Abstract
Daylight Saving Time (DST) is used worldwide and affects millions of people annually. In the most countries, DST begins turning clocks forward by an hour in the spring and backward by an hour in the fall. transition out of DST in the fall increases the available daylight in the morning by one hour. Springtime transition into DST leads to an increase of the available daylight in the evening. During World War I, in an effort to reduce fuel consumption, Germany and England began to practice DST in 1916. Currently, 77 countries and most of OECD adopted DST except Korea, Japan, Iceland. The rationale for Daylight Saving Time (DST) is bolstered by the fact that it increases daylight hours within which the activity a population reaches its peak. Therefore, the effects of transitions into DST to the public health should be further explored, as DST affects millions of people annually and its impacts are still largely unknown. A general perception is that Turning clock forwards (on spring) or backwards (on fall) by one hour would affect our health. In This study, the association between Daylight Saving Time (DST) and health in population was investigated through theoretical and systemic review studies. Since the study was conducted solely on theoretical grounds, further research is needed to assess additional health-related impacts of Daylight Saving Time (DST) and to carry out more specific analysis on population health in Korea. In conclusion, population health is more strongly affected during spring transition into DST than during fall transition out of DST.
Figures and Tables
Figure 1
Relationship between natural and behavioral light-dark cycles with and without DST; adopted from kantermann, et al.(9)

Table 1
Measures of the rest-activity cycle at baseline and after transition into DST
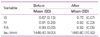
*Abbreviations: SD=standard deviation, IS=intra-daily stability, IV=intra-daily variability, RA=relative amplitude, tau=circadian period.
†Adopted from Lahti, et al.(8)
Table 2
Changes due to transition into DST among short -and long-sleepers
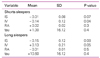
*Abbreviations: SD=standard deviation, IS=intra- daily stability, IV=intra-daily variability, RA= relative amplitude, tau=circadian period.
†Adopted from Lahti, et al.(8)
References
1. Lee SG. The brief history of Daylight Saving Time in other countries and energy saving effect. 2006. Republic of Korea: Korea Energy Economics Institute;5–42.
2. Mistlberger RE, Rusak B. Kryger MH, Roth T, Dement WC, editors. Circadian rhythms in mammals. Formal properties and envind practice of sleep medicine. 2005. 4thed. Philadelphia: Elsevier Sauronmental influences;321–334. Principles anders.

3. Turek FW, Dugovic C, Zee PC. Current understanding of the circadian clock and the clinical implications for neurological disorders. Arch Neurol. 2001. 58:1781–1787.

4. Monk TH, Folkard S. Adjusting to the changes to and from Daylight Saving Time. Nature. 1976. 261:688–689.

5. Monk TH, Aplin LC. Spring and autumn daylight saving time changes: studies of adjustment in sleep timings, mood, and efficiency. Ergonomics. 1980. 23:167–178.

6. Lahti TA, Leppämäki S, Lönnqvist J, Partonen T. Transition to daylight saving time reduces sleep duration plus sleep efficiency of the deprived sleep. Neuroscience Letters. 2006. 406:174–177.

7. Lahti TA, Leppämäki S, Ojanen SM, Haukka J, Tuulio-Henriksson A, Lönnqvist J, Partonen T. Transition into daylight saving time influences the fragmentation of the rest-activity cycle. J Circadian Rhythms. 2006. 19:1.

8. Lahti TA, Leppämäki S, Lönnqvist J, Partonen T. Transitions into and out of daylight saving time compromise sleep and the rest-activity cycles. BMC Physiol. 2008. 12:3.

9. Kantermann T, Juda M, Merrow M, Roenneberg T. The human circadian clock's seasonal adjustment is disrupted by daylight saving time. Curr Biol. 2007. 17:1996–2000.

10. Schneider AM, Randler C. Daytime sleepiness during transition into daylight saving time in adolescents: Are owls higher at risk? Sleep Med. 2009. 10:1047–1050.

11. Lahti TA, Haukka J, Lönnqvist J, Partonen T. Daylight saving time transitions and hospital treatments due to accidents or manic episodes. BMC Public Health. 2008. 8:74.

12. Bick PA, Hannah AL. The effect of daylight saving time on the incidence of psychiatric presentations. 1986. In : Royal College of Psychiatrists Annual Meeting; University of Southampton;–5.
13. Shapiro CM, Blake F, Fossey E, Adams B. Daylight saving time in psychiatric illness. J Affect Disord. 1990. 19:177–181.

14. Foerch C, Korf HW, Steinmetz H, Sitzer M. Abrupt shift of the pattern of diurnal variation in stroke onset with daylight saving time transitions. Circulation. 2008. 118:284–290.

15. Mistlberger RE, Skene DJ. Social influences on mammalian circadian rhythms. Biol Rev Camb Philos Soc. 2004. 79:533–556.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download