Abstract
Objective
The aim of this study was to evaluate the strain induced in the cortical bone surrounding an orthodontic microimplant during insertion in a self-drilling manner.
Methods
A 3D finite element method was used to simulate the insertion of a microimplant (AbsoAnchor SH1312-7, Dentos Co., Daegu, Korea) into 1 mm thick cortical bone. The shape and dimension of thread groove in the center of the cortical bone produced by the cutting flute at the apical of the microimplant was obtained from animal test using rabbit tibias. A total of 3,600 analysis steps was used to calculate the 10 turns and 5 mm advancement of the microimplant. A series of remesh in the cortical bone was allowed to accommodate the change in the geometry accompanied by the implant insertion.
Figures and Tables
 | Fig 1Geometry of microimplant, cortical bone specimen and the axis system together with important dimensions: A, geometry (unit: mm); B, initial mesh of the cortical bone constructed with 48,921 tetrahedral elements. |
 | Fig 2Cortical bone: A, 3D image reconstructed from micro CT data; B, A-A' aspect shown in A with detailed dimensions of thread groove. 0.3 mm chamfer was placed at the entrance of the implant bed to avoid numerical instability during FE analysis. |
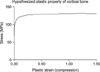 | Fig 3Material property of cortical bone used in the present study (cf. Table 1). |
 | Fig 4Strain (radial strain) distribution in the cortical bone at 9 separate stages of implant insertion (cut off strain: 4,000µ-strain). A, Step 720 (2 turns); B, step 1,080 (3 turns); C, step 1,440 (4 turns); D, step 1,800 (5 turns); E, step 2,160 (6 turns); F, step 2,520 (7 turns); G, step 2,880 (8 turns), H, step 3,240 (9 turns); I, step 3,600 (10 turns). |
 | Fig 5Development of strain (radial strain) with the course of microimplant insertion, monitored at 7 reference points. A, Location of the reference points within section A-A' (see Fig 2); B, comparison of the strains at each of 7 reference points. |
 | Fig 6Strain (radial strain) distribution in the cortical bone at 9 separate stages of implant insertion (cut off strain: 40,000µ-strain). A, Step 720 (2 turns); B, step 1,080 (3 turns); C, step 1,440 (4 turns); D, step 1,800 (5 turns); E, step 2,160 (6 turns); F, step 2,520 (7 turns); G, step 2,880 (8 turns), H, step 3,240 (9 turns); I, step 3,600 (10 turns). |
References
1. Park HS, Jeong SH, Kwon OW. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006. 130:18–25.

2. Cheng SJ, Tseng IY, Lee JJ, Kok SH. A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorage. Int J Oral Maxillofac Implants. 2004. 19:100–106.
3. Wilmes B, Rademacher C, Olthoff G, Drescher D. Parameters affecting primary stability of orthodontic mini-implants. J Orofac Orthop. 2006. 67:162–174.

4. Rubin CT, Lanyon LE. Regulation of bone mass by mechanical strain magnitude. Calcif Tissue Int. 1985. 37:411–417.

5. Frost HM. Wolff's law and bone structural's adaptation to mechanical usage: an overview for clinicians. Angle Orthod. 1994. 64:175–188.
6. Frost HM. Bone's mechanostat: a 2003 update. Anat Rec A Discov Mol Cell Evol Biol. 2003. 275:1081–1101.

7. Sugiura T, Horiuchi K, Sugimura1 M, Tsutsumi S. Evaluation of threshold stress for bone resorption around screws based on in vivo strain measurement of miniplate. J Musculoskel Neuron Interact. 2000. 1:165–170.
8. Isidor F. Loss of osseointegration caused by occlusal load of oral implants. A Clinical and radiographic study in monkeys. Clin Oral Impl Res. 1996. 7:143–152.

9. Tada S, Stegaroiu R, Kitamura E, Miyakawa O, Kusakari H. Influence of implant design and bone quality on stress/strain distribution in bone around implants: a 3-dimensional finite element analysis. Int J Oral Maxillofac Impl. 2003. 18:357–368.
10. Petrie CS, Williams JL. Comparative evaluation of implant designs: influence of diameter, length, and taper on strains in the alveolar crest. A three-dimensional finite-element analysis. Clin Oral Impl Res. 2005. 16:486–494.

11. Holmes DC, Loftus JT. Influence of bone quality on stress distribution for endosseous implants. J Oral Implantol. 1997. 23:104–111.
12. Kitagawa T, Tanimoto Y, Nemoto K, Aida M. Influence of cortical bone quality on stress distribution in bone around dental implant. Dent Mater J. 2005. 24:219–224.

13. Cha JY, Yun TM, Hwang CJ. Insertion and removal torques according to orthodontic mini-screw design. Korean J Orthod. 2008. 38:5–12.

14. Motoyoshi M, Hirabayashi M, Uemura M, Shimizu N. Recommended placement torque when tightening an orthodontic mini-implant. Clin Oral Implants Res. 2006. 17:109–114.

15. Nam OH, Yu WJ, Kyung HM. Cortical bone strain during the placement of orthodontic microimplant studied by 3D finite element analysis. Korean J Orthod. 2008. 38:228–239.

16. Meyer U, Vollmer D, Runte C, Bourauel C, Joos U. Bone loading pattern around implants in average and atrophic edentulous maxillae: a finite-element analysis. Clin Oral Impl Res. 2001. 12:648–657.

17. Meyer U, Joos U, Mythili J, Stamm T, Hohoff A, Stratmann U, et al. Ultrastructural characterization of the implant/bone interface of immediately loaded dental implants. Biometerials. 2004. 25:1959–1967.

18. Heidemann W, Gerlach KL, Gröbel KH, Köllner HG. Drill Free Screws: a new formof osteosynthesis screw. J Craniomaxillofac Surg. 1998. 26:163–168.
19. Kim JW, Ahn SJ, Chang YI. Histomorphometric and mechanical analyses of the drill-free screw as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2005. 128:190–194.

20. Chen Y, Shin HI, Kyung HM. Biomechanical and histological comparison of self-drillingand self-tapping orthodontic microimplants in dogs. Am J Orthod Dentofacial Orthop. 2008. 133:44–50.

21. Heidemann W, Gerlach KL. Clinical applications of drill free screws in maxillofacial surgery. J Craniomaxillofac Surg. 1999. 27:252–255.

22. Park HS. Orthodontic treatment using micro-implant: clinical applications of micro-implant anchorage. 2006. 2nd ed. Seoul, Korea: Daehan Nare Pub Co;18–19.
23. Sowden D, Schmitz JP. AO self-drilling and self-tapping screws in rat calvarial bone: an ultrastructual study of the implant interface. J Oral Maxillofac Surg. 2002. 60:294–299.

24. Maniatopoulos C, Pilliar RM, Smith D. Threaded versus porous-surfaced designs for implant stabilization in bone-endodontic implant model. J Biomed Mater Res. 1986. 20:1309–1333.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download