Abstract
Isolated pancreatic trauma and secondary obstructive jaundice in the pediatric population is unusual. Biliary tract obstruction can be a major cause of acute pancreatitis. We report a case of obstructive jaundice secondary to isolated traumatic acute pancreatitis in a previously healthy 32-month-old girl. In our case, secondary obstructive jaundice aggravated the pancreatic inflammation and was successfully treated with percutaneous transhepatic biliary drainage (PTBD).
Figures and Tables
Fig. 1
Whole abdominal computed tomography was performed on admission (A, B) showing diffuse pancreatic swelling and peripancreatic fluid collection (arrows), a relatively intact common bile duct (solid arrow), and a part of the gallbladder (dotted arrow), and 10 days after admission (C) showing intra- and extra-hepatic biliary duct dilatation (arrow) and milder pancreatic swelling and a decreased amount of peripancreatic fluid collection than before.

Fig. 2
Magnetic resonance cholangiopancreaticography was performed 28 days after admission showing a distended gallbladder, dilated biliary trees, and pancreatic duct (dotted arrow) and low signal lesion suggestive of a biliary stone in the distal common bile duct (solid arrow) and biliary sludge in the gallbladder.
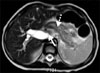
Fig. 3
Cholangiograms through the percutaneous transhepatic biliary drainage catheter were performed 33 days after admission (A) showing marked dilated intra- and extra-hepatic bile ducts, and a smooth, tapering biliary stricture in the distal common bile duct (solid arrow), and 35 days after admission (B) showing a mild dilated pancreatic duct and a filling defect (dotted arrow) in the distal common bile duct suggestive of a biliary stone which was removed by a skilled interventional radiologist via a stone basket and shown to be a small amount of biliary sludge, and 66 days after admission (C) showing no biliary dilatation or stricture of the common bile duct with free flow of contrast media from the common bile duct to the second portion of the duodenum.

References
1. Lopez MJ. The changing incidence of acute pancreatitis in children: a single-institution perspective. J Pediatr. 2002. 140:622–624.

2. Werlin SL, Kugathasan S, Frautschy BC. Pancreatitis in children. J Pediatr Gastroenterol Nutr. 2003. 37:591–595.

3. Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, Shackford SR, Champion HR, et al. Organ injury scaling. Surg Clin North Am. 1995. 75:293–303.

5. Mattix KD, Tataria M, Holmes J, Kristoffersen K, Brown R, Groner J, et al. Pediatric pancreatic trauma: predictors of nonoperative management failure and associated outcomes. J Pediatr Surg. 2007. 42:340–344.

6. Benifla M, Weizman Z. Acute pancreatitis in childhood analysis of literature data. J Clin Gastroenterol. 2003. 37:169–172.
7. Wood JH, Partrick DA, Bruny JL, Sauaia A, Moulton SL. Operative vs nonoperative management of blunt pancreatic trauma in children. J Pediatr Surg. 2010. 45:401–406.

8. Dryburgh PR, White JAM. Late obstruction of the intrahepatic common bile duct after seat-belt injury. S Afr Med J. 1980. 58:534–535.
9. Choi BH, Lim YJ, Yoon CH, Kim EA, Park YS, Kim KM. Acute pancreatitis associated with biliary disease in children. J Gastroenterol Hepatol. 2003. 18:915–921.

10. Ko JS. Fibrosing pancreatitis causing obstructive jaundice. Korean J Gastroenterol. 2008. 52:271–272.
11. Yachha SK, Chetri K, Saraswat VA, Baijal SS, Sikora SS, Lal R, et al. Management of childhood pancreatic disorders: a multidisciplinary approach. J Pediatr Gastroenterol Nutr. 2003. 36:206–212.

12. Sylvester FA, Shucktt B, Cutz E, Durie PR, Marcon MA. Management of fibrosing pancreatitis in children presenting with obstructive jaundice. Gut. 1998. 43:715–720.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download