INTRODUCTION
Generally, dental Angle Class II patients can be treated with either distalization of the maxillary posterior teeth or extraction of two maxillary premolars.1 Since current trends in orthodontics have shifted towards non-extraction therapy, molar distalization mechanics and treatment modalities have become increasingly popular.
The traditional approach to distalize molars, especially in the maxilla, is extraoral traction.2 The advantage of this method is the stability of extraoral anchorage with fewer side effects on the non-distalized teeth. Such a treatment requires much compliance from the patient. Alternatively, several methods3-15 have been introduced for molar distalization in the treatment of dental Class II malocclusions. Among these, non-compliance intraoral appliances are gaining popularity because they minimize the dependence on patient cooperation. Intra-oral distalization techniques such as pendulum appliance,3-7 Jones Jig,8-10 and distal jet11-13 are frequently used in this fashion. Many clinical studies substantiated the effectiveness of these appliances.
Recently, a new system (Frog Appliance, Forestadent, Pforzheim, Germany) for upper molar distalization has been developed. The purpose of this report was to present the clinical efficiency of this system in the treatment of a Class II, div 1 patient.
DIAGNOSIS AND ETIOLOGY
An 11-year-old girl was referred to our clinic for orthodontic treatment with a chief complaint of protruding upper anterior teeth and irregular upper and lower teeth. She had no significant medical and dental history in terms of orthodontic treatment. She was in the permanent dentition stage. Her gingival health was moderate and the radiographs did not reveal any periodontal problem or other pathology.
Clinical examination revealed normal jaw function with no signs of temporomandibular joint dysfunction. Pretreatment facial photographs indicated that her face was symmetrical from the front and the profile was mildly convex (Fig 1). The maxillary and mandibular dental midline was coincident with the soft tissue facial midline. The dental casts and intraoral examination revealed that she had a bilateral Class II molar and canine relationship, mild upper and lower crowding, 4 mm overjet, 50 per cent overbite, and no Bolton discrepancy (Fig 2). There was no transverse discrepancy.
The initial panoramic radiograph showed no missing teeth, and alveolar bone and root formation were within normal limits (Fig 3). Cephalometrically, the patient had an SNA angle of 76°, an SNB angle of 71°, and an ANB angle of 5° (Table 1). The upper incisors had a 115° angle relative to the palatal plane and the lower incisors had a 110° angle relative to the mandibular plane.
The patient did not want to wear an extraoral appliance, and she and her parents requested full retraction of the upper anterior teeth, without extractions.
TREATMENT OBJECTIVES
The treatment objectives, based on the clinical examination and the cephalometric analysis, were to
1. Distalize the maxillary molars to establish a well-intercuspated bilateral Class I molar and canine relationship.
2. Retract the upper incisors for overjet reduction.
3. Ideally align the fully erupted lower and upper permanent teeth.
TREATMENT ALTERNATIVES
The patient's chief concern was the protruding upper incisors, and her parents wanted complete retraction of the upper anterior teeth. There were six treatment alternatives for this case: (1) distalization of upper molars using an extraoral traction, (2) distalization of upper molars using an intraoral appliance, (3) extraction of two upper first premolars, (4) extraction of four first premolars, (5) extraction of maxillary first and mandibular second premolars, and (6) fixed orthodontic treatment with extraction followed by growth modification with a functional appliance.
Usage of an extraoral appliances and extraction therapy were rejected by the patient and her parents because they were against extraction of healthy teeth for orthodontic purposes and the patient was concerned about her facial appearance with an extraoral appliance.
Thus, another alternative involving distalization of maxillary molars using an intraoral appliance and enmasse retraction of the anterior teeth was evaluated. This treatment plan was selected by the patient and her parents.
Construction of the Frog Appliance
A frog appliance kit consists of a screw, a preformed spring and a screw driver (Fig 4). Firstly, molar bands with lingual sheaths were fitted to the upper first molars for construction of the appliance. During the same visit, alginate impression was taken and molar bands were transferred to the impression. An accurate model cast of the maxillary arch was obtained. Anchor wires were bent from 0.028" stainless steel wire for the maxillary premolars. The anchor wires should lie in the embrasures distal to the anchor teeth. The frog screw is placed on the model with the distal of the appliance being aligned anteroposteriorly with the mesial of the lingual sheaths.
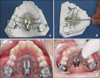
According to the manufacturer, occluso-apically the frog screw should be placed approximately 10 mm to 12 mm from the occlusal surface. This will place the appliance at approximately the center of resistance of the molars for bodily tooth movement. Therefore, we placed the frog screw 10 mm from the occlusal surface of the upper first molars. An acrylic Nance button with anterior extensions was fabricated and the frog screw was embedded in it (Figs 5A and B). The body of the frog screw was removed from the button to allow easier polishing. The preformed 0.032 inch stainless steel spring was adjusted to customize the distalizing spring (frog-legs). The polished appliance was secured with an elastic roundel for delivery to the patient.
TREATMENT PROGRESS
Treatment began with the cementation of the frog appliance into the oral cavity (Figs 5C and D). According to the manufacturer's instructions, the following procedures were followed: (1) cemented the upper first molar bands using a multi-cure glass ionomer orthodontic band cement (3M Unitek, Monrovia, CA, USA); (2) thoroughly cleaned, etched, and rinsed the anchor teeth; (3) inserted the ends of the distalizing spring into the lingual sheaths of the molar bands and pressed the Nance Button against the palate; (4) painted unfilled composite resin on the etched surfaces of the anchor teeth; (5) placed filled composite resin over the anchor wires; (6) with finger pressure held the appliance firmly in place against the palate and light cured the composite resin; (7) removed the securing elastic and activated the appliance.
According to the manufacturer, one complete rotation around the axis of the activation screw opens the appliance 0.4 mm. Three rotations are recommended for four to five-week intervals and five rotations are recommended for eight-week intervals. If second molars are erupted, three revolutions with five to six-week intervals are recommended. More than three rotations are not recommended when second molars are erupted. In our patient, the upper second molars were not erupted fully into the oral cavity so three rotations were performed to the appliance at four-week intervals. At each appointment, the stability of the appliance, progress of distalization, and oral hygiene were evaluated.
The maxillary first molars were distalized until a super Class I molar relationship was achieved (Figs 6 and 7). This was completed after four months. Soon after the maxillary first molar distalization, the device was left in place as a retention appliance after cutting of the premolar anchor wires to increase maxillary molar anchorage for three months. In this way the premolars and the canines drifted distally by means of the pull of the transeptal fibers.
Preadjusted fixed appliances (0.022 × 0.028-inch, MBT system) were placed in both arches for leveling and alignment. Maxillary premolars and canines were completely distalized by using sectional arches and power chains. After the Class I canine relationship was obtained, 0.017 × 0.025 inch stainless steel retraction archwire formed individually with reverse closing loops were used in the maxillary arch to retract the anterior teeth. At the end of active treatment, finishing procedures were applied for final alignment of the teeth and detailing of the occlusion. The orthodontic appliances were removed after active treatment was completed. A maxillary removable Hawley retainer and a canine to canine mandibular fixed lingual retainer were constructed for the patient and delivered after debonding (Figs 8, 9 and 10).
RESULTS
After 16 months of treatment with the Frog and pre-adjusted fixed appliances, a bilateral Class I molar and canine relationship with optimal alignment of both arches was obtained. Additionally, a favorable occlusal outcome with acceptable intercuspation was gained. Acceptable overjet and overbite were also achieved.
After distalization, cephalometric analysis revealed that the maxillary first molars were moved 4 mm (according to PTV) and tipped 3° (according to ANS/PNS) distally. As for anchorage loss, the upper central incisors exhibited a mesial movement of 2 mm, associated with a proclination of 4°. At the end of treatment, final cephalometric analysis and superimposition of pre- and post-treatment tracings showed that the skeletal Class II relationship had been maintained, and that she had an antero-inferior growth pattern (Fig 11). Cephalometrically, the dramatic changes were observed at overjet, overbite, and upper incisor's position at the end of treatment.
After the completion of active treatment, centric relation coincided with centric occlusion, and the patient reported no temporomandibular joint problems. The final panoramic radiograph showed good root parallelism, and the developing four third molars will be monitored.
DISCUSSION
Several methods exist for the correction of Class II malocclusion, none of which work for all patients in all situations. The availability of several methods to correct different Class II malocclusions is valuable for orthodontists. Compliance-dependent appliances such as headgear2 or removable plate appliance16 were traditionally used for upper molar distalization in treatment of Class II malocclusions. For over a decade, various innovative noncompliance intraoral molar distalization appliances have been described. These appliances derive their anchorage in an intramaxillary manner and act only in the maxillary arch to move molars distally: eg, the pendulum appliance,3-7 the sectional jig assembly,8-10 the distal jet,11-13 the Keles slider,14 or the first class appliance.15
One of the important goals of molar distalizing therapy is to obtain bodily tooth movement of the molars with minimal rotation and distal inclination. For this purpose, the vector of effective distalizing force ideally should pass through the center of resistance of upper molar or the heavy rods should be used for better control of the direction of the force. In the distal jet11-13 and the Keles slider,14 the force producers (closed coil springs) are placed at the level of center of resistance of upper first molar to obtain bodily distal movement. Similarly, the Frog appliance was positioned approximately 10 to 12 mm apically to the occlusal surface of the maxillary molar with parallel orientation to the occlusal plane in our case. In this manner, a vector of effective force passing through the centre of resistance of the first molar was obtained. The distalization force was produced by the activation of the screw. The preformed spring was not activated before inserting the appliance as pendulum springs.
In the current case, the correction of the Class II molar relationship was achieved by a 4 mm distal movement of maxillary first molar into a Class I relationship with a slight distal tipping of 3° after four months of distalization. There was also some anchorage loss as defined by maxillary incisor proclination (2 mm and 4°), increase in overjet (1.5 mm), and a mesial movement of the anchoring premolars at the end of distalization (Fig 12).
The distal jet and the pendulum are two of the more commonly used "noncompliance intraoral appliances" for upper molar distalization. Previous studies3-7,11-13 have indicated that the pendulum appliance produces on average greater molar distalization (3.14 - 6.1 mm) than the distal jet appliance (2.1 - 3.2 mm). The distal jet produces better bodily movement (1.8° - 5° of molar distal tipping) than the pendulum (8.4° - 15.7°) because the distalizing force is directed close to the level of the maxillary first molar's center of resistance. The amounts of anchorage loss that can be expected as a result of the mesial reciprocal force on the premolars are similar for both appliances (1.8 - 2.5 mm for the pendulum; 1.3 - 2.6 mm for the distal jet).
In the Jones jig studies,8-10 in addition to the distal tipping and movement of molars; there were also significant mesial movement and tipping of the anchoring premolar and increase in the overjet after distalization. Brickman et al.10 found that an average distal movement of 2.51 mm and distal tipping of 7.53° in maxillary first molar and an average mesial movement of 2 mm and mesial tipping of 4.76° in maxillary premolar at the end of distalization with the Jones jig appliance.
Anchorage control is a vexing problem during molar distalizing therapy; not only is it required for efficient molar distalization, but there is also the necessity of holding the distalized molars while the anterior dentition is subsequently retracted. Recently, intraoral molar distalizing appliances have been combined with various implants to achieve osseous anchorage and overcome the limitations of tooth and/or palate-supported appliances. Satisfactory distalization results without anchorage loss have been achieved in these implant or miniscrew supported molar distalization studies.1,17-21 We could implement the Frog appliance with an implant or a miniscrew to achieve osseous anchorage but we decided to apply it alone following the manufacturer's recommendation. Thus we aimed to determine the effects of the appliance applied alone. In further studies, the appliance can be combined with an osseous anchorage unit to eliminate the side effects on anchoring teeth.
Minor irritation of the palatal mucosa was determined after the removal of the appliance. This kind of soft tissue irritation was also reported with the use of a pendulum appliance and a Nance button. This situation can be prevented with maintenance of optimum oral hygiene.
CONCLUSION
The Frog is a fixed appliance, which does not rely on patient compliance and is doctor-controlled. Successful distalization of maxillary molars into a Class I position was achieved in 4 months. The results from this study indicate that the Frog appliance is an effective and reliable method for the distalization of maxillary molars. Unfortunately, reciprocal anchorage loss in the premolars and incisors occurred during distalization. The easy assembling and activation, lack of need for patient compliance, invisibility (palatal placement), patient acceptance and bodily molar distalization are the main advantages of the appliance. Additionally, this appliance eliminates the need to construct a new Nance appliance to stabilize the molars in their new positions after distalization. However, further studies with large samples are needed to determine the effects of it on dentofacial structures.




 PDF
PDF ePub
ePub Citation
Citation Print
Print













 XML Download
XML Download