Abstract
Objective
To identify clinical, salivary, and bacterial changes during orthodontic treatment with follow-up to 24 months.
Methods
In 30 patients, clinical (decayed, missing, and filled surfaces [DMFS], O'Leary's plaque index, and plaque pH), salivary (unstimulated and stimulated saliva, buffer capacity, pH, and occult blood), and bacterial (Streptococcus mutans and Lactobacillus) markers were evaluated. A questionnaire was employed to evaluate their hygienic-dietary habits. Data were analyzed by ANOVA, logistic regression and Spearman's correlation.
Results
DMFS increased significantly, whereas the plaque index diminished, plaque pH was more acidic (p = 0.23), and unstimulated salivary flow showed significant differences during the treatment (p = 0.013). Stimulated saliva flow increased in females after the placement of appliances; buffer capacity was diminished in males during the therapy; salivary pH remained at basal values. Bacterial levels and occult blood increased to high-risk levels and were not statistically significant different between genders (p > 0.05). Two major relationships were confirmed: initial plaque with use of dental aids (r = 0.429; p = 0.018) and final DMFS with unstimulated salivary flow (r = -0.372; p = 0.043).
The dental literature reports that orthodontic treatment induces changes in the oral environment by increasing the number of retentive surfaces for plaque, augmenting the bacterial levels of Streptococcus mutans (SM) and Lactobacillus; these modify the patient's salivary characteristics, for example, pH, buffer capacity, and salivary flow.1-5 These alterations increase caries risk: some patients develop white spots on the enamel surface and generalized gingival alterations that appear at the completion of and even during orthodontic treatment.6,7
Enamel demineralization after placing orthodontic appliances can affect more than 50% of patients,6 sometimes progressing rapidly. The process is found most frequently in cervical and middle thirds of the buccal surfaces of upper lateral incisors, lower canines, and first premolars.8 These changes in the oral environment can be worsened by the use of attachments such as elastic chains, loops, and springs. Nevertheless, the best way to minimize this problem is plaque control. Some studies recommend scrupulous oral cleanliness, suggesting the use of irrigators,9 electrical or ultrasonic brushes,10 rinsings,11 and varnish,12 but one of the most important requirements for oral health is the motivation of the patient.
Therefore, the aim of this study was to identify changes in the oral environment in hygienic-dietary habits, saliva, plaque, and bacterial counts during four different stages of orthodontic treatment.
Patients who required treatment with fixed orthodontic appliances (straight wire technique) from the Orthodontic Clinic at the Research Center and Advanced Studies in Dentistry of the Autonomous University of the State of Mexico (UAEM) were studied. Thirty patients, including 11 males (mean age, 16.5 ± 3.7 years) and 19 females (mean age, 16.5 ± 5.5 years) participated. Patients having any systemic disease, using antibiotics within 15 days of enrolling in the study, having active caries, or being in the mixed dentition phase were excluded. Dental and skeletal diagnoses were made for each patient, defined by Angle's molar class and cephalometric angle ANB.
The Ethics Committee of the University approved this research. All patients or their guardians consented to participate after obtaining information about the study.
Not all patients started their orthodontic treatment at the same time, so during 24 months, samples were taken from the same patients over four different stages of orthodontic treatment (Fig 1).
Patients were to avoid eating, drinking, and toothbrushing for 2 hours before sample processing. Two certified researchers performed all procedures, and the commercial kits were used according to the manufacturers' instructions. Intraexaminer reliability in using these kits and evaluating all markers was tested prior to the study using a group of orthodontic patients from one author's (NMMB) clinical practice.
Subjects were examined in the clinic area with the aid of a dental mouth mirror and periodontal probe, type E. The presence of caries was recorded using WHO13 DMFS criteria.
Plaque was disclosed with a chewable tablet (Viarden®; Viarden, Mexico City, Mexico) and its amount estimated using criteria according to O'Leary's plaque index.14,15 This index was evaluated before toothbrushing as routinely performed by the patients to verify whether the techniques they employed were effective for plaque removal.
Plaque from the buccal surface of the upper first molar was collected with a Q-tip and evaluated with the aid of Cariostat®16,17 (Dentsply-Sankin KK, Tokyo, Japan). The material was placed inside the culture and incubated at 37℃ for 48 hours. The pH was determined according to the color: dark blue, pH = 6.1; green, pH = 5.4; greenish-yellow, pH = 4.7; and bright yellow, pH = 4.0.
Unstimulated salivary flow was measured by the time of formation of small drops of saliva on the mucous membrane of the lower lip (Saliva Check®, GC America Inc, Alsip, IL, USA). The results were expressed in seconds.18
Stimulated salivary flow was obtained by chewing on an unflavored piece of wax for 5 minutes. The patient was asked to chew bilaterally in the usual way, as in chewing gum; the ensuing saliva was collected in a graduated cup. The volume was measured and the flow expressed in ml/min.18
Buffer capacity was determined by placing the saliva in a strip test (Saliva Check®, GC America Inc, Alsip, IL, USA); after 2 minutes, the final result was obtained by adding the scores of 3 reactive zones: 5 points = very low; 6 - 9 points = low; ≥ 10 points = normal.18
The reactive strip of the Saliva Check® kit was submerged in stimulated saliva for 10 seconds and the color obtained was compared with categorical levels in the chart: 5.0 - 5.8 = highly acidic; 6.0 - 6.6 = moderately acidic; and 6.8 - 7.8 = healthy saliva.18
S. mutans was measured in stimulated saliva using a commercial technique, Dentocult-SM® (Orion Diagnostica, Espoo, Finland) according to Jensen and Bratthall.19,20 The classification of test scores was 0 = negative or < 104 colony-forming units (CFU)/ml, 1 = 105 CFU/ml, 2 = 105 to 106 CFU/ml, and 3 = > 106 CFU/ml.
To measure "occult blood in saliva," we used the Salivaster® reactive strip (Showa Yakuhin Kako Co, Tokyo, Japan).22 The procedure involves dipping the test paper into the hematemetic, stimulated saliva for 2 - 3 seconds and then judging by comparing it with the standard color-change chart. The color reaction is divided into three levels: no change = 0.0 mg of blood per ml of saliva (no periodontal disease), light-blue = 1.0 mg/ml (incipient periodontal disease), and dark-blue = 2.5 mg/ml (periodontal disease present).
The patients were asked to fill out a questionnaire stating their identification data and hygienic-dietary habits, both before treatment and at the last stage. This questionnaire included a series of questions regarding daily brushing and eating habits, focusing on behavioral risk factors for dental disease. The questions were the following: 1) When do you brush your teeth?, 2) How many times do you brush your teeth per day?, 3) Do you use some dental auxiliary for cleaning your mouth?, 4) How often do you change your toothbrush?, 5) Do you eat between meals?, 6) How many times per day do you eat food between meals?
Recommendations to avoid sticky, cariogenic, and hard foods during orthodontic treatment were provided verbally. We recommended that patients brush their teeth three times a day using the Bass modified technique with fluoridated toothpaste after the placement of appliances.
Clinical data (DMFS and plaque index) and hygienic-dietary habits were obtained only before treatment and at the final stage. The following statistical analyses were used: (a) a repeated-measures ANOVA model to analyze quantitative variables; (b) a logistic regression model for bimodal or multinomial response variables; and (c) a Spearman's correlation test to measure the association between the variables and the questionnaire. The information was analyzed using JMP 7.0.1 (SAS Institute Inc, Cary, NC, USA). The statistical level of significance was set at 0.05.
Fifteen patients had Class I molar relation, 10 had Class II, 4 had class III, and in 1 patient it was not possible to determine the relationship due to missing first molars. As for skeletal diagnosis, 13 were Class I, 16 were Class II, and 1 was Class III. When we analyzed skeletal diagnoses, we eliminated Class III because the sample size was too small. However, dental and skeletal diagnoses did not correlate with or determine the behavior of any of the studied variables (p > 0.05) (data not shown).
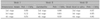
The initial mean on the DMFS index was 5.7 (6.7 for females and 4.1 for males; p = 0.407). In the follow-up study, the DMFS increased slightly to 5.9 (7.0 for females and 4.2 for males, p = 0.391); we did not observe differences between the two stages (p = 0.057; Tables 1 and 2).
The initial plaque index was 43.9%. The average of the follow-up plaque index decreased by 39.9% (Table 1). The males showed a greater, but not statistically significant, decrease (53.5%) than females (38.3%) (p = 0.079; Table 2). At the final stage we observed a similar trend: males decreased by slightly more than females (45.2% vs. 36.8%; p = 0.163). The difference between the initial and final plaque indices in our total study population was not significant (p = 0.061).
The plaque acidity decreased during the orthodontic treatment, though no significant differences were found (p = 0.230; Table 1). Initially only one patient showed parameters of high risk, and at the fourth sample, they were 8/30 with values of high risk. Only at the first stage did we find differences between genders (p = 0.004; Table 2).
Using a repeated-measure analysis between the four unstimulated-saliva stages, we observed significant differences between all the samples (p = 0.013), indicating a diminution of unstimulated saliva flow (Table 1). On the basis of gender, we found the means were different only at the second stage (p = 0.002; Table 2).
The stimulated salivary flow rates were stable in the follow-up study (p = 0.255). The placement of orthodontic appliances promoted a slight increase in the stimulated salivary flow in females but not in males (Table 2). Significant differences between genders were observed only at the initial stage (p = 0.001).
The salivary buffering evaluation did not demonstrate significant differences during the treatment (p = 0.548; Table 1), although at the first stage there were differences between genders (p = 0.040). The salivary buffer capacity in males decreased during treatment, whereas it increased in females after the placement of appliances and later diminished (Table 2).
When we applied a multinomial logistic regression model for initial bacteria and occult blood in saliva fitted by Streptococcus mutans (SM), Lactobacillus (LB) and occult blood history during the follow-up, we found significant differences in the distribution of SM at the second stage and marginal differences at the last stage (anterior segment retraction; Table 3). During treatment, changes in bacterial counts appeared; at the first stage, 13 of 30 (13/30) subjects had high-risk values for caries (>105); at the second stage, there were 15/30, and at the third and fourth stages, there were 26/30 with high values (Table 4).
At the beginning of the study, 7/30 patients showed high-risk values, and at the final stage, 17/30 had an increased risk. A greater presence of blood derived from inflamed gingival tissue was found at the first and second stages of treatment. We then observed stabilization during the processes of canine retraction and anterior segment retraction (chi-square values of 0.07 and 0.08, respectively, by multinomial logistic regression analysis).
At the beginning of the study and at the time of taking the final sample (anterior segment retraction with closing loops), we queried the patients' hygienic and dietary habits with a questionnaire. We compared their responses with the experimental results to determine the influence hygienic-dietary habits may have had on the latter. Table 5 shows those statistically significant associations revealed by the correlation analysis. The salivary factors (pH, buffer capacity, stimulated and unstimulated salivary flow) were correlated with each other (p < 0.0001).
Several relationships were confirmed, for example initial plaque with use of dental aids (r = 0.429; p = 0.018); final DMFS with unstimulated salivary flow (third stage) (r = -0.372; p = 0.043); buffer capacity with LB (third stage) (r = -0.419; p = 0.021); and Salivaster (third stage) with frequency of toothbrushing (r = 0.399; p = 0.029).
In the present study we determined the changes in clinical, salivary, and bacterial markers that occur in the oral environment during four stages of orthodontic treatment with fixed appliances on permanent dentition. Actually, there exist few clinical studies that show the physiologic and biological characteristics of saliva, plaque and bacteria and their correlation. There are no reports relating these to the behavior of patients undergoing orthodontic therapy.
Among the clinical factors which were evaluated, the DMFS index increased slightly during orthodontic treatment, more in females than males, similar to previous reports on diverse cultures.23 Probably because women have higher risk factors than men, differences have been attributed principally to less salivary production and to hormonal patterns in women.
With the reinforcement of oral hygiene, it is possible to avoid the associations reported in the literature, as the frequency of toothbrushing positively influenced the results we obtained; this was demonstrated by the lower plaque index at the completion of the study than that at the beginning, indicating that patients can improve their hygiene habits, which is in contrast to Chang's findings.2 A previous study24 established that adequate use of the manual toothbrush can significantly reduce plaque during the first stages of orthodontic treatment. In this study we reported significant, positive correlations between plaque index and the use of dental aids. Plaque percentages were lower in females than in males, which agrees with a previous report.25
In this study unstimulated salivary production diminished during orthodontic treatment, with statistically significant differences between genders, which is consistent with Percival et al.26 The stimulated salivary flow findings also demonstrated significant differences between genders, as previously suggested,2,27,28 after the placement of orthodontic appliances. Salivary flow is known to be stimulated by foreign bodies in the mouth, which occurs after the placement of appliances; nevertheless, this study demonstrates that subjects become accustomed to the attachments, with resultant diminished salivary secretion, reaching basal parameters.
The salivary buffer capacity increased drastically after the placement of orthodontic appliances but diminished during treatment, consistent with the findings of Chang.2 At one month of treatment, he found statistically significant differences, with no significant changes between the first and third month of his study.
Salivary buffer capacity is an important factor influencing the salivary pH and relating to the salivary flow.28 This was verified in our study because all these factors were positively correlated. Patients with a high buffer capacity are often resistant to the caries process because a high host response can compensate for detrimental caries habits. If orthodontic patients at high caries risk can be identified at the beginning of treatment, preventive measures can be implemented with maximal effect.
The salivary pH did not demonstrate significant differences over four stages of orthodontic study. However, Chang2 reported a significant increase 3 months after the placement of fixed orthodontic appliances. We observed significant positive correlations of salivary pH with buffer capacity and with stimulated saliva production, which is why the subjects maintained basal salivary pH values during the treatment. The placement of orthodontic appliances altered the buffer capacity, but this salivary characteristic maintained the healthy salivary pH during the treatment.
On the other hand, as orthodontic therapy progressed, plaque became more acidic, most prominently in females, whereas the males maintained more steady plaque pH. The caries activity test Cariostat® (Dentsply-Sankin KK, Tokyo, Japan) was designed to measure the pH decrease caused by microorganisms in the dental plaque. Positive correlations between caries activity test score and the counts of Streptococcus mutans and Lactobacillus have been reported.29 In our study, the bacterial counts increased, which might explain the plaque acidification.
The oral cavity is a complex ecosystem inhabited by more than 300 bacterial species, such that any external interference, such as fixed orthodontic appliances, can disturb the delicate balance between components of the microflora in this environment.30 The presence of attachments in the mouth favors the increase of plaque which is difficult to remove, and which promotes the increase of bacteria.1,12 The findings of this study indicate that patients undergoing orthodontic treatment show a continuing increase of SM and LB levels at diverse degrees of significance. According to Rosenbloom1 the highest levels of bacteria appear in the "active treatment" stage. Likewise, the positive correlation between toothbrushing frequency and plaque control demonstrates the importance of hygiene maintenance programs during orthodontic therapy.
The development of gingivitis and gingival hyperplasia are also recognized as problems associated with fixed orthodontic treatment.11 Moreover, periodontal disease has been reported in subjects with malocclusion due to crowding, considered a primary etiologic factor in the development of periodontal injury.31
The presence of occult blood in saliva at the initial stages may be due to malocclusion. In addition, we observed that the risk of periodontal damage increased as orthodontic treatment advanced, with the introduction of elastic chains and closing loops. It should be determined whether occult blood in saliva disappears when the appliances are removed and the problem of dental malposition is eliminated.32
Stimulated salivary flow initially increased after placing the appliances; subsequently, it diminished, returning to basal levels. The increase in retentive surfaces increased bacterial levels, leading to increased plaque acidity, and gingival damage rose, as evaluated by occult blood in saliva. The placement of orthodontic appliances altered the buffer capacity, but this salivary characteristic maintained the healthy salivary pH value during the treatment.
Plaque control in orthodontic patients is essential to support periodontal and dental health. We strongly recommend a program of home care for patients wearing fixed orthodontic appliances.
Figures and Tables
Table 3
Significance levels obtained from three multinomial logistic regression models for initial bacterial markers and occult blood in saliva fitted by Streptococcus mutans, Lactobacillus and occult blood history during the follow-up
ACKNOWLEDGMENTS
We thank the National Council of Science and Technology of Mexico (CONACYT) for their support.
References
1. Rosenbloom RG, Tinanoff N. Salivary Streptococcus Mutans levels in patients before, during and after orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991. 100:35–37.

2. Chang HS, Walsh LJ, Freer TJ. The effect of orthodontic treatment on salivary flow, pH, buffer capacity, and levels of Mutans Streptococci and Lactobacilli. Aust Orthod J. 1999. 15:229–234.
3. Papaioannou W, Gizani S, Nassika M, Kontou E, Nakou M. Adhesion of Streptococcus Mutans to different types of brackets. Angle Orthod. 2007. 77:1090–1095.
4. Yu JK, Ahn SJ, Lee SJ, Chang YI. Quantitative analysis of Mutans Streptococci adhesion to various orthodontic bracket materials in vivo. Korean J Orthod. 2009. 39:105–111.

5. Choi JH. Comparison of slim bristled and V-shaped orthodontic toothbrushes in patients with fixed orthodontic appliances. Korean J Orthod. 2009. 39:383–392.

6. Faltermeier A, Bürgers R, Rosentritt M. Bacterial adhesion of Streptococcus Mutans to esthetic bracket materials. Am J Orthod Dentofacial Orthop. 2008. 133:4 Suppl. S99–S103.
7. Alves PV, Alviano WS, Bolognese AM, Nojima LI. Treatment protocol to control Streptococcus Mutans level in an orthodontic patient with high caries risk. Am J Orthod Dentofacial Orthop. 2008. 133:91–94.

8. Derks A, Kujipers-Jagtman AM, Frencken JE, Van't Hof MA, Katsaros C. Caries preventive measures used in orthodontic practices: An evidence-based decision? Am J Orthod Dentofacial Orthop. 2007. 132:165–170.

9. Sharma NC, Lyle DM, Qaqish JG, Galustians J, Schuller R. Effect of a dental water jet with orthodontic tip on plaque and bleeding in adolescent patients with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2008. 133:565–571.

10. Costa MR, Silva VC, Miqui MN, Sakima T, Spolidorio DM, Cirelli JA. Efficacy of ultrasonic, electric and manual toothbrushes in patients with fixed orthodontic appliances. Angle Orthod. 2007. 77:361–366.

11. Tufekci E, Casagrande ZA, Lindauer SJ, Fowler CE, Williams KT. Effectiveness of an essential oil mouthrinse in improving oral health in orthodontic patients. Angle Orthod. 2008. 78:294–298.

12. Derks A, Frencken J, Bronkhorst E, Kuijpers-Jagtman AM, Katsaros C. Effect of chlorhexidine varnish application on Mutans Streptococci counts in orthodontic patients. Am J Orthod Dentofacial Orthop. 2008. 133:435–439.

13. World Health Organization. Oral Health Surveys. Basic methods. 1997. 3rd ed. Geneva: WHO.
14. Arrieta-Blanco JJ, Bartolomé-Villar B, Jiménez-Martinez E, Saavedra-Vallejo P, Arrieta-Blanco FJ. Bucco-dental problems in patients with diabetes mellitus (I): Index of plaque and dental caries. Med Oral. 2003. 8:97–109.
15. O'Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972. 43:38.
16. Koroluk L, Hoover JN, Komiyama K. The sensitivity and specificity of a colorimetric microbiological caries activity test (Cariostat) in preschool children. Pediatr Dent. 1994. 16:276–281.
17. Montiel BN, Satoh Y, Shimizu Y, Kawarai C, Kanegae H, Yasui T. Relationship among snack taking, caries activity, and caries prevalence in Japanese infants and young children. Meikai Univ Dent J. 2002. 31:149–153.
18. Varma S, Banerjee A, Bartlett D. An in vivo investigation of associations between saliva properties, caries prevalence and potential lesion activity in an adult UK population. J Dent. 2008. 36:294–299.

19. Jensen B, Bratthall D. A new method for the estimation of Mutans Streptococci in human saliva. J Dent Res. 1989. 68:468–471.

20. Davenport ES, Day S, Hardie JM, Smith JM. A comparison between commercial kits and conventional methods for enumeration of salivary Mutans Streptococci and Lactobacilli. Community Dental Health. 1992. 9:261–271.
21. Larmas M. A new dip-slide method for the counting of salivary Lactobacilli. Proc Finn Dent Soc. 1975. 71:31–35.
22. Montiel BN, Nagai A. A study on changes in some oral environmental factors caused by orthodontic treatment with fixed appliances. Meikai Univ Dent J. 2006. 34:188–197.
23. Farsi N. Dental caries in relation to salivary factors in Saudi population groups. J Contemp Dent Pract. 2008. 9:16–23.

24. Hickman J, Millett DT, Sander L, Brown E, Love J. Powered vs manual tooth brushing in fixed appliance patients: A short term randomized clinical trial. Angle Orthod. 2002. 72:135–140.
25. Davies TM, Shaw WC, Worthington HV, Addy M, Dummer P, Kingdon A. The effect of orthodontic treatment on plaque and gingivitis. Am J Orthod Dentofacial Orthop. 1991. 99:155–161.

26. Percival RS, Challacombe SJ, Marsh PD. Flow rates of resting whole and stimulated parotid saliva in relation to age and gender. J Dent Res. 1994. 73:1416–1420.

27. de Almeida PV, Gregio AM, Machado MA, de Lima AA, Azevedo LR. Saliva composition and functions: a comprehensive review. J Contemp Dent Pract. 2008. 9:72–80.

28. Fenoll-Palomares C, Muñoz-Montagud JV, Sanchiz V, Herreros B, Hernández V, Mínguez M, et al. Unstimulated salivary flow rate, pH and buffer capacity of saliva in healthy volunteers. Rev Esp Enferm Dig. 2004. 96:773–783.

29. Nishimura M, Bhuiyan MM, Matsumura S, Shimono T. Assesment of the caries activity test (Cariostat) based on the infection levels of Mutans Streptococci and Lactobacilli in 2- to 13-year children's dental plaque. J Dent Child. 1988. 65:248–251.
30. Smiech-Slomkowska G, Jablonska-Zrobek J. The effect of oral health education on dental plaque development and the level of caries-related Streptococcus Mutans and Lactobacillus spp. Eur J Orthod. 2007. 29:157–160.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download