bisco, Schaumburg, IL, USA), Tetric N-Flow (Ivoclar Vivadent, Schaan, Liechten-Liechtenstein), and Transbond XT Adhesive paste (3M Unitek, Monrovia, CA, USA). Wire retainers were pre-fabricated by twisting three strands of 0.009-inch ligature together and cutting them to a length of 13-mm.
Prior to bonding, all prepared enamel surfaces were etched with a 37% phosphoric acid gel (Etch-37, Bisco, Schaumburg, IL, USA) for 30 seconds, rinsed for 20 seconds, and dried with air for 20 seconds. In the direct bonding method, both ends of a pre-fabricated twisted ligature wire were bonded to the enamel surface using one of three resins: Light-Core, Tetric N-Flow, and Transbond XT Adhesive paste. Before bonding, the etched enamel surface was primed with either One-Step (Bisco, Schaumburg, IL, USA) (for Light-Core and Tetric N-Flow) or Transbond XT Primer (3M Unitek, Monrovia, CA, USA) (for Transbond XT Adhesive paste). To standardize the bonding area (4 mm in diameter), resin thickness, and the amount of resin applied, Mini-Mold Kit (Ortho-Direct, Farmingdale, NY, USA) was used and the same pressure was applied by one author in the procedure. Light-curing was performed from the mesial and distal aspects for 10 seconds each (total time = 20 seconds) using a curing light (Skylight, Dmetec, Bucheon, Korea) with a light intensity of 1,000 mW/cm2 as measured with a radiometer.
For indirect bonding, the wire retainer was positioned on the polished bovine enamel surface. Each resin was then prepared with the same diameter and shape as used in the direct method at both ends of a ligature wire and light-cured before bonding. The ligature wire/pre-cured resin units were transferred onto the enamel surfaces prepared according to the procedures described above, and the primers then light-cured under the same light-curing conditions as in the direct method. All bonded specimens were examined under an optical microscope (× 30); specimens with bonding defects were excluded from further analysis and replaced. A diagram of a bonded specimen is shown in Fig 1.
Bonded specimens were placed in distilled water for 24 hours at 37℃. They were then removed, and SBS tests were performed. For SBS tests, specimens were secured in a jig that was attached to a universal testing machine (3343; Instron Inc., Norwood, MA, USA). A chisel-edge plunger was mounted in the movable crosshead of the machine and positioned so that the edge was aimed at the center of the ligature wire and was parallel to the tooth surface. We set the crosshead speed to 1.0 mm/min. The maximum load was recorded as the force, in Newtons (N), exerted on the wire when one of the two bonding sites separated from the tooth. Weibull analyses of the SBS data were used to calculate the Weibull modulus, characteristic bond strength, correlation coefficient, and strength levels at 5% and 10% probability of failure for each resin/bonding method combination.
After debonding, each specimen was assigned an ARI score corresponding to the amount of adhesive remaining on the enamel surface that was observable under an optical microscope. The scores were: 0 = no resin remaining; 1 = less than 50% of resin remaining; 2 = more than 50% of resin remaining; and 3 = all resin remaining.15
As the quantitative data were normally distributed (Kolmogorov-Smirnov test) and exhibited equal variance (Levene's test), the means of the different groups were compared using a two-way ANOVA with Tukey's post hoc test. p-values ≤ 0.05 were considered significant. As ARI scores are ordinal,16 we used the Mann-Whitney non-parametric test to compare ARI values between bonding methods using the same material (α = 0.05).15-17 All statistical analyses were performed using SPSS 17.0 for Windows (SPSS Inc., Chicago, IL, USA).
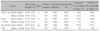
Two-way ANOVA indicated that both the resin material and the bonding method significantly affected the SBS of retainers (p = 0.017 and p < 0.001, respectively), and there was no significant interaction between these 2 factors (p = 0.149). Mean SBSs and the standard deviations for each group are summarized in Table 1. The SBS of Light-Core was significantly higher than that of Tetric N-Flow (p = 0.019), whereas the SBS of Transbond XT was not significantly different from that of Light-Core (p = 0.841). The parameters of the Weibull analysis (modulus, correlation coefficient, characteristic, and strengths at 5% and 10% probability of failure) for each group are also presented in Table 1.
Fig 2 illustrates the probability that the bonds in each tested group would fail when subjected to a given amount of shearing force. The graph indicates that direct bonding methods perform better than indirect bonding methods, in terms of SBS.
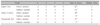
During debonding, one of the two bonding sites for each wire retainer was debonded and that side was used for ARI assessment. Table 2 shows the ARI scores for residual resin on the enamel surfaces. Direct bonding produced significantly higher ARI values for all resin materials, than indirect bonding (p < 0.05).
For all resin systems used in this study, direct bonding produced significantly higher SBS values than indirect bonding (Table 1). These results suggest that one-step direct bonding is superior to two-step indirect bonding in terms of SBS. However, caution should be used when generalizing the results directly to clinical situations because certain regions of the oral cavity, such as the lingual surface of the lower anterior teeth, do not allow easy access for bonding resins, potentially impairing practical bond strength.
Several studies have compared direct and indirect bonding, either in clinical settings18 or in vitro.19,20 Indirect bonding techniques have been investigated mainly in the context of bracket bonding. Sinha et al.11 reported that the direct technique for bracket bonding resulted in significantly higher bond strength than indirect techniques in 4 of the 7 groups evaluated. In their study, however, all combinations of techniques and adhesive type resulted in clinical bond strengths that were more than adequate. However, these results are not directly applicable to bonding of lingual retainers. It is not necessarily beneficial for orthodontic adhesives to have high SBS, because enamel can be lost during the debonding procedure as well as during the removal of residual resin.21 Bishara et al.22 reported that an SBS of 7 MPa was clinically acceptable for bonding to the enamel surface. In contrast to bracket bonding, retainer bonding may not require a debonding step. Therefore, in this application, there is no disadvantage associated with high SBS, and high SBS might even provide some advantages. When high bond strength is the primary clinical concern, we recommend direct bonding of a wire retainer.
Weibull analysis indicates the probability of failure of a given material, and how that material is likely to perform in clinical situations.23 The Weibull-derived graph of data from the present study provides additional information that is not evident from the statistical analysis of the SBS data (Fig 2). The graph clearly shows that for all 3 resins, direct bonding performs more reliably than indirect bonding. Although Light-Core and Transbond XT had similar SBS values (Table 1), Light-Core is predicted to have greater SBS reliability. Because relatively low stress levels may cause the failure of bonds, even those with high mean bond strength value,23,24 we calculated the SBS values at 5% and 10% failure probability. The values at both 5% and 10% probability of failure were higher for indirect bonding of the Light-Core group than for the Transbond XT group (11.65 vs. 7.94 N for 5% failure probability; 13.16 vs. 9.56 N for 10% probability of failure). A core build-up material such as Light-Core would thus be a better choice than Transbond XT for indirect bonding of a lingual retainer.
In direct bonding, filled resins are applied onto "very thin" uncured, unfilled liquid sealant (One-Step or Transbond XT primer in this study). This allows the light-cure filled resins to copolymerize with the unfilled liquid sealant under light curing.25 In indirect bonding, Light-Core and Tetric N-Flow groups had significantly different SBS values despite using the same sealant, One-Step (Table 1). Although the precured filled resins are linked with the uncured liquid sealant chemically as well as micromechanically, it seems that the copolymerization of liquid sealant and filled resin produces better polymerization than when liquid sealant is light cured under a pre-cured filled resin.25
For all three materials, ARI scores for the indirect method were significantly lower than those for direct methods (Table 2), indicating more frequent adhesive failure between the resin and the enamel surface are likely when indirect methods are used. Unlike bracket bonding, wherein a failure at the enamel/adhesive interface results in enamel surface damage,15 the lower ARI scores for indirectly bonded groups might be attributable to lower SBS values. Moreover, there was no evidence of enamel cracks after debonding in this study, even when the ARI score was 0. Although low ARI scores might predict easy clean-up during the bracket debonding procedure,11 this is not necessarily a favorable property for lingual retainer bonds, as these might be permanent and thus never debonded.
The Light-Core group was expected to have a significantly higher SBS than the other groups due to its greater strength. However, its SBS was not statistically different from that of the Transbond XT group. This result may be partially attributable to poor wetting of the Light-Core around the prepared ligature wire, resulting in the formation of a gap between the two materials and thus a lower SBS.
There were certain limitations to the experimental design of this in vitro study. As a wide enamel surface is required for retainer bonding, bovine teeth were used instead of human teeth. We assumed that the retainers would bond to bovine enamel in the same way as to human enamel.23,26 However, bond strengths to bovine teeth have been reported to be lower than for human teeth.23,27 Moreover, the bovine teeth were polished to obtain a flat enamel surface for bonding. In clinical situations, the surface (e.g., the lingual side of the upper incisors) for a lingual retainer is not flat. Therfore, it may sometimes be difficult for resin bonding systems to wet the entire tooth area to be bonded. To avoid such an event, the viscosity of the resin bonding systems should be optimized. Although core build-up composites such as Light-Core are recommended for indirect retainer bonding, these materials have a rough surface and do not finish well due to the incorporation of large filler particles,13 a surface property that might stimulate plaque accumulation. The potential for increased plaque accumulation associated with the use of this material requires further research. Gentle tapping of resin with cotton ball, however, may reduce surface roughness clinically. Additionally, some clinicians might find that fields like the lingual surface of lower anterior teeth are difficult to isolate and make moisture-free. As this is necessary for the indirect method, such factors will probably result in lower retainer-to-enamel bond strength than seen in this study. Therefore, longer-term bond strength tests simulating aging through techniques such as thermocycling or long-term water immersion are needed together with clinical observation to determine the clinical performance of various bonding techniques for lingual retainers.
The direct bonding method for a wire retainer produced significantly higher shear bond strengths than indirect methods, regardless of the resin system used.
The Weibull analysis suggested that Light-Core might perform better than Transbond XT and Tetric N-Flow when bonding with indirect method.
Figures and Tables
Fig. 2
Probability of failure versus shear bond strength for all tested groups according to Weibull analysis. LC, Light-Core; TF, Tetric N-Flow; TX, Transbond XT; D, direct bonding method; and ID, indirect bonding method.
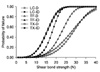
Table 1
Mean shear bond strengths, standard deviations (in parenthesis), and Weibull parameters for each group (N = 15)
References
1. Little RM, Riedel RA, Engst ED. Serial extraction of first premolars--postretention evaluation of stability and relapse. Angle Orthod. 1990. 60:255–262.
2. Little RM, Riedel RA, Stein A. Mandibular arch length increase during the mixed dentition: postretention evaluation of stability and relapse. Am J Orthod Dentofacial Orthop. 1990. 97:393–404.

3. Little RM, Riedel RA, Artun J. An evaluation of changes in mandibular anterior alignment from 10 to 20 years postre-tention. Am J Orthod Dentofacial Orthop. 1988. 93:423–428.

4. Littlewood SJ, Millett DT, Doubleday B, Bearn DR, Worthington HV. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst Rev. 2006. CD002283.

5. Sadowsky C, Schneider BJ, BeGole EA, Tahir E. Long-term stability after orthodontic treatment: nonextraction with prolonged retention. Am J Orthod Dentofacial Orthop. 1994. 106:243–249.

6. Zachrisson BU. Clinical experience with direct-bonded orthodontic retainers. Am J Orthod. 1977. 71:440–448.

7. Bearn DR. Bonded orthodontic retainers: a review. Am J Orthod Dentofacial Orthop. 1995. 108:207–213.

8. Bearn DR, McCabe JF, Gordon PH, Aird JC. Bonded orthodontic retainers: the wire-composite interface. Am J Orthod Dentofacial Orthop. 1997. 111:67–74.

9. Sondhi A. Efficient and effective indirect bonding. Am J Orthod Dentofacial Orthop. 1999. 115:352–359.

10. Zachrisson BU, Brobakken BO. Clinical comparison of direct versus indirect bonding with different bracket types and adhesives. Am J Orthod. 1978. 74:62–78.

11. Sinha PK, Nanda RS, Duncanson MG, Hosier MJ. Bond strengths and remnant adhesive resin on debonding for orthodontic bonding techniques. Am J Orthod Dentofacial Orthop. 1995. 108:302–307.

12. Cadenaro M, Marchesi G, Antoniolli F, Davidson C, De Stefano Dorigo E, Breschi L. Flowability of composites is no guarantee for contraction stress reduction. Dent Mater. 2009. 25:649–654.

13. Albers HF. Tooth-colored restoratives: principles and techniques. 2002. 9th ed. Hamilton, Ontario, Canada: BC Decker;111–125.
14. Uysal T, Ulker M, Baysal A, Usumez S. Different lingual retainer composites and the microleakage between enamel-composite and wire-composite interfaces. Angle Orthod. 2008. 78:941–946.

15. Ryou DB, Park HS, Kim KH, Kwon TY. Use of flowable composites for orthodontic bracket bonding. Angle Orthod. 2008. 78:1105–1109.

16. Toroglu MS, Yaylali S. Effects of sandblasting and silica coating on the bond strength of rebonded mechanically retentive ceramic brackets. Am J Orthod Dentofacial Orthop. 2008. 134:181e1–181e7.

17. Isci D, Sahin Saglam AM, Alkis H, Elekdag-Turk S, Turk T. Effects of fluorosis on the shear bond strength of orthodontic brackets bonded with a self-etching primer. Eur J Orthod. 2011. 33:161–166.

18. Aguirre MJ, King GJ, Waldron JM. Assessment of bracket placement and bond strength when comparing direct bonding to indirect bonding techniques. Am J Orthod. 1982. 82:269–276.

19. Hocevar RA, Vincent HF. Indirect versus direct bonding: bond strength and failure location. Am J Orthod Dentofacial Orthop. 1988. 94:367–371.

20. Yi GK, Dunn WJ, Taloumis LJ. Shear bond strength comparison between direct and indirect bonded orthodontic brackets. Am J Orthod Dentofacial Orthop. 2003. 124:577–581.

21. Martin S, Garcia-Godoy F. Shear bond strength of orthodontic brackets cemented with a zinc oxide-polyvinyl cement. Am J Orthod Dentofacial Orthop. 1994. 106:615–620.

22. Bishara SE, Gordan VV, VonWald L, Jakobsen JR. Shear bond strength of composite, glass ionomer, and acidic primer adhesive systems. Am J Orthod Dentofacial Orthop. 1999. 115:24–28.

23. Elekdag-Turk S, Turk T, Isci D, Ozkalayci N. Thermocycling effects on shear bond strength of a self-etching primer. Angle Orthod. 2008. 78:351–356.

24. McCabe JF, Walls AW. The treatment of results for tensile bond strength testing. J Dent. 1986. 14:165–168.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download