Abstract
The myeloproliferative neoplasm (MPN), polycythemia vera (PV), essential thrombocytosis (ET), and primary myelofibrosis (PMF) are clonal hematopoietic stem cell diseases that share in common overproduction of one or more of the formed elements of the blood with overlapping clinical features but exhibit different natural histories and different therapeutic requirements. Therefore, accuracy of diagnosis is the cornerstone of therapy. The World Health Organization diagnostic criteria for both the classic BCR-ABL-negative MPNs (that is PV, ET, and PMF) and chronic eosinophilic leukemia/hypereosinophilic syndrome have been revised in the 2008 edition, by incorporating new information on their V617F mutation in the Janus kinase 2 (JAK2) tyrosine kinase. The JAK2 V617F point mutation makes the normal hematopoietic progenitor cells hypersensitive to thrombopoietin, erythropoietin, and myeloid progenitor cells, leading to trilinear hematopoietic myeloproliferation. JAK2 V617F is found in most patients with PV, ET, or PMF and is, therefore, useful as a clonal marker when present. However their absence does not exclude the diagnosis of an MPN. The major complications of the MPN are thrombosis, hemorrhage and extramedullary hematopoiesis with massive splenomegaly and bone marrow failure. Myelofibrosis is classically listed as a complication of the MPN. Current treatment options are low dose aspirin, phlebotomy and cytoreductive therapy with hydroxyurea, anagrelide, and interferon for PV and ET but the most effective therapy is still bone marrow transplantation for PMF for the relief of symptoms and the prevention of complications. Drugs targeting JAK2 V617F are promising. This article reviews the changes in diagnostic criteria and algorithms, and also provides treatment guidelines that are tailored to routine clinical practice.
Figures and Tables
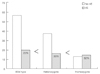
 | Figure 1(A) Annual registered number of patients with polycythemia vera (PV), essential thrombocythemia (ET) and primary myelofibrosis (PMF). (B) Assumptive prevalence rate of PV, ET, and PMF per 100,000 persons per one year (from the databases of Korean Health Insurance Review and Assessment Service). |
Table 1
The 2008 World Health Organization (WHO) diagnostic criteria for polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF) [9]

Hgb, hemoglobin; Hct, hematocrit; CML, chronic myelogenous leukemia; MDS, myelodysplastic syndrome; BM, bone marrow; Epo, erythropoietin; EEC, endogenous erythroid colony; LDH, lactate dehydrogenase.
a)Diagnosis of polycythemia vera (PV) requires meeting either both major criteria and one minor criterion or the first major criterion and 2 minor criteria. Diagnosis of ET requires meeting all four major criteria.
b)Small to large megakaryocytes with an aberrant nuclear/cytoplasmic ratio and hyperchromatic and irregularly folded nuclei and dense clustering.
References
1. Tefferi A, Thiele J, Orazi A, Kvasnicka HM, Barbui T, Hanson CA, Barosi G, Verstovsek S, Birgegard G, Mesa R, Reilly JT, Gisslinger H, Vannucchi AM, Cervantes F, Finazzi G, Hoffman R, Gilliland DG, Bloomfield CD, Vardiman JW. Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood. 2007. 110:1092–1097.

2. Ania BJ, Suman VJ, Sobell JL, Codd MB, Silverstein MN, Melton LJ 3rd. Trends in the incidence of polycythemia vera among Olmsted County, Minnesota residents, 1935-1989. Am J Hematol. 1994. 47:89–93.

3. Mesa RA, Silverstein MN, Jacobsen SJ, Wollan PC, Tefferi A. Population-based incidence and survival figures in essential thrombocythemia and agnogenic myeloid metaplasia: an Olmsted County Study, 1976-1995. Am J Hematol. 1999. 61:10–15.

4. Baxter EJ, Scott LM, Campbell PJ, East C, Fourouclas N, Swanton S, Vassiliou GS, Bench AJ, Boyd EM, Curtin N, Scott MA, Erber WN, Green AR. The Cancer Genome Project. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005. 365:1054–1061.

5. Kralovics R, Passamonti F, Buser AS, Teo SS, Tiedt R, Passweg JR, Tichelli A, Cazzola M, Skoda RC. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med. 2005. 352:1779–1790.

6. Percy MJ, Scott LM, Erber WN, Harrison CN, Reilly JT, Jones FG, Green AR, McMullin MF. The frequency of JAK2 exon 12 mutations in idiopathic erythrocytosis patients with low serum erythropoietin levels. Haematologica. 2007. 92:1607–1614.

7. Scott LM, Tong W, Levine RL, Scott MA, Beer PA, Stratton MR, Futreal PA, Erber WN, McMullin MF, Harrison CN, Warren AJ, Gilliland DG, Lodish HF, Green AR. JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N Engl J Med. 2007. 356:459–468.

8. Martinez-Aviles L, Besses C, Alvarez-Larran A, Cervantes F, Hernandez-Boluda JC, Bellosillo B. JAK2 exon 12 mutations in polycythemia vera or idiopathic erythrocytosis. Haematologica. 2007. 92:1717–1718.

9. Tefferi A, Vardiman JW. Classification and diagnosis of myeloproliferative neoplasms: the 2008 World Health Organization criteria and point-of-care diagnostic algorithms. Leukemia. 2008. 22:14–22.

10. Tefferi A, Thiele J, Vardiman JW. The 2008 World Health Organization classification system for myeloproliferative neoplasms: order out of chaos. Cancer. 2009. 115:3842–3847.

11. Chen Q, Lu P, Jones AV, Cross NC, Silver RT, Wang YL. Amplification refractory mutation system, a highly sensitive and simple polymerase chain reaction assay, for the detection of JAK2 V617F mutation in chronic myeloproliferative disorders. J Mol Diagn. 2007. 9:272–276.

12. Olsen RJ, Tang Z, Farkas DH, Bernard DW, Zu Y, Chang CC. Detection of the JAK2(V617F) mutation in myeloproliferative disorders by melting curve analysis using the LightCycler system. Arch Pathol Lab Med. 2006. 130:997–1003.

13. Murugesan G, Aboudola S, Szpurka H, Verbic MA, Maciejewski JP, Tubbs RR, Hsi ED. Identification of the JAK2 V617F mutation in chronic myeloproliferative disorders using FRET probes and melting curve analysis. Am J Clin Pathol. 2006. 125:625–633.

14. Cankovic M, Whiteley L, Hawley RC, Zarbo RJ, Chitale D. Clinical performance of JAK2 V617F mutation detection assays in a molecular diagnostics laboratory: evaluation of screening and quantitation methods. Am J Clin Pathol. 2009. 132:713–721.

15. Chusid MJ, Dale DC, West BC, Wolff SM. The hypereosinophilic syndrome: analysis of fourteen cases with review of the literature. Medicine (Baltimore). 1975. 54:1–27.
17. Fauci AS, Harley JB, Roberts WC, Ferrans VJ, Gralnick HR, Bjornson BH. NIH conference. The idiopathic hypereosinophilic syndrome. Clinical, pathophysiologic, and therapeutic considerations. Ann Intern Med. 1982. 97:78–92.
18. Golub TR, Barker GF, Lovett M, Gilliland DG. Fusion of PDGF receptor beta to a novel ets-like gene, tel, in chronic myelomonocytic leukemia with t(5;12) chromosomal translocation. Cell. 1994. 77:307–316.

19. Cogan E, Schandené L, Crusiaux A, Cochaux P, Velu T, Goldman M. Brief report: clonal proliferation of type 2 helper T cells in a man with the hypereosinophilic syndrome. N Engl J Med. 1994. 330:535–538.

20. Vardiman JW, Brunning RD, Harris NL. Jaffe ES, Harris NL, Stein H, Vardiman JW, editors. WHO histological classification of chronic myeloproliferative diseases. World Health Organization classification of tumours of haematopoietic and lymphoid tissues. 2001. Lyon: IARC Press;17–44.
21. Trempat P, Villalva C, Laurent G, Armstrong F, Delsol G, Dastugue N, Brousset P. Chronic myeloproliferative disorders with rearrangement of the platelet-derived growth factor alpha receptor: a new clinical target for STI571/Glivec. Oncogene. 2003. 22:5702–5706.

22. Cools J, DeAngelo DJ, Gotlib J, Stover EH, Legare RD, Cortes J, Kutok J, Clark J, Galinsky I, Griffin JD, Cross NC, Tefferi A, Malone J, Alam R, Schrier SL, Schmid J, Rose M, Vandenberghe P, Verhoef G, Boogaerts M, Wlodarska I, Kantarjian H, Marynen P, Coutre SE, Stone R, Gilliland DG. A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosino-philic syndrome. N Engl J Med. 2003. 348:1201–1214.

23. Klion AD, Bochner BS, Gleich GJ, Nutman TB, Rothenberg ME, Simon HU, Wechsler ME, Weller PF. The Hypereosinophilic Syndromes Working Group. Approaches to the treatment of hypereosinophilic syndromes: a workshop summary report. J Allergy Clin Immunol. 2006. 117:1292–1302.

24. Roche-Lestienne C, Lepers S, Soenen-Cornu V, Kahn JE, Laï JL, Hachulla E, Drupt F, Demarty AL, Roumier AS, Gardembas M, Dib M, Philippe N, Cambier N, Barete S, Libersa C, Bletry O, Hatron PY, Quesnel B, Rose C, Maloum K, Blanchet O, Fenaux P, Prin L, Preudhomme C. Molecular characterization of the idiopathic hypereosinophilic syndrome (HES) in 35 French patients with normal conventional cytogenetics. Leukemia. 2005. 19:792–798.

25. Klion AD, Noel P, Akin C, Law MA, Gilliland DG, Cools J, Metcalfe DD, Nutman TB. Elevated serum tryptase levels identify a subset of patients with a myeloproliferative variant of idiopathic hypereosinophilic syndrome associated with tissue fibrosis, poor prognosis, and imatinib responsiveness. Blood. 2003. 101:4660–4666.

26. Xiao S, Nalabolu SR, Aster JC, Ma J, Abruzzo L, Jaffe ES, Stone R, Weissman SM, Hudson TJ, Fletcher JA. FGFR1 is fused with a novel zinc-finger gene, ZNF198, in the t(8;13) leukaemia/lymphoma syndrome. Nat Genet. 1998. 18:84–87.

27. Finazzi G, Barbui T. Risk-adapted therapy in essential thrombocythemia and polycythemia vera. Blood Rev. 2005. 19:243.

28. Marchioli R, Finazzi G, Landolfi R, Kutti J, Gisslinger H, Patrono C, Marilus R, Villegas A, Tognoni G, Barbui T. Vascular and neoplastic risk in a large cohort of patients with polycythemia vera. J Clin Oncol. 2005. 23:2224–2232.

30. Berk PD, Goldberg JD, Donovan PB, Fruchtman SM, Berlin NI, Wasserman LR. Therapeutic recommendations in polycythemia vera based on Polycythemia Vera Study Group protocols. Semin Hematol. 1986. 23:132–143.
31. Di Nisio M, Barbui T, Di Gennaro L, Borrelli G, Finazzi G, Landolfi R, Leone G, Marfisi R, Porreca E, Ruggeri M, Rutjes AW, Tognoni G, Vannucchi AM, Marchioli R. The haematocrit and platelet target in polycythemia vera. Br J Haematol. 2007. 136:249–259.

32. Landolfi R, Marchioli R, Kutti J, Gisslinger H, Tognoni G, Patrono C, Barbui T. Efficacy and safety of low-dose aspirin in polycythemia vera. N Engl J Med. 2004. 350:114–124.

33. Fruchtman SM, Mack K, Kaplan ME, Peterson P, Berk PD, Wasserman LR. From efficacy to safety: a Polycythemia Vera Study Group report on hydroxyurea in patients with polycythemia vera. Semin Hematol. 1997. 34:17–23.
34. Najean Y, Rain JD. Treatment of polycythemia vera: the use of hydroxyurea and pipobroman in 292 patients under the age of 65 years. Blood. 1997. 90:3370–3377.

35. Sterkers Y, Preudhomme C, Lai JL, Demory JL, Caulier MT, Wattel E, Bordessoule D, Bauters F, Fenaux P. Acute myeloid leukemia and myelodysplastic syndromes following essential thrombocythemia treated with hydroxyurea: high proportion of cases with 17p deletion. Blood. 1998. 91:616–622.

36. Murphy S, Peterson P, Iland H, Laszlo J. Experience of the Polycythemia Vera Study Group with essential thrombocythemia: a final report on diagnostic criteria, survival, and leukemic transition by treatment. Semin Hematol. 1997. 34:29–39.
37. Finazzi G, Caruso V, Marchioli R, Capnist G, Chisesi T, Finelli C, Gugliotta L, Landolfi R, Kutti J, Gisslinger H, Marilus R, Patrono C, Pogliani EM, Randi ML, Villegas A, Tognoni G, Barbui T. Acute leukemia in polycythemia vera: an analysis of 1638 patients enrolled in a prospective observational study. Blood. 2005. 105:2664–2670.

38. Lengfelder E, Berger U, Hehlmann R. Interferon alpha in the treatment of polycythemia vera. Ann Hematol. 2000. 79:103–109.
39. Harrison CN, Green AR. Essential thrombocythemia. Hematol Oncol Clin North Am. 2003. 17:1175–1190.

40. Finazzi G, Rambaldi A, Guerini V, Carobbo A, Barbui T. Risk of thrombosis in patients with essential thrombocythemia and polycythemia vera according to JAK2 V617F mutation status. Haematologica. 2007. 92:135–136.

41. Hsiao HH, Yang MY, Liu YC, Lee CP, Yang WC, Liu TC, Chang CS, Lin SF. The association of JAK2V617F mutation and leukocytosis with thrombotic events in essential thrombocythemia. Exp Hematol. 2007. 35:1704–1707.

42. Hexner EO. JAK2 V617F: implications for thrombosis in myeloproliferative diseases. Curr Opin Hematol. 2007. 14:450–454.

43. Ruggeri M, Finazzi G, Tosetto A, Riva S, Rodeghiero F, Barbui T. No treatment for low-risk thrombocythaemia: results from a prospective study. Br J Haematol. 1998. 103:772–777.

44. Cortelazzo S, Viero P, Finazzi G, D'Emilio A, Rodeghiero F, Barbui T. Incidence and risk factors for thrombotic complications in a historical cohort of 100 patients with essential thrombocythemia. J Clin Oncol. 1990. 8:556–562.

45. Cortelazzo S, Finazzi G, Ruggeri M, Vestri O, Galli M, Rodeghiero F, Barbui T. Hydroxyurea for patients with essential thrombocythemia and a high risk of thrombosis. N Engl J Med. 1995. 332:1132–1136.

46. Alvarez-Larran A, Cervantes F, Bellosillo B, Giralt M, Julia A, Hernandez-Boluda JC, Bosch A, Hernandez-Nieto L, Clapes V, Burgaleta C, Salvador C, Arellano-Rodrigo E, Colomer D, Besses C. Essential thrombocythemia in young individuals: frequency and risk factors for vascular events and evolution to myelofibrosis in 126 patients. Leukemia. 2007. 21:1218–1223.

47. Griesshammer M. Options in the management of essential thrombocythaemia. Eur J Haematol Suppl. 2007. (68):35–39.

48. Birgegard G. Essential thrombocythaemia treatment options: addressing patient-specific needs. Eur J Haematol Suppl. 2007. (68):27–31.
49. Harrison CN, Campbell PJ, Buck G, Wheatley K, East CL, Bareford D, Wilkins BS, van der Walt JD, Reilly JT, Grigg AP, Revell P, Woodcock BE, Green AR. United Kingdom Medical Research Council Primary Thrombocythemia 1 Study. Hydroxyurea compared with anagrelide in high-risk essential thrombocythemia. N Engl J Med. 2005. 353:33–45.

50. Steurer M, Gastl G, Jedrzejczak WW, Pytlik R, Lin W, Schlögl E, Gisslinger H. Anagrelide for thrombocytosis in myeloproliferative disorders: a prospective study to assess efficacy and adverse event profile. Cancer. 2004. 101:2239–2246.

51. Shvidel L, Sigler E, Haran M, Klepfish A, Duek A, Berrebi A, Shtalrid M. Busulphan is safe and efficient treatment in elderly patients with essential thrombocythemia. Leukemia. 2007. 21:2071–2072.

52. Pagliaro P, Arrigoni L, Muggiasca ML, Poggio M, Russo U, Rossi E. Primary thrombocythemia and pregnancy: treatment and outcome in fifteen cases. Am J Hematol. 1996. 53:6–10.

53. Schmidt HH, Neumeister P, Kainer F, Karpf EF, Linkesch W, Sill H. Treatment of essential thrombocythemia during pregnancy: antiabortive effect of interferon-alpha? Ann Hematol. 1998. 77:291–292.

54. Elliott MA, Tefferi A. Interferon-alpha therapy in polycythemia vera and essential thrombocythemia. Semin Thromb Hemost. 1997. 23:463–472.

55. Cervantes F, Dupriez B, Pereira A, Passamonti F, Reilly JT, Morra E, Vannucchi AM, Mesa RA, Demory JL, Barosi G, Rumi E, Tefferi A. New prognostic scoring system for primary myelofibrosis based on a study of the International Working Group for Myelofibrosis Research and Treatment. Blood. 2009. 113:2895–2901.

56. Hoffman R, Rondelli D. Biology and treatment of primary myelofibrosis. Hematology Am Soc Hematol Educ Program. 2007. 346–354.

57. Verstovsek S. Therapeutic potential of JAK2 inhibitors. Hematology Am Soc Hematol Educ Program. 2009. 636–642.

58. Parrillo JE, Fauci AS, Wolff SM. Therapy of the hypereosinophilic syndrome. Ann Intern Med. 1978. 89:167–172.

59. Klion AD, Law MA, Noel P, Kim YJ, Haverty TP, Nutman TB. Safety and efficacy of the monoclonal anti-interleukin-5 antibody SCH55700 in the treatment of patients with hypereosinophilic syndrome. Blood. 2004. 103:2939–2941.

60. Garrett JK, Jameson SC, Thomson B, Collins MH, Wagoner LE, Freese DK, Beck LA, Boyce JA, Filipovich AH, Villanueva JM, Sutton SA, Assa'ad AH, Rothenberg ME. Anti-interleukin-5 (mepolizumab) therapy for hypereosinophilic syndromes. J Allergy Clin Immunol. 2004. 113:115–119.

61. Klion AD, Robyn J, Akin C, Noel P, Brown M, Law M, Metcalfe DD, Dunbar C, Nutman TB. Molecular remission and reversal of myelofibrosis in response to imatinib mesylate treatment in patients with the myeloproliferative variant of hypereosinophilic syndrome. Blood. 2004. 103:473–478.

62. von Bubnoff N, Sandherr M, Schlimok G, Andreesen R, Peschel C, Duyster J. Myeloid blast crisis evolving during imatinib treatment of an FIP1L1-PDGFR alpha-positive chronic myeloproliferative disease with prominent eosinophilia. Leukemia. 2005. 19:286–287.

63. Pitini V, Arrigo C, Azzarello D, La Gattuta G, Amata C, Righi M, Coglitore S. Serum concentration of cardiac Troponin T in patients with hypereosinophilic syndrome treated with imatinib is predictive of adverse outcomes. Blood. 2003. 102:3456–3457.

64. Ueno NT, Anagnostopoulos A, Rondón G, Champlin RE, Mikhailova N, Pankratova OS, Zoubarovskaya LS, Semenova EV, Afanasyev BV, O'Brien S, Andreeff M, Zaritskey AY. Successful non-myeloablative allogeneic transplantation for treatment of idiopathic hypereosinophilic syndrome. Br J Haematol. 2002. 119:131–134.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download