Abstract
Figures and Tables
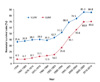 | Figure 1Changes of neonatal survival rates for very low birth weight infants (VLBWI) and extremely low birth weight infants (ELBWI) in Korea (1960-2014 June) (From Shim JW, et al. J Korean Med Sci 2015;30 Suppl 1:S25-S34, according to the Creative Commons license) [3]. |
 | Figure 2Changes of neonatal survival rates by gestational period in Korea (2002-2014 June). *P<0.015, 2007 vs. 2002; †P<0.015, 2009 vs. 2002; ‡P<0.015, 2013-2014.6 vs. 2002 (From Shim JW, et al. J Korean Med Sci 2015;30 Suppl 1:S25-S34, according to the Creative Commons license) [3]. |
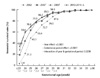
 | Figure 3Comparison of neonatal survival rate in Korea, Japan, Europe, Canada, and Autralia-New Zealand by very low birth weight infants (VLBWIs) and extremely low birth weight infants (ELBWIs). *P<0.05 comparison to the Korean Neonatal Network (KNN) reference birth weight specific survival rates. NRNJ, Neonatal Research Network of Japan [12]; CNN, Canadian Neonatal Network [13]; AZN, Australia-New Zealand Neonatal Network [14]; EuroNeo-Net, European Neonatal Network [15] (From Shim JW, et al. J Korean Med Sci 2015;30 Suppl 1:S25-S34, according to the Creative Commons license) [3]. |
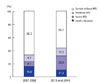 | Figure 4Changes of the rate of death before 36 weeks, survival with bronchopulmonary dysplasia (BPD) or survival without BPD at 36 weeks postmenstrual age (PMA) from 2013 to mid 2014 compared to 2007 to 2008 [10] among very low birth weight (VLBW) infants born at 23 to 31 weeks of gestation. In total, 1,990 VLBW infants were compared to 3,841 VLBW infants from the nationwide survey in 2007 to 008 [18]. The distribution of the overall rate of the three possible outcomes at 36 weeks PMA were different compared to that in the survey from 2007 to 2008 [18] using the chi-square test (P<0.001). The incidence of BPD increased by 85% (from 17.8% to 33.0%); the rate of severe BPD increased by 157% (from 8.1% to 20.8%); the rate of death before 36 weeks' PMA decreased by 28.9% (from 15.9% to 11.3%) compared to the retrospective survey in 2007 to 2008 [18] (From Jo HS, et al. J Korean Med Sci 2015;30 Suppl 1:S81-S87, according to the Creative Commons license) [19]. |
 | Figure 5Incidence of intraventricular hemorrhage (IVH) according to gestational age (GA) (A) and birth weight (BW) (B). The proportions of infants with grades 1, 2, 3, and 4 IVH and without IVH are presented according to GA and BW (From Ahn SY, et al. J Korean Med Sci 2015;30 Suppl 1:S52-S58, according to the Creative Commons license) [20]. |
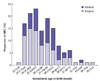 | Figure 6Ecrotizing enterocolitis (NEC) incidence according to gestational age (week) (From Youn YA, et al. J Korean Med Sci 2015;30 Suppl 1:S75-S80, according to the Creative Commons license) [23]. |
 | Figure 7The incidences of severity of retinopathy of prematurity (ROP) and treatment according to the gestational age and birth weight in very low birth weight infants. (A) The incidences of severity of ROP and treatment according to gestational age. (B) The incidences of severity of ROP and treatment according to birth weight (From Hwang JH, et al. J Korean Med Sci 2015;30 Suppl 1:S88-S94, according to the Creative Commons license) [24]. |
Table 1
Neonatal survival rates of VLBWIs and ELBWI in the Korea by the Korean Neonatal Network (2013-2014. June)
From Shim JW, et al. J Korean Med Sci 2015;30 Suppl 1:S25-S34, according to the Creative Commons license [3]. VLBWI, very low birth weight infant; ELBWI, extremely low birth weight infants.
*Total number of admission in neonatal intensive care units: 2,386 data-locked cases; †Number of survived infants at time of discharge from neonatal intensive care unit.
Table 2
Patient characteristics according to the PDA treatment strategies in very low birth weight infants in Korea

From Lee JA, et al. J Korean Med Sci 2015;30 Suppl 1:S59-S66, according to the Creative Commons license [21].
PDA, patent ductus arteriosus; PT, prophylactic treatment; PST, pre-symptomatic treatment; ST, symptomatic treatment; CT, conservative treatment without any intervention; NA, not appropriate; GA, gestational age at birth; HCA, histologic chorioamnionitis; PIH, pregnancy induced hypertension; SGA, small for gestational age; DR, delivery room; AS, apgar score.
*P<0.05 in one-way ANOVA with Tukey or chi-square test with Bonferroni correction between no PDA, PT, PST, ST, and CT groups; †P<0.05 when compared with no PDA group;
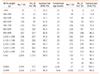
Table 3
Rates of sepsis/1,000 hospital days and incidence of sepsis versus birth weight and GA

From Lee SM, et al. J Korean Med Sci 2015;30 Suppl 1:S67-S74, according to the Creative Commons license [22].
GA, gestational age.
*Same in the birth weight group.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download