Abstract
Plain X-ray radiographs are the first line of investigation taken in the diagnosis of abdominal pathology and are considered an important diagnostic tool to provide guidelines for further imaging studies and comprehensive therapeutic management. Although most abdominal pathology demonstrates non-specific radiologic findings, the plain abdominal radiography is very useful in specific diseases, including certain gastrointestinal anomalies. This review provides image findings of normal plain abdominal radiography and some common abdominal pathology in infants and children.
Although there are a variety of recent, highly advanced imaging techniques available, plain X-ray radiographs are still important and commonly used as the first line of investigation in the diagnosis of abdominal pathology. They can be used as definitive diagnostic tools or as early indicators to guide further investigations.
The aim in pediatric radiology is to obtain the required diagnostic information using the minimum radiation dosage. For instance, the well-known double-bubble sign is diagnostic of duodenal atresia without the need for further radiologic investigation. Plain X-ray radiographs can suggest the presence of pyloric stenosis, intussusception, ileus, obstruction, pathologic calcification, and masses. They also provide information on intramural air, portal venous air, and free intraperitoneal air secondary to intestinal perforation. It is important for the pediatrician to be familiar with normal findings of plain X-ray radiographs in infants and young children that are different from those in adults. This study also reviews normal abdominal radiographic findings and those of common diseases in infants and young children.
Supine and upright views are obtained in any radiographic evaluation of the abdomen. If the patient is too young or sick to stand, then in place of the upright view a left lateral decubitus view or cross-table lateral view is obtained. Left-side-down decubitus and upright views are used to evaluate free intraperitoneal air and air-fluid levels. A cross-table lateral view is available for the evaluation of free intraperitoneal air in the neonate with immobilization state1~3).
Plain radiography demonstrates three categorical structures that consist of soft tissue, air and bony or calcification densities according to the X-ray absorption coefficient.
The borders of soft tissue structures including the liver, spleen, kidneys, psoas muscles, bladder, muscles and peritoneum can often be identified by the fat that surrounds them. The liver is located in the right upper quadrant, whereas the spleen and stomach are located in the left upper quadrant (Fig. 1A). Hepatomegaly can be identified with a bulging contour of the liver tip below the 12th rib on supine view. Because there is insufficient perihepatic fat in neonates and infants, it is difficult to identify the hepatic outline on plain radiography. The appearance of the stomach varies, depending on the position of the child (for example supine versus upright) and the degree of gastric distension. On upright images, air moves to the fundus, which is below the diaphragms, medial to the splenic shadow (Fig. 1A). On supine views, the stomach is outlined by air within the more anterior antrum. Distension of the stomach is normal after a full meal but is abnormal if the patient presents with a history of vomiting. The enlarging spleen may displace the gastric air bubble medially. The enlarging spleen may also displace the splenic flexure of the colon caudally and medially, and there may be elevation of the left hemidiaphragm (Fig. 2). A portion of each upper renal pole usually extends above the 12th rib, with the right kidney normally slightly lower than the left due to the position of the liver. The vertical axis of the kidney should be parallel to the upper one-third of the psoas muscle. Obliteration of the psoas outlines and renal outlines is extremely nonspecific. Asymmetric visualization of the psoas margin occurs commonly and usually is due to anatomic variations, scoliosis, and intraperitoneal (such as appendicitis) as well as retroperitoneal pathology1~3).
Air is the inherent contrast medium in plain diagnosis and gas pattern in the abdomen can be most useful for assessing gut anatomical and functional status. Relatively large amounts of gas are normally present in the stomach and colon but only a small amount is usually seen in the small bowel. It is usual to be able to identify the gastric rugae on a supine radiograph (Fig. 1B). There is rarely sufficient gas present in the small bowel to outline more than a short length, and although the mucosal pattern may be seen, the thin bands of the valvular conniventes are seldom identified in a normal patient. Air and fluid are normal contents of the small bowel, and short fluid levels are not abnormal on an erect radiograph. The colon is easily identified by haustra, larger caliber than the small bowel loops and its peripheral and posterior location. The amount of gas present in a normal colon is extremely variable, from almost none to what may appear to be abnormal gaseous distension. Sufficient gas is usually present for colonic haustra to be identified readily. Large-bowel caliber is very variable, and there is a considerable overlap between the normal and abnormal. Fluid levels are common in normal people, and usually lie in the colon. Three to five small fluid levels may be seen, particularly in the right lower quadrant, without any evidence of intestinal obstruction or paralytic ileus.
Finally, the bony structures need to be carefully examined, especially in a very young patient, who can have difficulty in expressing precisely where the pain is originating from. Vertebral body, disk space heights, spinal alignment, and pedicle size are to be checked with regards to the skeleton on the abdominal radiography.
The normal bowel gas pattern in neonates is quite different from that seen in older children and adults. Gas is usually present in the stomach within 10 to 15 minutes after birth. Gas normally reaches the proximal small bowel within an hour and fills most of the small bowel by 6 hours. The large bowel is filled by 12~14 hours, often with the passage of meconium2,3).
The normal bowel gas pattern in neonates is characterized by gas throughout the small and large bowels and little fluid with respect to air. The bowel air interfaces are thin and sharp. The gas distribution is one of multiple, closely apposed, rounded or polyhedral structures. The small and large bowel cannot be distinguished (Fig. 3). The large and small bowel may be differentiated on lateral views because the ascending and descending parts of the colon overlie the spine, whereas the small bowel is more anterior.
Free intraperitoneal gas due to hollow viscus perforation is identified on the erect or cross-table lateral view under the diaphragm or under the anterior abdominal wall. In infants and young children a cross-table lateral view (Fig. 4A) is preferred to an erect view. On supine view it may be identified by the presence of air on both sides of the bowel wall or air outlining the ligamentum falcifarum (Fig. 4B), and can also be seen as the 'football' sign (Fig. 4B)2,3).
Plain radiographs are also crucial in the early diagnosis and management of neonatal necrotizing enterocolitis. At the time of diagnosis, plain abdominal radiography must include one image obtained using a vertical beam with the patient supine and a second image obtained with a cross-table lateral view. The main observations to be made on the plain abdominal radiograph relate primarily to the presence, amount, and distribution of gas, which include intraluminal gas, intramural gas (pneumatosis cystoides intestinalis), portal venous gas (air-portograms) (Fig. 6), and free intraperitoneal gas. From observations of the intraluminal gas, it may sometimes be possible to make inferences regarding the presence of bowel wall thickening, free fluid, and focal fluid collections4).
In adynamic or paralytic ileus, which can be clinically and radiologically very difficult to distinguish from obstruction in children, the bowel is typically less distended, the fluid levels are long and there is gas through the bowel. Ileus is characterized by uniform dilatation of bowel to the level of the rectum. It is a non-specific finding and is present in medical disorders, such as sepsis, electrolyte imbalance and also most commonly in children with enterocolitis (Fig. 8).
Mechanical obstruction, on the other hand, leads to differential bowel dilatation. There is dilatation of the loops proximal to the point of obstruction, with characteristic collapse of points distal to the obstruction. In obstruction, fluid levels are short and on an erect film the gas pattern is often described as a "ladder pattern" (Fig. 9). In closed-loop obstruction the affected bowel may become completely fluid filled with the absent of air-fluid levels5).
The level or cause of obstruction in neonates and young infants may be suspected by associated findings such as a bubbly pattern produced by meconium ileus, calcification following meconium peritonitis, gas collected within a hernia sac, or gas in the bladder from a high anorectal malformation4).
Positive findings will include the presence of a faecolith in the right lower quadrant present in approximately 30% of cases, and a localized ileus with mildly dilated loops of bowel. A scoliosis is often present, concave to the right. There may be loss of the psoas outline but this is not a specific sign of appendicitis as loss of psoas outline can occur with rotation of a radiograph (Fig. 10)1~3).
The most common finding of
intussusception is a soft-tissue mass, which is most often seen in the right upper quadrant effacing the adjacent hepatic or renal contour. Other signs include reduced air in the small intestine or a gasless abdomen and variable degree of small intestine obstruction. The most specific plain radiographic findings are the 'target' sign and 'meniscus' sign. The 'target' sign consists of a soft-tissue mass that contains concentric circular or nearly circular areas of lucency, which are due to the mesenteric fat of the intussusceptum. The mass is most often seen in the right upper quadrant projecting over the right kidney. The 'meniscus' sign consists of a crescent of gas within the colonic lumen that outlines the apex of the intussusception (the intussusceptum) (Fig. 11). Identification of a cecum filled with gas or feces in the normal location is the finding that allows exclusion of intussusception with the most confidence5,6).
Although most abdominal pathology demonstrates nonspecific radiologic findings, plain abdominal radiography is very useful in the diagnosis of certain gastrointestinal anomalies, intestinal obstruction, intramural air, free peritoneal air secondary to intestinal perforation, pathologic calcification, and masses large enough to displace normal structures. Plain abdominal radiographs also provide a guideline for further imaging studies and better therapeutic management in children.
Figures and Tables
Fig. 1
Erect (A) and supine (B) views of the abdominal radiography in a normal child (thin arrows: kidney, thick arrow: psoas shadow).
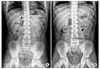
Fig. 2
Splenomegaly. The enlarging spleen (arrows) in the left upper quadrant displaces the splenic flexure of the colon caudally and medially, and the stomach medially.

Fig. 3
Supine view of a normal neonate. The gas distribution is present throughout the small and large bowel and is one of multiple, closely apposed, rounded or polyhedral structures. The small and large bowel cannot be distinguished.

Fig. 4
Pneumoperitoneum. The gas is under the anterior abdominal wall (short arrows) and the ligamentum falcifarum is demonstrated (long white arrow) on a cross table lateral view (A). Supine view (B) shows a large oval air collection (long black arrows) in the central abdomen with the shape of a 'football'. It may be identified by the presence of air on both sides of the bowel wall (short black arrows) or air outlining the ligamentum falcifarum (long white arrows).

Fig. 5
Ascites in a neonate with meconium peritonitis. Supine view demonstrates separation of the flank fat stripe (long arrows) from gas in the descending colon (short arrow) and central displacement of bowel loops.
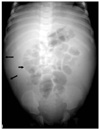
Fig. 6
Necrotizing enterocolitis. Supine view shows diffusely dilated bowels with linear intramural gases (short arrows) (pneumatosis cystoides intestinalis) and also multiple linear and branching airs (long arrows) in the liver (air-portogram).

Fig. 7
Hypertrophic pyloric stenosis. Supine view demonstrates over distension of the stomach and evidence of a peristaltic wave (arrow) along the gastric body. Note the relatively sparse bowel gas.

Fig. 8
Adynamic ileus with gastroenteritis. The fluid levels tend to be long and are the same level on an erect view. Note gases in both colon and small bowel loops.

Fig. 9
Mechanical small bowel obstruction. Erect view shows absent colon gas and multiple different air-fluid levels in the dilated small bowel loop with a 'ladder' appearance.

Fig. 10
Appendicitis with an appendicolith. Supine view illustrates the presence of a faecolith in the right lower quadrant (short arrows) and loss of the right psoas outline (long arrows). Note normal well-defined left psoas shadow.

Fig. 11
Intussusception with the 'target' and 'meniscus' signs. Supine view shows a round soft-tissue mass in the right upper quadrant. The mass contains a ring-like area of lucency representing the 'target' sign (small arrows). The mass protrudes into the gas-filled transverse colon representing the 'meniscus' sign (long arrows).

References
1. Coley BD, Hernans-Schulman M. Slovis TL, editor. The abdomen, pelvis, retroperitoneum. Caffey's pediatric diagnostic imaging. 2008. 11th ed. Philladelphia: Mosby;1759–2464.
2. String DA. Carty H, Brunelle F, Stringer DA, Kao SCS, editors. The gastrointestinal tract. Imaging children. 2005. 2nd ed. Philadelphia: Elsevier Ltd;1289–1529.
3. Swichuk LE. Imaging of the newborn, infant, and young child. 2004. 5th ed. Philadelphia: Lippncott Williams and Wilkins;539–589.
4. McAlister WH, Kronemer KA. Emergency gastrointestinal radiology of the newborn. Radiol Clin North Am. 1996. 34:819–844.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download