Abstract
Objective
This study investigated the skeletal and dentoalveolar changes after intrusion of maxillary posterior teeth using miniscrew implants during the treatment and posttreatment period.
Method
The subjects consisted of 11 adults (1 male, 10 females) whose open bites were treated by posterior teeth intrusion with miniscrew. The lateral cephalometric x-rays of pre-treatment, post-treatment, and the retention period were evaluated.
Results
The average intrusion of maxillary posterior teeth at the end of the treatment period was 2.22 mm (p < 0.001) and the average extrusion of maxillary posterior teeth at the end of the 17.4 month retention period was 0.23 mm (p = 0.359). The relapse rate was calculated at 10.36%. A decrease in overbite after the 17.4 month retention period was 0.99 mm (p < 0.05). The relapse rate was calculated at 18.10%. The skeletal changes and vertical height change of maxillary posterior teeth during the retention period was statistically insignificant, but there was a significant decrease in overbite (mean 0.99 mm, p < 0.05). The amount of intrusion and the overbite improvement from treatment significantly correlates to the degree of relapse.
Figures and Tables
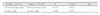
 | Fig 1Appliance for intrusion of maxillary molars using miniscrew. A, Miniscrew insertion on buccal and palatal sides (buccal view); B, miniscrew insertion on buccal and palatal sides (palatal view); C, miniscrew insertion on the buccal side only, with a palatal rigid splint for preventing buccal tipping (transverse view); D, miniscrew insertion on the buccal side only, with a palatal rigid splint for preventing buccal tipping (palatal view). |
 | Fig 2Cephalometric landmarks and reference planes. S (Sella), N (nasion), Ar (articulare), P (porion), Go (gonion), Me (menton), Gn (gnathion), Po (pogonion), Or (orbitale), ANS (anterior nasal spine), PNS (posterior nasal spine), A (A point), B (B point), U1 (upper incisor tip), U6 (upper molar mesiobuccal cusp tip), L1 (lower incisor tip), L6 (lower molar mesiobuccal cusp tip), Pog' (soft tissue pogonion); SN (SN plane), a line through sella and nasion; FH (FH plane), a line through orbitale and porion; HP (horizontal reference plane), a line through nasion rotated 7° from sella-nasion line; VP (vertical reference plane), a line through sella and perpendicular line to HP; PP (palatal plane), a line through ANS and PNS; MP (mandibular plane), a line through menton and gonion. |
 | Fig 3Skeletal angular measurements. a, SN-GoMe; b, S-N-Pog; c, SNA, S-N-A angle; d, SNB, S-N-B angle; e, ANB difference, c-d; f, IMPA, mandibular incisor long axis to Mn. plane; g, FMA, FH-MP. |
 | Fig 4Skeletal and dental linear measurements. 1, N-Me, Anterior facial height; 2, VP-Pog, Antero-posterior location of pogonion; 3, U6-PP (mm), perpendicular distance between mesiobuccal cusp of Mx. first molar to palatal plane; 4, U1-PP (mm), perpendicular distance between Mx. incisor edge to palatal plane; 5, OB (mm), distance between incisal edges of maxillary and mandibular central incisors, perpendicular to horizontal reference plane; 6, OJ (mm), distance between incisal edges of maxillary and mandibular central incisors, perpendicular to vertical reference plane. |
Table 1
Cephalometric measurements before treatment (T1), after treatment (T2), and during retention period (T3)

References
1. Lopez-Gavito G, Wallen TR, Little RM, Joondeph DR. Anterior open bite malocclusion: A longitudinal 10-year postretention evaluation of orthodontically treated patients. Am J Orthod. 1985. 87:175–186.

2. Janson G, Valarelli FP, Beltrao RT, De Freitas MR, Henriques JFC. Stability of anterior open bite extraction and nonextraction treatment in the permanent dentition. Am J Orthod Dentofacial Orthop. 2006. 129:768–774.

3. Janson G, Valarelli FP, Henriques JFC, De Freitas MR, Cancado RH. Stability of anterior open bite nonextraction treatment in the permanent dentition. Am J Orthod Dentofacial Orthop. 2003. 124:265–276.

4. Kuster R, Ingervall B. The effect of treatment of skeletal open bite with two types of bite blocks. Eur J Orthod. 1992. 14:489–499.

5. Rinchuse DJ. Vertical elastics for correction of anterior open bite. J Clin Orthod. 1994. 28:284.
6. Chang YI, Moon SC. Cephalometric evaluation of the anterior open bite treatment. Am J Orthod Dentofacial Orthop. 1999. 115:29–38.

7. Denison TF, Kokich VG, Shapiro PA. Stability of maxillary surgery in openbite versus nonopenbite malocclusions. Angle Orthod. 1989. 59:5–10.
8. Proffit WR, Bailey LJ, Phillips C, Turvey TA. Long-term stability of surgical open bite correction by Le Fort I osteotomy. Angle Orthod. 2000. 70:112–117.
9. Ko DI, Lim SH, Kim KW. Treatment of occlusal plane canting using miniscrew anchorage. World J Orthod. 2006. 7:269–278.
10. Park HS, Kwon OW, Sung JH. Nonextraction treatment of an open bite with microscrew implant anchorage. Am J Orthod Dentofacial Orthop. 2006. 130:391–402.

11. Park YC, Lee SY, Kim DH, Jee SH. Intrusion of posterior teeth using mini-screw implants. Am J Orthod Dentofacial Orthop. 2003. 123:690–694.

12. Sherwood KH, Burch JG, Thompson WJ. Closing anterior open bites by intruding molars with titanium miniplate anchorage. Am J Orthod Dentofacial Orthop. 2002. 122:593–600.

13. Umemori M, Sugawara J, Mitani H, Nagasaka H, Kawamura H. Skeletal anchorage system for open bite correction. Am J Orthod Dentofacial Orthop. 1999. 115:166–174.
14. Xun C, Zeng X, Wang X. Microscrew anchorage in skeletal anterior open bite treatment. Angle Orthod. 2007. 77:47–56.
15. Sugawara J, Baik UB, Umemori M, Takahashi I, Nagasaka H, Kawamura H, et al. Treatment and posttreatment dentoalveolar changes following intrusion of mandibular molars with application of a skeletal anchorage system (SAS) for open bite correction. Int J Adult Orthodon Orthognath Surg. 2002. 17:243–253.
17. Schudy FF. The rotation of the mandible resulting from growth: its implication in orthodontic treatment. Angle Orthod. 1965. 35:36–50.
18. Reitan K, Rygh P. Graber TM, Vanarsdall RL, editors. Biomechanical principles and reactions. Orthodontics-current principles and techniques. 1994. 2nd ed. St. Louis: Mosby;168–169.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download