Abstract
Objective
Intraoral noncompliance upper molar distalization techniques have gained in popularity and have subsequently found to be successful in Class II correction. The aim of the present study was to introduce a screw supported intraoral distalization appliance and investigate its efficiency.
Methods
Twenty-one subjects (11 females, 10 males; average age of 14.9 years) with Angle Class II malocclusion participated in this study. Two screws were inserted behind the incisive foramen and immediately loaded to distalize the upper first molars. An intraoral screw supported distalization appliance was used to distalize the upper molars in order to achieve a Class I molar relationship. Skeletal and dental changes were evaluated using cephalometric and three-dimensional (3D) model analysis.
Results
Upper molars were distalized 3.95 mm on average and a Class I molar relationship was achieved without any anchorage loss. The upper molars were tipped only 1.49° and the upper right and left molars were rotated only 0.54° and 0.74° respectively which were statistically non-significant (p > 0.05).
Class II malocclusions can be evaluated as skeletal and dental Class II. If a skeletal Class II malocclusion involves a normal positioned mandible sagitally, it can be treated with either upper molar distalization or upper first or second premolar extractions as in dental Class II malocclusions. The orthodontist should consider many factors such as skeletal, vertical and sagittal properties, soft tissue profile and patient compliance to reach a definitive treatment plan. After detailed considerations, if molars are to be distalized, many methods are available today.1-10
The most conventional method to distalize molars is to use cervical headgear which can either be used for orthodontic or orthopedic corrections. It is easy to apply and may distalize not only upper first molars but also first and second premolars via transeptal fibers. However, lack of patient cooperation is the major disadvantage of extraoral traction,11,12 which directed researchers to investigate alternative noncompliance distalization methods. Over recent years, many studies examined appliances which require minimal patient compliance such as NiTi coil springs,13 Wilson arches,14 pendulum,5,10,15-18 Jones-jig,3,19,20 distal jet8,21,22 or Keles slider.23,24 However, all these intraoral distalization appliances cause protrusion of upper incisors which results in an increase in overjet. This is absolutely an undesirable situation in Class II treatment. Investigators have been directed to use temporary anchorage devices (TADs) to overcome this side effect. The development of dental implants has also led to their use as orthodontic anchorage. However, implants could not become widespread because the cost is relatively high and total treatment time increases due to the 3 to 6 months of healing and osseointegration period.
Kircelli et al.1 succeeded in distalizing upper molars and premolars of ten patients with a bone anchored pendulum appliance. The results showed that the anterior movement of upper incisors was restricted and so a Class I molar relationship was achieved without any anchorage loss.
Similarly, Escobar et al.9 designed a pendulum type appliance consisting of an anchorage plate screwed to the palatal area with two endosseous screws. The upper premolars were not included in the appliance and anchorage was obtained directly from the screws. The average molar movement was 6 mm in 7.8 months with 11.3° of distal tipping and a 0.5 mm retrusion of maxillary anteriors which therefore indicates no anchorage loss during distalization.
The success of screws in maintaining anchorage was recently reported by Papadopuolos.2 Stationary anchorage was provided by two miniscrews and upper molars were moved into a Class I molar relationship within 6 months in a parallel manner in an 11.5 year old girl.
The present prospective study was aimed to investigate the efficiency of a newly designed screw supported maxillary molar distalization appliance with cephalometric and three dimensional (3D) model analyses.
The treatment sample consisted of 21 patients (11 females, 10 males) with an average age of 14.9 years (between 13 - 19 years) at the beginning of treatment. The inclusion diagnostic criterion was an Angle Class II malocclusion, requiring distalization of the maxillary molars with normal vertical relationships and overbite. All patients and parents were informed about the study procedure and an informed consent was received. The study was reviewed and approved by the Medical Scientific Ethics Committee of Cumhuriyet University. Both upper second molars of each patient were erupted and if present, both upper third molars of all patients were extracted or germectomy was performed prior to distalization in order to avoid tipping of first and second molars during distalization.
Two intermaxillary fixation (IMF) screws with a 2.0 mm diameter and 11 mm length (M-5146, 11, Medartis AG, Basel, Switzerland) were used for intraosseous anchorage. The screws were placed right and left of the incisive canal with a safe distance away from the midpalatal suture following the palatinal anatomy.
The upper molars were banded and stone casts were obtained. Teucher tubes of 0.045-inch diameter (Leone A076-45, Firenze, Italy) were soldered on the palatal side of the first molar bands at the level of the centre of resistance of the first molars. A 1.1 mm diameter stainless steel (SS) wire was oriented parallel to the occlusal plane and passed through the tube. The SS wire was extended about 7 mm distal to the tube and a "U" bend was made (Fig 1). A Ni-Ti coil spring of 25 mm length, 0.055-inch diameter, and 0.014-inch thickness (Leone C1214-55, Firenze, Italy) was placed on the wire and activated with Gurin lock (3M Unitek, Monrovia, CA, USA) in full compression. By adopting this approach, 300 gm of consistent force was obtained. Screws and palatal mucosa were blocked out with wax, and an acrylic plate was prepared on stone casts. The appliance was carried to the mouth, bands were cemented and the spaces between screws and acrylic were filled with light cure adhesive (3M Unitek, Transbond XT, Monrovia, CA, USA). The patients were monitored every 6 weeks and coil springs were compressed by a Gurin lock screwdriver when necessary. After both upper molars were distalized and a Class I molar relationship was obtained, upper molars were banded, a transpalatal arch was placed and the treatment was continued with fixed appliance therapy.
Study models and lateral cephalograms were obtained before and after molar distalization. Seventeen cephalometric landmarks were selected to measure dental, skeletal and soft tissue changes. A perpendicular line was drawn to the SN plane from the intersection of the anterior wall of sella turcica and the anterior clinoid processes in order to form a vertical reference plane (Fig 2). The stability of these landmarks during growth has been shown previously.25
Model analysis was carried out with 3D digital images. For this purpose, impressions were taken before and after molar distalization and all dental casts sent to O3DM laboratory (OrtoLab, Czestochowa, Poland) for 3D surface laser scanning. A sagittal plane passing through the incisive papilla and midpalatal suture was drawn on the 3D models and the degree of rotation of each maxillary first molar and the amount of expansion of first molars were calculated (Fig 3).
Both cephalometric and 3D model measurements were repeated one month after the initial measurements and the method error was calculated according to Dahlberg's26 formula. The mean cephalometric measurement error was between 0.06 and 0.36, and the mean 3D digital model measurement error was between 0.10 and 0.32 which were near to the ideal value of zero. Wilcoxon Matched-Pairs Signed-Ranks Test (α= 0.05) was implemented in order to determine the differences before and after molar distalization. A probability of 0.05 was accepted as critical significance.
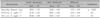
Class I molar relationship was obtained in all patients in an average of 9.61 ± 2.1 months (ranging between 6 to 12 months). The incisors were not moved forward during distalization, furthermore they were retruded (Table 1). The treatment was continued with fixed appliances and lasted a mean of 13 months. A sample case is demonstrated in Figs 4, 5 and 6. The screws remained stable in all patients during distalization. The adjacent tissues around the screw showed minimum to moderate inflammation, but spontaneously recovered in a few days. No complication was seen during germectomy and/or at the postoperative period.
The mean maxillary molar distalization was 3.95 ± 1.35 mm while distal tipping was only 1.49 ± 1.75°. However, it showed 5.8 ± 4.53° and 3 ± 4.41° on the first and second premolars respectively. The maxillary incisors were slightly retroclined (1.33 ± 2.03°) during distalization. The mean, standard deviation (SD) and statistical significance of the skeletal, dental and soft tissue cephalometric changes are summarized in Table 1.
The results of 3D cast analysis showed that the upper right and left first molars showed distobuccal rotation which was statistically nonsignificant (0.54 ± 1.74° and 0.74 ± 0.4° respectively). Maxillary first molars were expanded an average of 2.75 ± 1.07 mm (Table 2). The superimposition of cephalometric tracings on the maxillary plane and superimposition of 3D images of the maxilla indicated bodily distal movement of first molars, distal movement of premolars with distal crown tipping and slight incisor retrusion (Figs 7 and 8).
Many studies on intraoral maxillary molar distalization without patient cooperation were carried out in order to overcome the patient compliance problem created by extraoral distalization appliances.1-10,13-24 However, these appliances also have some disadvantages such as an anchorage problem, which means upper incisor protrusion and mesial movement of premolars, prolonged treatment time and jiggling effect during retraction of proclined upper incisors.3-6,8,10,13-24 In order to try to avoid these side effects, researchers have benefited from rigid bone anchors such as osseointegrated implants7,27,28 and intraosseous screws.1,2,4,9 Several clinical studies showed that implants have the potential to resist orthodontic forces,7,27,28 which has also been proved with histological studies.29,30 Although their success in maintaining anchorage is certain, implants nevertheless have some limitations including the fact that they cannot be immediately loaded due to need of an osseointegration period, in addition to increased costs and additional surgical procedure during removal.
Screws can provide sufficient anchorage, require simple and less invasive surgical procedures and are less costly relative to implants. Thereby, screw supported intraoral distalization devices have gained popularity in the recent past.1,7,9,31 The results of these studies were very satisfactory in that the molars were moved distally and a Class I relationship was achieved in an average of 6 to 9 months. However, a significant degree of distal crown tipping of upper molars was observed during distalization which consequently creates the need for additional time, extra uprighting mechanics and overcorrection of the molar relationship.
In the present study, we aimed to achieve bodily distalization of upper first molars without any anchorage loss. Anchorage was maintained with two screws and the results showed that the incisors remained stable during distalization. The appliance used in the present study has a specialty in its design to maintain bodily distalization. The point of force application is the crucial issue when striving to achieve a parallel movement. Most distalization devices push the first molars occlusally to their center of resistance (CR) and it is certain that the closer the point to the center of resistance, the more parallel movement is achieved. In the present study, the distalization force was tried to be applied at the level of CR of the maxillary first molars on sagittal view which was at the bifurcation of their roots. Thus, distal tipping of the upper first molars was only 1.49° in the present study, while it ranged between 3° and 11.3° with other screw supported distalization mechanics.1,7,9
Use of an acrylic button might be considered a disadvantage of the appliance used in the present study due to hygienic reasons. Although mild to moderate inflammation under the acrylic button was observed due to acrylic coverage, it was spontaneously recovered within one week in all patients. The acrylic part of the appliance was very important in this system to achieve bodily distalization of the upper molars because, the rod that the first molars slide on was extended into the acrylic, thus the free part of the rod has been shortened and flexibility of the rod was reduced. A flexible rod could not resist rotational and tipping forces during distalization. As a second precaution to reduce the flexibility of the rod, a 'U' bend was inserted at the level of distal surface of the upper second molars and extended into the acrylic plate. This means that the posterior part of the rod (distal extension) that the upper molar slides on became more rigid and stable to resist rotational and tipping movements during distalization. Although the force was applied palatally from the center of resistance of the molars on frontal view, the unique design of the appliance managed to resist rotational movements in that the upper right and left first molars showed only 0.54° and 0.74° of distobuccal rotations respectively during distalization which were statistically non-significant while this was ranged between 2.40° and 8.35° with conventional and screw supported intraoral distalization appliances.1,3,31
The role of second molars in distalization of the first molars was evaluated by many researchers and generally has been considered as a barrier in traditional means of distalization. Bondemark et al.,32 Worms et al.,33 Gianelly et al.,34 Gianelly,35 Ten Hoeve,36 Jeckel and Rakosi,37 concluded that the duration of treatment would be longer, greater forces would have to be applied and more anchorage would be lost if patients had second molars. In another study, Kinzinger et al.18 investigated the role of both second and third molar eruption stages on bodily molar distalization using biomechanical analysis and concluded that a tooth bud acts on the mesial neighboring tooth like a fulcrum and that tipping of the first molars in patients in whom the second molar was still at the budding stage was thus greater. In patients whose second molars had completely erupted, the degree of tipping was greater when a third molar bud was located in the direction of movement. Consequently, in the present study due to the results of a previous study,18 distalization was anticipated until the second molars were fully erupted. However the above mentioned problems were not the case with intraosseous screw supported molar distalization.
Extraction of the upper second molars and distalizing the upper first molars would have been another treatment option. There are many studies showing improvements in upper third molar position after upper second molar extraction. Smith38 evaluated the position of 94 maxillary third molars after the extraction of second molars and found that 100% of the maxillary third molars occluded with an opposing tooth, 96% had a mesial contact point, and 97% had an acceptable axial inclination. However, in another study Staggers39 evaluated the effects of second molar extractions on third molar positions and stated that a favorable change in third molar inclination after second-molar extractions does not necessarily mean that third molars will erupt into the mouth with good inclination, proper contact with the first molar, or acceptable occlusion. Moreover, even with completion of orthodontic treatment, the appliances should remain in place in the mouth since orthodontic treatment cannot be considered finished until the upper third molars are occluded. Consequently, we preferred extraction of upper third molars in order not to prolong the total treatment time.
The upper molars were moved distally a mean of 3.95 mm and the Class I molar relationship was achieved in all patients within 9 months on average. As another advantage of the appliance, not only did the upper first and second premolars drift distally a mean of 2.73 mm and 1.70 mm respectively, but the maxillary canines tended to move to their ideal positions spontaneously. The appliance was not anchored to the first or second premolars but directly to the maxilla with two screws. Both first and second premolars were free from attachments and distally drifted by means of the pull of the transseptal fibers. In most patients, a Class I relationship was achieved spontaneously in the first and second premolars. Although the distal crown tipping was minimal in the upper first molars, it was 3.0 ± 4.41° and 5.8 ± 4.53° in the upper first and second premolars respectively. Fortunately, this tipping was easily corrected during fixed appliance therapy since the upper molars were bodily distalized and had already been uprighted.
During distalization, the mandible did not rotate and the lower anterior facial height as well as the overbite remained stable. The bite opening seen in most distalization studies have been attributed to extrusion of the maxillary first molars or the molars being distalized into the arc of closure.10 However, in the present study the design of the appliance inhibited the extrusion of upper first molars and consequently, the vertical skeletal dimensions remained stable.
Figures and Tables
 | Fig. 1Fabrication of screw supported distalization appliance. 'U' bending of 0.040 inch stainless steel rod at the level of distal surface of the second molar was performed and extended into the acrylic part of the appliance to enhance its stability. A superelastic heavy open-coil spring is compressed along the rod and activated by Gurin lock (3M Unitek, Monrovia, CA, USA). In order for easy intraoral application, a second Gurin lock was placed just behind the tube. |
 | Fig. 2
A, Cephalometric landmarks and skeletal measurements. Landmarks: S, sella; Sa, intersection of the anterior wall of sella turcica and the anterior clinoid processes; Na, nasion; Or, orbitale; Po, porion; A, A point; B, B point; Go, gonion; UL, most anterior point of the upper lip; LL, most anterior point of the lower lip; u6f, furcation point of the upper first molar; u6s, sulcus between buccal tubercules of the upper first molar; u5b, tip of the buccal cusp of the upper second premolar; u4b, tip of the buccal cusp of the upper first premolar; U1i, incisal edge of the upper central incisor; L1i, incisal edge of the lower central incisor. SV indicates vertical reference line. Skeletal measurements: 1, SNA; 2, SNB; 3, ANB; 4, Go-Gn SN; 5, FMA; 6, UL ┴ SV; 7, LL ┴ SV. B, dental angular measurements (°): 1, U1-SN; 2, U4-SN; 3, U5-SN; 4, U6-SN. Dental linear Measurements (mm): 5, U6 ┴ SN; 6, U1 ┴ SV; 7, U4 ┴ SV; 8, U5 ┴ SV; 9, U6 ┴ SV. |
 | Fig. 3Landmarks, angular and linear measurements on the 3D models. Landmarks: In, tip of the incisive papilla; Bc, tip of the buccal cusp of the upper first molar; Mpc, tip of the mesiopalatal cusp of the upper first molar; Dpc, tip of the distopalatal cusp of the upper first molar. Angular measurements (°): α (rotation of upper right first molar) and β (rotation of upper left first molar). Linear measurement (mm): 1, Intermolar distance. |
 | Fig. 4
A, Intraoral photographs before distalization; B, intraoral photographs after distalization; C, posttreatment intraoral photographs. |
 | Fig. 5
A, Lateral cephalometric radiograph before distalization; B, lateral cephalometric radiograph after distalization; C, lateral cephalometric radiograph at the end of treatment. |
 | Fig. 6
A, Panoramic radiograph before distalization, B, panoramic radiograph after distalization; C, panoramic radiograph at the end of treatment. |
 | Fig. 7Superimposition of cephalometric tracing on the maxillary plane. Solid line represents before distalization; broken line represents after distalization. |
 | Fig. 8Superimposition of 3D image on palatal rugae. White color represents before distalization; gray color represents after distalization. |
References
1. Kircelli BH, Pektaş ZO, Kircelli C. Maxillary molar distalization with a bone-anchored pendulum appliance. Angle Orthod. 2006. 76:650–659.
2. Papadopoulos MA. Orthodontic treatment of Class II malocclusion with miniscrew implants. Am J Orthod Dentofac Orthop. 2008. 134:604.e1–604.e16.
3. Gulati S, Kharbanda OP, Parkash H. Dental and skeletal changes after intraoral molar distalization with sectional jig assembly. Am J Orthod Dentofacial Orthop. 1998. 114:319–327.

4. Gelgör IE, Büyükyilmaz T, Karaman AI, Dolanmaz D, Kalayci A. Intraosseous screw-supported upper molar distalization. Angle Orthod. 2004. 74:838–850.
5. Angelieri F, Almeida RR, Almeida MR, Fuziy A. Dentoalveolar and skeletal changes associated with the pendulum appliance followed by fixed orthodontic treatment. Am J Orthod Dentofacial Orthop. 2006. 129:520–527.

6. Keles A, Sayınsu K. A new approach in maxillary molar distalization: intraoral bodily molar distalizer. Am J Orthod Dentofacial Orthop. 2000. 117:39–48.

7. Keles A, Erverdi N, Sezen S. Bodily distalization of molars with absolute anchorage. Angle Orthod. 2003. 73:471–482.
8. Bolla E, Muratore F, Carano A, Bowman SJ. Evaluation of maxillary molar distalization with the distal jet: a comparison with other contemporary methods. Angle Orthod. 2002. 72:481–494.
9. Escobar SA, Tellez PA, Moncada CA, Villegas CA, Latorre CM, Oberti G. Distalization of maxillary molars with the bone-supported pendulum: a clinical study. Am J Orthod Dentofacial Orthop. 2007. 131:545–549.

10. Chiu PP, McNamara JA Jr, Franchi L. A comparison of two intraoral molar distalization appliances: distal jet versus pendulum. Am J Orthod Dentofacial Orthop. 2005. 128:353–365.

11. Doruk C, Ağar U, Babacan H. The role of the headgear timer in extraoral co-operation. Eur J Orthod. 2004. 26:289–291.

12. Ağar U, Doruk C, Biçakçi AA, Büküsoğlu N. The role of psycho-social factors in headgear compliance. Eur J Orthod. 2005. 27:263–267.

13. Locatelli R, Bednar J, Dietz VS, Gianelly AA. Molar distalization with superelastic NiTi wire. J Clin Orthod. 1992. 26:277–279.
14. Wilson WL, Wilson RC. Multi-directional 3D functional Class II treatment. J Clin Orthod. 1987. 21:186–189.
15. Hilgers JJ. The pendulum appliance for Class II non-compliance therapy. J Clin Orthod. 1992. 26:706–714.
16. Ghosh J, Nanda RS. Evaluation of an intraoral maxillary molar distalization technique. Am J Orthod Dentofacial Orthop. 1996. 110:639–646.

17. Byloff FK, Darendeliler MA. Distal molar movement using the pendulum appliance. Part 1: Clinical and radiological evaluation. Angle Orthod. 1997. 67:249–260.
18. Kinzinger GS, Fritz UB, Sander FG, Diedrich PR. Efficiency of a pendulum appliance for molar distalization related to second and third molar eruption stage. Am J Orthod Dentofacial Orthop. 2004. 125:8–23.

19. Jones RD, White JM. Rapid Class II molar correction with an open coil jig. J Clin Orthod. 1992. 26:661–664.
20. Runge ME, Martin JT, Bukai F. Analysis of rapid maxillary molar distal movement without patient cooperation. Am J Orthod Dentofacial Orthop. 1999. 115:153–157.

21. Carano A, Testa M. The distal jet for upper molar distalization. J Clin Orthod. 1996. 30:374–380.
22. Ngantung V, Nanda RS, Bowman SJ. Posttreatment evaluation of the distal jet appliance. Am J Orthod Dentofacial Orthop. 2001. 120:178–185.

23. Keles A. Maxillary unilateral molar distalization with sliding mechanics: a preliminary investigation. Eur J Orthod. 2001. 23:507–515.

24. Keles A, Pamukcu B, Tokmak EC. Bilateral maxillary molar distalization with sliding mechanics: Keles slider. World J Orthod. 2002. 3:57–66.
25. Björk A, Skieller V. Normal and abnormal growth of the mandible. A synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur J Orthod. 1983. 5:1–46.

26. Dahlberg G. Statistical methods for medical and biological students. 1948. London: Allen and Unwin, Ltd;9–232.
27. Turley PK, Kean C, Schur J, Stefanac J, Gray J, Hennes J, Poon LC. Orthodontic force application to titanium endosseous implants. Angle Orthod. 1988. 58:151–162.
28. Roberts WE, Helm FR, Marshall KJ, Gongloff RK. Rigid endosseous implants for orthodontic and orthopedic anchorage. Angle Orthod. 1989. 59:247–256.
29. Linder-Aronson S, Nordenram A, Anneroth G. Titanium implant anchorage in orthodontic treatment: an experimental investigation in monkeys. Eur J Orthod. 1990. 12:414–419.

30. Smalley WM, Shapiro PA, Hohl TH, Kokich VG, Branemark PI. Osseointegrated titanium implants for maxillofacial protraction in monkeys. Am J Orthod Dentofacial Orthop. 1988. 94:285–295.

31. Kinzinger GS, Gülden N, Yildizhan F, Diedrich PR. Efficiency of a skeletonized distal jet appliance supported by miniscrew anchorage for noncompliance maxillary molar distalization. Am J Orthod Dentofacial Orthop. 2009. 136:578–586.

32. Bondemark L, Kurol J, Bernhold M. Repelling magnets versus superelastic nickel-titanium coils in the simultaneous distal movement of maxillary first and second molars. Angle Orthod. 1994. 64:189–198.
33. Worms FW, Isaacson RJ, Speidel TM. A concept and classifications of centers of rotation and extraoral force systems. Angle Orthod. 1973. 43:384–401.
34. Gianelly AA, Vaitas AS, Thomas WM. The use of magnets to move molars distally. Am J Orthod Dentofacial Orthop. 1989. 96:161–167.

35. Gianelly AA. Distal movement of the maxillary molars. Am J Orthod Dentofacial Orthop. 1998. 114:66–72.

36. Ten Hoeve A. Palatal bar and lip bumper in nonextraction treatment. J Clin Orthod. 1985. 19:272–291.
37. Jeckel N, Rakosi T. Molar distalization by intra-oral force application. Eur J Orthod. 1991. 3:43–46.

38. Smith DI. The eruption of third molars following extraction of second molars. Dental Pract. 1958. 8:292–294.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download