Abstract
Purpose
We aimed to study the distribution of rotavirus genotypes (VP7 and VP4) and disease severity of rotavirus gastroenteritis prevalent in our community.
Methods
Stool samples were collected from 156 children who were hospitalized with rotavirus gastroenteritis from December 2007 to June 2008. The disease severity of all patients was scored using the Vesikari scale. After extraction of ds-RNA of the rotavirus, cDNA synthesis using reverse transcription and polymerase chain reaction (RT-PCR) and multiplex PCR was performed. Following this, the final identification of genotypes was performed.
Results
Of the 156 samples, VP7(G) and VP4(P) genotypes were identified in 147 (94.2%) and 140 (89.7%) samples, respectively. G1 (116 of 147 samples; 78.9%) and P[8] (137 of 140 samples; 97.9%) were the most prevalent, respectively. Of the 138 samples identified of combination types of VP7 and VP4, G1P[8] (111 samples; 80.4%) was the most prevalent. Other combination types varied with very low distribution rates. 9.4% of genotypes were not included in the new vaccines. The disease severity score was 11.8±3.3 (mean±2SD). The distribution of disease severity was mild or moderate in 37.8% and severe in 62.2% of patients.
Conclusion
The most prevalent genotype combination of rotavirus was G1P[8] and genotypes not included in the vaccines represented 9.4% in our community. Disease severity distribution of hospitalized children with rotavirus gastroenteritis was higher in the severe than in the mild and moderate categories.
In 1998, the quadrivalent Rheshus-based recombinant rotavirus vaccine (RRV-TV; Rotashield®, Wyeth Lederle Vaccines, Philadelphia, USA) received approval from the USA Food and Drug Administration (FDA) and was successfully commercialized. However, in 1999 it was withdrawn from the market because of the high correlation rate of intussusception development after immunization1). Efforts for the development of new rotavirus vaccines continued after that2,3). Finally, worldwide studies of human rotavirus attenuated vaccine (Rotarix®, GlaxosmithKline, UK)4) and pentavlent human-bovine recombinant rotavirus vaccine (RotaTeq®, Merck, USA)5) were reported in 2006 and the safety of these new vaccines for inttussusception was demonstrated. These two vaccines were approved by the Korea Food and Drug Administration in 2008.
Surface proteins of the rotavirus defining the genotypes are the 23 VP7 (G genotype) and 28 VP4 (P genotype) genes. Of the 42 combinations of G and P genotypes, G1P[8], G2P[4], G3P[8], G4P[8] and G9P[8] are common genotype combinations6,7). Combination of G1 and P[8] is the most prevalent genotype globally.
Rotarix® is an attenuated live vaccine produced in the tissue incubator using rotavirus isolated from infected humans. It consists of G1 and P1a[8]. The efficacy for the prevention of severe rotavirus gastroenteritis and hospitalization caused by rotavirus infection was as high as 85%4). RotaTeq® is a pentavalent recombinant vaccine produced from the combination of G1~4P and P[8] of the human and bovine rotavirus. It results in a high production rate of IgA in humans8). The efficacy for the prevention of overall and severe rotavirus gastroenteritis is 74% and 98%, respectively5).
Although these two new vaccines have a high prevention rate for severe rotavirus gastroenteritis, there are only a few reports on the distribution of disease severity and rotavirus genotypes in children with rotavirus gastroenteritis. Therefore, we conducted a prospective study to address this issue.
Stool samples were collected from 156 out of 283 children who were hospitalized with rotavirus gastroenteritis diagnosed by identification of rotavirus Ag using an immunoassay, from December 2007 through June 2008 in Jeju National University Hospital and Seogwipo Medical Center, Korea. All samples were immediately stored at -80.0℃ after collection. Disease severity scoring for the 156 patients was performed using the 20-point Vesikari scale9).
After thawing of frozen stool samples at -4.0℃, followed by room temperature, rotavirus ds-RNA was extracted using TRIZOL® Reagent (Molecular Research Center, Cincinnati, OH, USA). The extracted ds-RNA was denatured by mixing with DEPC water and the remaining RNA, except for a small amount for the next step, was stored at -80.0℃.
For VP7 genotyping, RT-PCR with the primers Beg9 and End9 was performed using the following protocol: 30 minutes at 42.0℃ and 25 cycles, with each cycle consisting of 1 min at 94.0℃, 2 min at 42.0℃ and 1 min at 72.0℃, followed by extension for 7 min at 72.0℃ and storage at 4.0℃. For VP4 genotyping, the primers Con3 and Con2 were used.
For VP7 genotyping, 0.5µL DNA previously amplified from RT-PCR was mixed with 19.5µL PCR mixture including primers aBT1, aCT2, aET3, aDT4, aAT8 and aFT9, and subjected to PCR using the following protocol: 30 min at 94.0℃, 30 cycles (1 cycle; 5 min at 94.0℃, 5 min at 42.0℃ and 1 min at 72.0℃), extension for 7 min at 72.0℃ and storage at 4.0℃. For VP4 genotyping, for the primers Con3, 1T1, 2T1, 3T1, 4T1, 5T1 were used.
Electrophoresis of PCR products was performed for 20 minutes on a 1.5% agarose gel mixed with ethidium bromide and 1x TAE buffer (40 mM Tris-acetate, 2 mM EDTA, pH 8.0). Electrophoretic genotyping was performed by analyzing the band sizes of PCR products. VP7 genotyping by band size was as follows: G1 type 749 bp (primer aBT1), G2 652 bp (primer aCT2), G3 374 bp (primer aET3), G4 583 bp (primer aDT4), G8 885 bp (primer aAT8) and G9 306 bp (primer aFT9). VP4 genotyping by band size was as follows: P[8] type 345 bp (primer 1T1), P[4] 483 bp (primer 2T1), P[6] 267 bp (primer 3T1), P[9] 391 bp (primer 4T1) and P[10] 583 bp (primer 5T1).
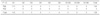
The sex distribution of the 156 children used in this study was 76 male and 80 female. The mean age of all the patients was 17.9±6.8 month (mean±2SD). Among the 156 stool samples, the VP7 gentoype was identified in 147 samples (94.2%), whereas the VP4 genotype was identified in 140 samples (87.9%) (Table 1). None of the 156 children received vaccination against rotavirus (Table 1).
For VP7 genotype distribution in the 147 patients (Fig. 1), G1 was the most common, identified in 116 patients (78.9%), follwed by G3 in 7 (4.8%), G9 in 6 (4.1%), G1/G9 in 5 (3.4%), G1/G3 in 4 (2.7%), G1/G8 in 3 (2.0%), G2 in 2 (1.4%) and G8 in 1 patient (0.7%). For VP4 genotype distribution in the 140 patients (Fig. 2), P[8] was the most common, identified in 137 patients (97.9%) followed by P[4] in 3 patients (2.1%). There was no distribution identified for P[6], P[9] and P[10].
The combination types of VP7 and VP4 was identified in 138 of 156 patients. In these 138 patients (Table 2), G1P[8] was the most common, identifed in 111 patients (80.4%) followed by G3P[8] in 5, G4P[8] in 3, G8P[8] in 1, G9P[8] in 4, G1/G3P[8] in 3, G1/G8P[8] in 3, G1/G9P[8] in 5, G1P[4] in 1 and G2P[4] in 2 patients.
Information for the scoring of disease severity of rotavirus gastroenteritis was collected from 143 patients (Table 3). In these patients, the mean duration of diarrhea was 5.06±2.27 (mean±2SD) days, whereas the mean duration of vomiting was 2.18±1.61 days. Fever of over 37.8℃ was reported in 62 (43.4%) of 143 patients. No dehydration was reported in 62.9% of patients, but mild dehydration was observed in 18.9%, moderate dehydration in 13.3%, and severe dehydration in 4.9% of patients. The disease severity score using the Vesikari scale was 11.8±3.3 (mean±2SD). The distribution of disease severity was mild or moderate in 37.8% and severe in 62.2% of patients.
Except for the Givon-Lavi et al.12) study, there were only a few reports on the distribution of disease severity of rotavirus gastroenteritis. Disease severity used to be one of the variables that was evaluated to study vaccine efficay. In our study, clinical information on scoring disease severity of rotavirus gastroenteritis was collected from 143 out of 156 patients. Disease severity score on the basis of the 20-points Vesikari scale was 11.8±3.3 (mean±2SD) (Table 3). In distribution of disease severity, the severe state (Vesikari scale≥11) was as high as 62.2% (Table 3).
This result was similar with the Givon-Lavi et al. report in that 756 (76.6%) of 987 rotavirus infected patients were classified in the severe state13). They also reported that the body temperature and serum levels of rotavirus antigen were higher in the severe state. Serum antigen level was considered one of the factors affeting disease severity, but we did not check antigenicity in patient serum.
There are two methods for the scoring of disease severity of rotavirus gastroenteritis, which include the 20-point Vesikari scale9) and the 24-point Clark scale3). A severe state is defined as a score of more than 11 points on the Vesikari scale and more than 16 points on the Clark scale. Givon-Lavi et al. reported that only 35% of patients that were scored as being in the severe state by the Vesikari scale were also scored as severe by the Clark scale. On the contrary, severe states using the Clark scale were all scored as severe by the Vesikari scale. Therefore, the Clark scale can be considered more strict than the Vesikari scale to evaluate disease severity. Based on this, when the reports were compared, both scales needed to be considered. When we applied the results from Givon-Lavi et al.9) to our study, the percentage of the severe state by the Clark scale was estimated to be 21% of 143 patients. In the clinical study of Rotarix4), the change of the Vesikari scale was used as one of the variables for the evaluation of vaccine efficacy. In the RotaTeq study5), the change observed in the Clark scale was used.
We analyzed the differences observed in disease severity distribution dependent on VP7 and VP4 genotypes. However, G1P[8] was as high as 80.4% whereas the other genotype combination in each was less than 5%. We did not do further analysis on the severity distribution since it was considered to be less informative. Aupiais et al.14) reported that the difference in disease severity between the G1 and G9 serotype was not significant in their study. On the other hand, Linhares et al.15) reported more severe disease associated with serotype G9 in Latin America.
In our study, there was no correlation between disease severity and dehydration grade as a major complication of rotavirus gastroenteritis on admission. In view of disease severity, 37.8% of the cohort was mild or moderate whereas 62.2% was severe. In view of dehydration grade, 62.9% of the cohort was not dehydrated, whereas 18.9% was mild, 13.3% was moderate and 4.9% was severely dehydrated. This dissociation between disease severity and dehydration grade may be due to appropriate management of the patient by their parents in Korea, with higher quality of life and easier access to medical clinics, compared to other developing countries.
Similar to several reports16~18) from America, Europe and the Le et al.19) report in Seoul, G1P[8] was the most common genotype (80.4%) in our study (Table 2). On the other hand, Han et al.20) reported the most frequent combination of genotypes was G9P[8] (32.1%) followed by G1P[8] (20.7%) in Seoul. Bishop21) insisted that the efficacy of the two new vaccines for genotypes not included in these vaccines may be reduced. Genotypes not included in the new vaccines represented 9.4% in our study (Table 2).
Recently, reports indicated that the epidemic peak of rotavirus gastroenteritis moved to spring from the winter16,22). Our previous study23) also revealed a peak in spring. Rotavirus infection can cause afebrile convulsion18,19,24,25), but no such case was observed in our study. Nosocomial infection contributed to less than 1% of all rotavirus infected children26). In particular, nosocomial infections are problematic in neonates and G4P[6] is the major genotype that causes these infections27). However, these could not be analyzed in our study due to the small number of neonatal cases.
One limitation in our study was that the period of recruiting patients was too short and may not represent the change of genotype prevalance over many years. Another limitation was the exclusion for outpatients, which may cause higher disease severity scores than what actually occurs.
In conclusion, the most prevalent genotype combination of rotavirus was G1P[8] in our community. Genotypes not included in the new vaccines was 9.4%. Disease severity distribution of hospitalized children with rotavirus gastroenteritis was higher in the severe than in the mild and moderate categories.
Figures and Tables
 | Fig. 1Distribution of VP7 genotypes of Rotavirus isolated from 147 patients. G1 was the most common, identified in 116 patients (78.9%). |
References
1. Murphy TV, Gargiullo PM, Massoudi MS, Nelson DB, Jumaan AO, Okoro CA, et al. Intussusception among infants given an oral rotavirus vaccine. N Engl J Med. 2001. 344:564–572.

2. Vesikari T, Karvonen A, Puustinen L, Zeng SQ, Szakal ED, Delem A, et al. Efficacy of rix4414 live attenuated human rotavirus vaccine in finnish infants. Pediatr Infect Dis J. 2004. 23:937–943.

3. Clark HF, Bernstein DI, Dennehy PH, Offit P, Pichichero M, Treanor J, et al. Safety, efficacy, and immunogenicity of a live, quadrivalent human-bovine reassortant rotavirus vaccine in healthy infants. J Pediatr. 2004. 144:184–190.

4. Ruiz-Palacios GM, Perez-Schael I, Velazquez FR, Abate H, Breuer T, Clemens SC, et al. Safety and efficacy of an attenuated vaccine against severe rotavirus gastroenteritis. N Engl J Med. 2006. 354:11–22.

5. Vesikari T, Matson DO, Dennehy P, Van Damme P, Santosham M, Rodriguez Z, et al. Safety and efficacy of a pentavalent human-bovine (wc3) reassortant rotavirus vaccine. N Engl J Med. 2006. 354:23–33.

6. Gentsch JR, Laird AR, Bielfelt B, Griffin DD, Banyai K, Ramachandran M, et al. Serotype diversity and reassortment between human and animal rotavirus strains: Implications for rotavirus vaccine programs. J Infect Dis. 2005. 192:Suppl 1. S146–S159.

7. Santos N, Hoshino Y. Global distribution of rotavirus serotypes/genotypes and its implication for the development and implementation of an effective rotavirus vaccine. Rev Med Virol. 2005. 15:29–56.

8. Kim DS, Lee TJ, Kang JH, Kim JH, Lee JH, Ma SH, et al. Immunogenicity and safety of a pentavalent human-bovine (wc3) reassortant rotavirus vaccine in healthy infants in Korea. Pediatr Infect Dis J. 2008. 27:177–178.

9. Ruuska T, Vesikari T. Rotavirus disease in finnish children: Use of numerical scores for clinical severity of diarrhoeal episodes. Scand J Infect Dis. 1990. 22:259–267.

10. Gouvea V, Glass RI, Woods P, Taniguchi K, Clark HF, Forrester B, et al. Polymerase chain reaction amplification and typing of rotavirus nucleic acid from stool specimens. J Clin Microbiol. 1990. 28:276–282.

11. Gentsch JR, Glass RI, Woods P, Gouvea V, Gorziglia M, Flores J, et al. Identification of group a rotavirus gene 4 types by polymerase chain reaction. J Clin Microbiol. 1992. 30:1365–1373.

12. Givon-Lavi N, Greenberg D, Dagan R. Comparison between two severity scoring scales commonly used in the evaluation of rotavirus gastroenteritis in children. Vaccine. 2008. 26:5798–5801.

13. Sugata K, Taniguchi K, Yui A, Miyake F, Suga S, Asano Y, et al. Analysis of rotavirus antigenemia and extraintestinal manifestations in children with rotavirus gastroenteritis. Pediatrics. 2008. 122:392–397.

14. Aupiais C, de Rougemont A, Menager C, Vallet C, Brasme JF, Kaplon J, et al. Severity of acute gastroenteritis in infants infected by g1 or g9 rotaviruses. J Clin Virol. 2009. 46:282–285.

15. Linhares AC, Verstaeten T, Wolleswinkel-van den Bosch J, Clemens R, Breuer T. Rotavirus serotype G9 is associated with more-severe disease in Latin America. Clin Infect Dis. 2006. 43:312–314.

16. Mast TC, Walter EB, Bulotsky M, Khawaja SS, DiStefano DJ, Sandquist MK, et al. Burden of childhood rotavirus disease on health systems in the united states. Pediatr Infect Dis J. 2010. 29:e19–e25.

17. Iturriza-Gomara M, Dallman T, Banyai K, Bottiger B, Buesa J, Diedrich S, et al. Rotavirus surveillance in europe, 2005-2008: Web-enabled reporting and real-time analysis of genotyping and epidemiological data. J Infect Dis. 2009. 200:Suppl 1. S215–S221.

18. Payne DC, Staat MA, Edwards KM, Szilagyi PG, Gentsch JR, Stockman LJ, et al. Active, population-based surveillance for severe rotavirus gastroenteritis in children in the United States. Pediatrics. 2008. 122:1235–1243.

19. Le VP, Kim JY, Cho SL, Nam SW, Lim I, Lee HJ, et al. Detection of unusual rotavirus genotypes g8p[8] and g12p[6] in South Korea. J Med Virol. 2008. 80:175–182.

20. Han T, Kim C, Chung J, Park S, Hwang E. Genetic characterization of rotavirus in children in South Korea from 2007 to 2009. Arch Virol. 2010. 155:1663–1673.

21. Bishop R. Discovery of rotavirus: implications for child health. J Gastroenterol Hepatol. 2009. 24:Suppl 3. S81–S85.

22. Dey SK, Ushijima H, Phathammavong O, Chanit W, Okitsu S, Mizuguchi M, et al. Seasonal trend and serotype distribution of rotavirus infection in Japan, 1981-2008. Pediatr Infect Dis J. 2010. 29:166–167.

23. Kang KS, Kim JR. The pattern of occurrence of rotavirus gastroenteritis in Jeju area between 2001 and 2005. Korean J Pediatr Gastroenterol Nutr. 2005. 8:113–116.

24. Yang HR, Jee YM, Ko JS, Seo JK. Detection and genotyping of viruses detected in children with benign afebrile seizures associated with acute gastroenteritis. Korean J Pediatr Gastroenterol Nutr. 2009. 12:183–193.

25. Choi JH, Kim YJ, Oh JW, Kim CL, Yum MK, Sul IJ, et al. Genotype of rotavirus isolated from patients with rotaviral enteritis and neurological complications. Korean J Pediatr. 2006. 49:513–518.

26. Gleizes O, Desselberger U, Tatochenko V, Rodrigo C, Salman N, Mezner Z, et al. Nosocomial rotavirus infection in european countries: a review of the epidemiology, severity and economic burden of hospital-acquired rotavirus disease. Pediatr Infect Dis J. 2006. 25:S12–S21.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download