Abstract
Purpose
Stiffness in the first metatarsophalangeal joint after surgery for hallux valgus has been reported. The goal of this study was to test the efficacy of releasing plantar aponeurosis for improving the range of extension in the first metatarsophalangeal joint that was limited after hallux valgus surgery.
Materials and Methods
Thirteen patients (1 man, 12 women [17 feet]; median age, 54.4 years; range, 44~69 years) with limited first metatarsophalangeal joint extension after hallux valgus surgery, who underwent an additional procedure of plantar aponeurosis release between March 2015 and August 2015, were included. Subsequently, the passive range of extension in the first metatarsophalangeal joint was evaluated via knee extension and flexion positions. Hallux valgus angle, inter-metatarsal angle, distal metatarsal articular angle, and talo-first metatarsal angle were measured on weightbearing dorsoplantar and lateral radiographs of the foot preoperatively.
Results
The mean range of extension for the first metatarsophalangeal joint improved significantly, from 2.5° to 40.9° in the knee extension position (p<0.00). The mean extension range for the first metatarsophalangeal joint also improved, from 18.2° to 43.2° in the knee flexion position (p<0.00). In all patients, congruence of the first metatarsophalangeal joint was recovered.
Hallux valgus is one of the common foot deformities with a reported prevalence of 23%~35.7% among adults.1) Multiple procedures have been described for treating hallux valgus,23) with the goal of correcting all pathologic elements, which is critical for recovering the biomechanical function of hallux.456)
Appropriate surgical treatment resulted in beneficial outcomes in 85% of patients7); however, recurrence, malunion, hallux varus and implant failure have been described as common complications after hallux valgus surgery.89) Even though stiffness of the first metatarsophalangeal joint (1MTP) is not a common complication, Kernozek and Sterriker10) reported reduced dorsiflexion range of motion at 1MTP as one of the complications after hallux valgus surgery. During propulsion, 1MTP was reported to dorsiflex between 40° and 60° during typical gait.11) A limitation in this extension affects normal gait pattern and leads to pain even if medial eminence pain is reduced, despite satisfactory correction of deformities and restoration of 1MTP congruence after hallux valgus surgery. Possible causes of stiffness in 1MTP after surgery for hallux valgus include the first metatarsal elevation, intra-capsular adhesion, and tightness of the gastrocnemius-plantar aponeurosis complex.101213) However, only a few clinical studies have investigated these issues and no clinical resolution has been reported as yet.
We hypothesized that tightness of the gastrocnemius-plantar aponeurosis complex is one of the factors that limits the extension of 1MTP after hallux valgus surgery. Thus, an additional procedure of the plantar aponeurosis release during hallux valgus surgery may improve the range of extension at 1MTP. The purpose of this study was to test the efficacy of the simultaneous procedure of plantar aponeurosis release in improving the range of extension when it is limited during hallux valgus surgery.
Thirty-eight patients (46 feet) with hallux valgus were operated at Inje University Haeundae Paik Hospital between March 2015 and August 2015. Among them, 13 patients (1 man, 12 women [17 feet]; median age, 54.4 years; range, 44~69 years) underwent an additional procedure of plantar aponeurosis release as their 1MTP extension was limited after hallux valgus surgery. The inclusion criterion was restricted 1MTP extension showing more than 15° of difference between the knee extension and flexion positions, measured after completing all procedures of the hallux valgus surgery. Cases with revised surgery of hallux valgus, osteoarthritis of 1MTP, history of trauma, infection, rheumatoid arthritis, seronegative spondyloarthropathy or gout were excluded. The approval for this study was obtained from Inje University Haeundae Paik Hospital's Institutional Review Board and informed consent was obtained from all patients.
The passive range of 1MTP extension was evaluated by a goniometer assuming a weightbearing position with knee 0° of extension and 30° of flexion while, supporting the first metatarsal head with a palm, measured after completing all procedures of the hallux valgus surgery including distal soft tissue release, corrective osteotomy and internal fixation, and before plantar aponeurosis release, respectively (Barouk test).12) In previous literature, the Barouk test was described as positive when the difference in range of 1MTP extension was over 14° between knee extension and flexion,14) and thus, in this study we chose a reference value of 15°. A Silfverskiold test15) was performed to test tightness of gastrocnemius in all cases preoperatively. It was considered positive if the ankle could not be neutral when the knee was extended but would dorsiflex to or beyond neutral alignment with the knee flexed, or if ankle dorsiflexion reached 90° with knee extension and increased about 15° to 20° with knee flexion.15161718) We measured the angle between the shaft of the fibula and lateral border of the foot by a goniometer.
The radiographic assessments were performed using weight-bearing dorsoplantar and lateral radiographs of the foot preoperatively. All preoperative radiographs were obtained in the digital form, through the Picture Archiving Communication System (Marosis Enterprise PACS; Infinitt, Seoul, Korea). On the dorsoplantar radiographs of the weightbearing foot, hallux valgus angle (HVA), intermetatarsal angle (IMA) and distal metatarsal articular angle (DMAA) were measured, while on the lateral radiographs, the talo-first metatarsal angle (TMA) was measured. The HVA was defined as the angle created by intersection of the mechanical axes of first metatarsal and proximal phalanx on a dorsoplantar radiograph. The IMA was defined as the angle created by intersection of the mechanical axes of the first metatarsal and the second metatarsal on a dorsoplantar radiograph. The DMAA was defined as the angle between the perpendicular line to the mechanical axis of first metatarsal and the connecting line between the most medial and lateral extent of the first metatarsal distal articular surface on a dorsoplantar radiograph. The normal range of DMAA was considered from 0° to 7° and the congruity of 1MTP was confirmed by this range in this study.2) The TMA was measured between the long axis of talus (which extended from the mid-height of talar body through the mid-diameter of talonavicular joint), and the mechanical axis of first metatarsal on a lateral radiograph. If this angle was more than 10°, the case was considered as a flatfoot deformity in this study. At post surgery, correction of the HVA, IMA and congruence of 1MTP were confirmed by the nonweightbearing dorsoplantar and lateral radiograph of the foot by C-arm (ARCADIS Varic; Siemens AG, Munich, Germany).
A thigh tourniquet was inflated to 300 mmHg under spinal anaesthesia. A medial longitudinal skin incision was created, centred over the 1MTP. A second longitudinal incision was created over the joint capsule and the first metatarsal, exposing the 1MTP. After medial eminence was excised, the lateral joint capsule of 1MTP and the adductor hallucis tendon were released through the under surface of first metatarsal head. Subsequently, restoration of 1MTP congruence with minimal force was confirmed after distal soft tissue release. In cases of IMA less than 15°, distal chevron osteotomy was performed and one 1.6 mm-diameter Kirschner wire (K-wire) was fixed (Fig. 1A). In contrast, proximal reverse chevron osteotomy along with fixation of two 1.6 mm-diameter K-wires was performed in cases of IMA more than 16° (Fig. 1B). In all the remaining cases, medial closing wedge osteotomy of the proximal phalanx (Akin procedure) and fixation of one 1.4 mm-diameter K-wire were performed. Correction of the HVA, IMA and congruence of 1MTP were confirmed by C-arm. Wound closure was performed without tightening the medial joint capsule. Additional procedures of plantar aponeurosis release were performed after verifying the limitation of 1MTP extension >15° while, supporting the first metatarsal head with a palm, and assuming a weightbearing position with knee 0° of extension (Fig. 2A). For this procedure, a 2 cm-longitudinal skin incision over the medial tuberosity of the calcaneus origin site of the plantar aponeurosis was made. Dissection was performed precisely to avoid any injuries at the medial calcaneal nerve branch and calcaneal origin of plantar aponeurosis was exposed. At 1 cm distal from the origin, medial half of plantar aponeurosis was excised using No. 15 blade or metzenbaum scissors (Fig. 3). After partial release of the plantar aponeurosis, it was elongated by passive stretching with maximal force. The wound was closed after confirming the improved range of 1MTP extension (Fig. 2B).
Statistical analysis of the range of 1MTP extension range between pre- and post-plantar aponeurosis release was performed using the Wilcoxon signed rank test. All statistical analyses were performed using IBM SPSS Statistics version 22.0 (IBM Co., Armonk, NY, USA). A p-value <0.05 was considered statistically significant.
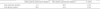
The mean range of 1MTP extension was examined under anesthesia during the operation. The mean range of 1MTP extension significantly improved from 2.5° to 40.9° in the knee extension position (p<0.00). The mean range of the 1MTP extension also improved from 18.2° to 43.2° in the knee flexion position (p<0.00) (Table 1). The Silfverskiold test was positive in 12 cases. The mean HVA, IMA, and DMAA respectively changed from 34.8°, 16.9°, and 19.6° preoperatively to 4.3°, 0.4°, and 3.7° postoperatively. In all patients, congruence of 1MTP was recovered based on DMAA (range, 1°~5°). Preoperative mean TMA was 18.3° (range, 5°~30°), and it was over 10° in 12 cases. There were no surgery-related complications such as plantar aponeurosis rupture or nerve injury.
We speculated that contracture of the gastrocnemius-plantar aponeurosis complex was one of the causes of restricted 1MTP extension after hallux valgus surgery, even though the correction of HVA and IMA and recovery of 1MTP congruence were achieved successfully. Gastrocnemius-plantar aponeurosis complex undergoes gastrocnemius-soleus complex (GSC), Achilles tendon and plantar aponeurosis running distally.1920) In case of hallux valgus, medial band of the central component of plantar aponeurosis, which acts like a bow string, moves plantarly and laterally.12) In this system, the plantar aponeurosis acts as a critical biomechanical link between GSC and hallux1920) because the calcaneus transmits effects of GSC shortening to the plantar aponeurosis, and posterior tuberosity of the calcaneus attaching to both, the Achilles tendon and the plantar aponeurosis.21) Thus, tightness of the GSC contributes to increased tension at the plantar aponeurosis, resulting in limitation of the 1MTP extension, possibly because of its anatomical structure.2021) Several non-English articles22232425) have reported that the limitation in 1MTP extension is related to gastrocnemius tightness because of the anatomic connection between the gastrocnemius and hallux. In this study, we observed a significant improvement in 1MTP extension by performing plantar aponeurosis release in cases with a limitation after hallux valgus surgery.
Kowalski et al.26) have reported that, a reduction in 1MTP extension is caused by an activating windlass mechanism which is induced by the increased tension of plantar aponeurosis in the weightbearing position, and such a phenomenon of relaxation at the plantar aponeurosis is not observed in the nonweightbearing position. Laird14) explains this phenomenon as a concept of functional hallux limitus. Functional hallux limitus is described as the inability of 1MTP extension during gait, even though normal motion is present during the nonweightbearing examination.27) Contracture of the gastrocnemius increases tensile force at the plantar aponeurosis because the knee is extended to support the limb while, the opposite is swinging during stance phase.28) In this study, a limitation of 1MTP extension was presented definitely while supporting the first metatarsal head with the contralateral palm, assuming the weightbearing position. We believed that, this was also a type of functional hallux limitus that occurred because of increased tension at the plantar aponeurosis.
The Silfverskiold test is usually performed to test the tightness of gastrocnemius. On the other hand, as the Barouk test is a combination of the test for functional hallux limitus with the Silfverskiold test,28) it represents a correlation between the bi-articular component of the GSC and plantar aponeurosis. Thus, a positive of the Barouk test can be resulted from either a) tightness of the gastrocnemius, or b) tightness of the plantar aponeurosis by increased windlass mechanism or c) both.28) In this study, the Silfverskiold test was positive in 12 cases with flatfoot deformities. The fact that most flatfoot deformities are accompanied with tightness of gastrocnemius is well known.1826) In these 12 cases, we couldn't predict if the main source of restricted 1MTP extension after hallux valgus surgery was either tightness of the GSC or tightness of the plantar aponeurosis resulting from tightness of the GSC. Furthermore, which of these possible mechanisms was responsible for the postoperative stiffness of 1MTP was also un-determined. However, we could predict that the main source of limitation in the 1MTP extension was tightness of the plantar aponeurosis in a different set of 5 cases. In this study, clinical improvements in the 1MTP extension after release of the plantar aponeurosis were observed in these 12 cases with a positive Silfverskiold test. These results suggested that tightness of the GSC might cause plantar aponeurosis tightness because of the anatomical structure of gastrocnemius-plantar aponeurosis complex. However, a combination of gastrocnemius and plantar aponeurosis release, which would be more effective in gaining an improved extension of 1MTP, also remained to be established.
This study has several limitations, with the first one being a small number of cases. All cases of hallux valgus did not present stiffness after hallux valgus surgery, regardless of the accompanying flatfoot deformity, suggesting that stiffness resulted due to more than one causative factors as investigated in this study. Thus, further investigations are needed to address the unknown mechanisms. The second limitation is the absence of follow-up. This study was designed to immediately test the range of motion in the 1MTP after hallux valgus surgery alone or perform an additional procedure of plantar aponeurosis release to test its efficacy. Serial follow-ups to test if the improved range of motion is maintained would be valuable. Lastly, this study is not a comparative study. In cases with presentation of the GSC contracture, comparisons between plantar aponeurosis release and GSC release would be meaningful.
Our study supports tightness of the gastrocnemius-plantar aponeurosis complex is one of the factors that limits the extension of 1MTP after hallux valgus surgery. Hence, plantar aponeurosis release can be considered as an effective additional procedure to improve the range of 1MTP extension when a limitation is presented after hallux valgus surgery.
Figures and Tables
 | Figure 1(A) In cases of intermetatarsal angle (IMA) less than 15°, distal chevron osteotomy was performed and one 1.6 mm-diameter Kirschner wire (K-wire) was fixed. (B) In cases of IMA more than 16°, proximal reverse chevron osteotomy was performed and two 1.6 mm-diameter K-wire was fixed. |
 | Figure 2(A) This photo presented limitation of first metatarsophalangeal joint (1MTP) extension while, supporting the first metatarsal head with a palm, and assuming a weightbearing position with knee 0° of extension after finishing all of the procedures for hallux valgus surgery. (B) This photo presented improvement of 1MTP extension after partial release of the plantar aponeurosis with same position. |
 | Figure 3(A) After longitudinal skin incision over the medial tuberosity of the calcaneus was made, dissection was performed precisely to avoid any injuries at the medial calcaneal nerve branch and calcaneal origin of plantar aponeurosis was exposed. (B) Further dissection was performed to separate plantar aponeurosis from abductor hallucis muscle using freer elevator. (C) At 1 cm distal from the origin of plantar aponeurosis, medial half of the plantar aponeurosis was cut using metzenbaum scissors. (D) After partial release of the plantar aponeurosis, it was elongated by passive stretching with maximal force. |
References
1. Nix S, Smith M, Vicenzino B. Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res. 2010; 3:21.

2. Richardson EG, Graves SC, McClure JT, Boone RT. First metatarsal head-shaft angle: a method of determination. Foot Ankle. 1993; 14:181–185.

3. Robinson AH, Limbers JP. Modern concepts in the treatment of hallux valgus. J Bone Joint Surg Br. 2005; 87:1038–1045.

4. Easley ME, Trnka HJ. Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int. 2007; 28:748–758.

5. Klosok JK, Pring DJ, Jessop JH, Maffulli N. Chevron or Wilson metatarsal osteotomy for hallux valgus. A prospective randomised trial. J Bone Joint Surg Br. 1993; 75:825–829.

6. Thompson FM. Complications of hallux valgus surgery and salvage. Orthopedics. 1990; 13:1059–1067.

7. Wülker N, Mittag F. The treatment of hallux valgus. Dtsch Arztebl Int. 2012; 109:857–867. quiz 868.

8. Baravarian B, Ben-Ad R. Revision hallux valgus: causes and correction options. Clin Podiatr Med Surg. 2014; 31:291–298.
9. Schuh R, Willegger M, Holinka J, Ristl R, Windhager R, Wanivenhaus AH. Angular correction and complications of proximal first metatarsal osteotomies for hallux valgus deformity. Int Orthop. 2013; 37:1771–1780.

10. Kernozek TW, Sterriker SA. Chevron (Austin) distal metatarsal osteotomy for hallux valgus: comparison of pre- and post-surgical characteristics. Foot Ankle Int. 2002; 23:503–508.

11. Hetherington VJ, Johnson RE, Albritton JS. Necessary dorsiflexion of the first metatarsophalangeal joint during gait. J Foot Surg. 1990; 29:218–222.
12. Barouk LS. The effect of gastrocnemius tightness on the pathogenesis of juvenile hallux valgus: a preliminary study. Foot Ankle Clin. 2014; 19:807–822.

13. Jones RO, Harkless LB, Baer MS, Wilkinson SV. Retrospective statistical analysis of factors influencing the formation of long-term complications following hallux abducto valgus surgery. J Foot Surg. 1991; 30:344–349.
14. Laird PO. Functional hallux limitus. Illinois Podiatrists. 1972; 9:4.
15. Silfverskiold N. Reduction of the uncrossed two-joints muscles of the leg to one-joint muscles in spastic conditions. Acta Chir Scand. 1924; 56:315–330.
16. Abbassian A, Kohls-Gatzoulis J, Solan MC. Proximal medial gastrocnemius release in the treatment of recalcitrant plantar fasciitis. Foot Ankle Int. 2012; 33:14–19.

17. Barouk LS, Barouk P, Toulec E. Resulltats de la liberation proximale des Gastrocnemiens [Results of proximal gastrocnemius release]. Paper presented at: Etude Prospective Symposium Brièveté des gastrocnémiens symposium journees de Printemps SFMCP-AFCP, Toulouse. Med Chir Pied. 2006; 22:151–156.
18. De los Santos-Real R, Morales-Muñoz P, Payo J, Escalera-Alonso J. Gastrocnemius proximal release with minimal incision: a modified technique. Foot Ankle Int. 2012; 33:750–754.

19. Sarrafian SK. Anatomy of the foot and ankle. 2nd ed. Philadelphia: Lippincott William & Wilkins;1993.
20. Snow SW, Bohne WH, DiCarlo E, Chang VK. Anatomy of the Achilles tendon and plantar fascia in relation to the calcaneus in various age groups. Foot Ankle Int. 1995; 16:418–421.

21. Arandes R, Viladot A. Biomecanica del Calcaneo. Med Clin. 1954; 21:21–25.
22. Barouk LS, Barouk P. Hallux valgus et Gastrocnemiens courts: étude de deux series cliniques. Brièveté des gastrocnémiens. Montpellier (France): Sauramps;2012. p. 265–268.
23. Drakos MC, DiGiovanni CW. Importance de la brièveté isolée des gastrocné-miens dans la pathologie du pied. Brièveté des Gastrocnémiens: de l'anatomie au traitement. Montpellier (France): Sauramps;2012. p. 231–240.
24. Maceira E, Orejana A. Hallux limitus fonctionnel et le système suro- Achilleoplantaire Brièveté des gastrocnémiens. De l'anatomie au traitement. Montpellier (France): Sauramps;2012. p. 147–194.
25. Pascual Huerta J. Brièveté des gastrocnémiens et son effet sur l'aponévrose plantaire et le comportement sagittal. Brièveté des gastrocnémiens de l'anatomie au traitement. Montpellier (France): Sauramps;2012. p. 119–140.
26. Kowalski C, Diebold P, Pennecot GF. Le tendon Calcaneen court. Paris: Encyclopedie medico Chirurgicale Elsevier;1999. p. 27–60.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download