Abstract
Evaluation systems can produce curricular change. Korean medical schools face a new responsibility to prepare students for the Korean Medical Licensing Examination (KMLE) clinical skills test (CST) that had been administered since 2009. Several innovations in medical education have resulted, including augmentation of hand-on skills training and a standardized patient program during clerkships. This review explored the results of a survey of 41 medical schools on the impact of the CST on medical education in Korea as of 2011. The majority of respondents reported having an independent skills training laboratory and conducting a clinical skills assessment during the third or fourth year of medical school. The preparatory undergraduate courses were perceived as helpful for self-confidence, communication with real patients, basic clinical skills for work, information sharing with patients, and getting the confidence of patients during internship and residency. However, an extreme policy emphasizing maintenance of a high pass rate has warped the curriculum with simple preparatory courses for the CST. The long-term educational outcomes of the CST of the KMLE must be evaluated again a few years later focused on searching for any relationship with a reduction in medical errors or increase in patient satisfaction in real practice.
Figures and Tables
Table 1
The change of educational facilities and curricular contents of medical schools after the introduction of clinical skills test in 2009 at KMLE
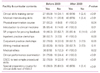
Table 2
The change of opportunity for medical students to practice during clerkship rotations after the introduction of CSA in KMLE

Table 3
The behavioral change of interns or the first year residents at university hospital rated by professors, nurses, and patients after the introduction of clinical skills assessment of KMLE in 2009
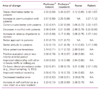
Rating was done on the 5-point Likert scale (strong agree, 5; agree, 4; neutral, 3; disagree, 2; strongly disagree, 1).
The numbers in parentheses are standard deviation.
KMLE, Korean Medical Licensing Examination; NA, not applicable; IV, intravenous catheterization; EKG, electrocardiogam.
a)Professors' opinion about interns' ability.
b)Professors' opinion about residents' ability.
Acknowledgement
This study was supported by funding from the Research Institute for Healthcare Policy of the Korean Medical Association in 2011.
References
1. Guskey TR. How classroom assessments improve learning. Educ Leadersh. 2003. 60:6–11.
2. Carraccio C, Wolfsthal SD, Englander R, Ferentz K, Martin C. Shifting paradigms: from Flexner to competencies. Acad Med. 2002. 77:361–367.
3. Park JH, Kim UM, Lee WC, Lee YS. A study on the satisfaction of medical licensing examination and the present condition of skill test in medical schools. J Educ Eval Health Prof. 2004. 1:77–86.

4. Park H. Clinical skills assessment in Korean Medical Licensing Examination. Korean J Med Educ. 2008. 20:309–312.

6. Kim KS. Introduction and administration of the clinical skill test of the Medical Licensing Examination, Republic of Korea (2009). J Educ Eval Health Prof. 2010. 7:4.

7. Hauer KE, Teherani A, Kerr KM, O'sullivan PS, Irby DM. Impact of the United States Medical Licensing Examination Step 2 Clinical Skills exam on medical school clinical skills assessment. Acad Med. 2006. 81:10 Suppl. S13–S16.

8. Wartman SA, Littlefield JH. Changes in the US Medical Licensure Examination and impact on US medical schools. JAMA. 2005. 293:424–425.

9. Pfeiffer CA, Ardolino AJ, Madray H. The impact of a curriculum renewal project on students' performances on a fourth-year clinical skills assessment. Acad Med. 2001. 76:173–175.

10. Mehta NP, Kramer DB. A Critique of the USMLE clinical skills examination. MedGenMed. 2005. 7:76.
11. Petrusa ER. Taking standardized patient-based examinations to the next level. Teach Learn Med. 2004. 16:98–110.
12. McGaghie WC, Issenberg SB, Petrusa ER. Simulation-Savior or Satan? A rebuttal. Adv Health Sci Educ Theory Pract. 2003. 8:97–103.
13. Rickles NM, Tieu P, Myers L, Galal S, Chung V. The impact of a standardized patient program on student learning of communication skills. Am J Pharm Educ. 2009. 73:4.

14. Hauer KE, Hodgson CS, Kerr KM, Teherani A, Irby DM. A national study of medical student clinical skills assessment. Acad Med. 2005. 80:10 Suppl. S25–S29.

15. Davis MH, Harden RM. Planning and implementing an undergraduate medical curriculum: the lessons learned. Med Teach. 2003. 25:596–608.

16. Turner JL, Dankoski ME. Objective structured clinical exams: a critical review. Fam Med. 2008. 40:574–578.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download