Abstract
Mucositis is the one of the most common complications during chemotherapy or radiotherapy. Once developed, mucositis influences the treatment outcome by severe pain, malnutrition, risk of infection, and prolonged hospitalization. Mucositis is usually developed in oral cavity and gastrointestinal tract. It is developed by the complex pathway, which is composed of initiation by reactive oxygen species, upregulation of various cytokine (e.g. TNF-α, IL-1β, IL- 6), and amplification of tissue injury, ulceration, and healing. Risk factors of mucositis include specific kinds of chemotherapy drug, hematopoietic stem cell transplantation, the site and dose of radiation, concurrent chemoradiation, malnutrition, salivary grand dysfunction, and poor oral hygiene. Routine oral care is very important for the prevention and treatment of oral mucositis and its administration should be included in patient education. Local anesthetics and systemic opioid can be used for severe pain of oral mucositis. Cryotherapy and low-level laser treatment is also useful for prevention of oral mucositis. Diarrhea, which is the most common symptom of gastrointestinal mucositis, can be controlled by loperamide or octreotide. More effective agents or procedures are needed for the prevention and treatment of chemotherapy related oral and gastrointestinal mucositis. The prevention is the most important approach in mucositis care and therefore multidisciplinary team approach including oncologists, dentists, nurses, and nutritionists is essential.
Figures and Tables
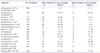
Table 1
Comparison of toxicity grading of oral mucositis according to World Health Organization Criteria, National Cancer Institute-Common Toxicity Criteria

Table 2
Toxicity grading of gastrointestinal mucositis according to National Cancer Institute-Common Toxicity Criteria

Table 3
Relation between antineoplastic therapy and risk of grade 3~4 oral and gastrointestinal mucositis
GI: gastrointestinal, 95% CI: 95% confidence interval, 5-FU: 5-fluorouracil, XRT: radiotherapy, BMT: bone marrow transplantation, TBI: total body irradiation.
Adapted from reference (1).
Table 4
Relation between cancer diagnosis and risk of grade 3-4 oral and gastrointestinal mucositis
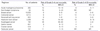
GI: gastrointestinal, 95% CI: 95% confidence interval, NR: not reported.
Adapted from reference (1).
References
1. Sonis ST, Elting LS, Keefe D, Peterson DE, Schubert M, Hauer-Jensen M, Bekele BN, Raber-Durlacher J, Donnelly JP, Rubenstein EB. Perspectives on cancer therapy-induced mucosal injury: pathogenesis, measurement, epi-demiology, and consequences for patients. Cancer. 2004. 100:1995–2025.

2. Bowen JM, Gibson RJ, Cummins AG, Keefe DM. Intestinal mucositis: the role of the Bcl-2 family, p53 and caspases in chemotherapy-induced damage. Support Care Cancer. 2006. 14:713–731.

3. Keefe DM, Cummins AG, Dale BM, Kotasek D, Robb TA, Sage RE. Effect of high-dose chemotherapy on intestinal permeability in humans. Clin Sci (Lond). 1997. 92:385–389.

4. Pico JL, Avila-Garavito A, Naccache P. Mucositis: Its Occurrence, Consequences, and Treatment in the Oncology Setting. Oncologist. 1998. 3:446–451.

5. Elting LS, Cooksley C, Chambers M, Cantor SB, Manzullo E, Rubenstein EB. The burdens of cancer therapy. Clinical and economic outcomes of chemotherapy-induced mucositis. Cancer. 2003. 98:1531–1539.
6. Goldberg SL, Chiang L, Selina N, Hamarman S. Patient perceptions about chemotherapy-induced oral mucositis: implications for primary/secondary prophylaxis strategies. Support Care Cancer. 2004. 12:526–530.

7. Potten CS. A comprehensive study of the radiobiological response of the murine (BDF1) small intestine. Int J Radiat Biol. 1990. 58:925–973.

8. World Health Organization. WHO handbook for reporting results of cancer treatment. 1979. Geneva: World Health Organization.
9. Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, Langer C, Murphy B, Cumberlin R, Coleman CN, Rubin P. CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol. 2003. 13:176–181.

11. Sonis ST, Oster G, Fuchs H, Bellm L, Bradford WZ, Edelsberg J, Hayden V, Eilers J, Epstein JB, LeVeque FG, Miller C, Peterson DE, Schubert MM, Spijkervet FK, Horowitz M. Oral mucositis and the clinical and economic outcomes of hematopoietic stem-cell transplantation. J Clin Oncol. 2001. 19:2201–2205.

12. Lockhart PB, Sonis ST. Alterations in the oral mucosa caused by chemotherapeutic agents. A histologic study. J Dermatol Surg Oncol. 1981. 7:1019–1025.
13. Paris F, Fuks Z, Kang A, Capodieci P, Juan G, Ehleiter D, Haimovitz-Friedman A, Cordon-Cardo C, Kolesnick R. Endothelial apoptosis as the primary lesion initiating intestinal radiation damage in mice. Science. 2001. 293:293–297.

14. Sonis ST, Peterson RL, Edwards LJ, Lucey CA, Wang L, Mason L, Login G, Ymamkawa M, Moses G, Bouchard P, Hayes LL, Bedrosian C, Dorner AJ. Defining mechanisms of action of interleukin-11 on the progression of radiation-induced oral mucositis in hamsters. Oral Oncol. 2000. 36:373–381.

15. Wang J, Albertson CM, Zheng H, Fink LM, Herbert JM, Hauer-Jensen M. Short-term inhibition of ADP-induced platelet aggregation by clopidogrel ameliorates radiation-induced toxicity in rat small intestine. Thromb Haemost. 2002. 87:122–128.

16. Hall PD, Benko H, Hogan KR, Stuart RK. The influence of serum tumor necrosis factor-alpha and interleukin-6 concentrations on nonhematologic toxicity and hematologic recovery in patients with acute myelogenous leukemia. Exp Hematol. 1995. 23:1256–1260.
17. Epstein JB, Silverman S Jr, Paggiarino DA, Crockett S, Schubert MM, Senzer NN, Lockhart PB, Gallagher MJ, Peterson DE, Leveque FG. results from a multicenter, randomized, double-blind, placebo-controlled clinical trial. Cancer. 2001. 92:875–885.
18. Culy CR. Spencer CM Amifostine: an update on its clinical status as a cytoprotectant in patients with cancer receiving chemotherapy or radiotherapy and its potential therapeutic application in myelodysplastic syndrome. Drugs. 2001. 61:641–684.
19. van den Broek GB, Balm AJ, van den Brekel MW, Hauptmann M, Schornagel JH, Rasch CR. Relationship between clinical factors and the incidence of toxicity after intra-arterial chemoradiation for head and neck cancer. Radiother Oncol. 2006. 81:143–150.

20. Bensinger W, Schubert M, Ang KK, Brizel D, Brown E, Eilers JG, Elting L, Mittal BB, Schattner MA, Spielberger R, Treister NS, Trotti AM 3rd. NCCN Task Force Report. prevention and management of mucositis in cancer care. J Natl Compr Canc Netw. 2008. 6:Suppl 1. S1–S21. quiz S22-24.

21. Chansky K, Benedetti J, Macdonald JS. Differences in toxicity between men and women treated with 5-fluorouracil therapy for colorectal carcinoma. Cancer. 2005. 103:1165–1171.

22. Robien K, Schubert MM, Bruemmer B, Lloid ME, Potter JD, Ulrich CM. Predictors of oral mucositis in patients receiving hematopoietic cell transplants for chronic myelogenous leukemia. J Clin Oncol. 2004. 22:1268–1275.

23. Vera-Llonch M, Oster G, Hagiwara M, Sonis S. Oral mucositis in patients undergoing radiation treatment for head and neck carcinoma. Cancer. 2006. 106:329–336.

24. McCollum AD, Catalano PJ, Haller DG, Mayer RJ, Macdonald JS, Benson AB 3rd, Fuchs CS. Outcomes and toxicity in african-american and caucasian patients in a randomized adjuvant chemotherapy trial for colon cancer. J Natl Cancer Inst. 2002. 94:1160–1167.

25. Iyer L, King CD, Whitington PF, Green MD, Roy SK, Tephly TR, Coffman BL, Ratain MJ. Genetic predisposition to the metabolism of irinotecan (CPT-11). Role of uridine diphosphate glucuronosyltransferase isoform 1A1 in the glucuronidation of its active metabolite (SN-38) in human liver microsomes. J Clin Invest. 1998. 101:847–854.

26. McCarthy GM, Awde JD, Ghandi H, Vincent M, Kocha WI. Risk factors associated with mucositis in cancer patients receiving 5-fluorouracil. Oral Oncol. 1998. 34:484–490.

27. Keefe DM, Schubert MM, Elting LS, Sonis ST, Epstein JB, Raber-Durlacher JE, Migliorati CA, McGuire DB, Hutchins RD, Peterson DE. Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer. 2007. 109:820–831.

28. McGuire DB, Correa ME, Johnson J, Wienandts P. The role of basic oral care and good clinical practice principles in the management of oral mucositis. Support Care Cancer. 2006. 14:541–547.

29. Mahood DJ, Dose AM, Loprinzi CL, Veeder MH, Athmann LM, Therneau TM, Sorensen JM, Gainey DK, Mailliard JA, Gusa NL, et al. Inhibition of fluorouracil-induced stomatitis by oral cryotherapy. J Clin Oncol. 1991. 9:449–452.

30. Anderson H, Scarffe JH, Sutton RN, Hickmott E, Brigden D, Burke C. Oral acyclovir prophylaxis against herpes simplex virus in non-Hodgkin lymphoma and acute lymphoblastic leukaemia patients receiving remission induction chemotherapy. A randomised double blind, placebo controlled trial. Br J Cancer. 1984. 50:45–49.

31. Saral R, Ambinder RF, Burns WH, Angelopulos CM, Griffin DE, Burke PJ, Lietman PS. Acyclovir prophylaxis against herpes simplex virus infection in patients with leukemia. A randomized, double-blind, placebo-controlled study. Ann Intern Med. 1983. 99:773–776.

32. Okuno SH, Foote RL, Loprinzi CL, Gulavita S, Sloan JA, Earle J, Novotny PJ, Burk M, Frank AR. A randomized trial of a nonabsorbable antibiotic lozenge given to alleviate radiation-induced mucositis. Cancer. 1997. 79:2193–2199.

33. Okuno SH, Woodhouse CO, Loprinzi CL, Sloan JA, LaVasseur BI, Clemens-Schutjer D, Swan D, Axvig C, Ebbert LP, Tirona MR, Michalak JC, Pierson N. Phase III controlled evaluation of glutamine for decreasing stomatitis in patients receiving fluorouracil (5-FU)-based chemotherapy. Am J Clin Oncol. 1999. 22:258–261.

34. Barasch A, Peterson DE, Tanzer JM, D'Ambrosio JA, Nuki K, Schubert MM, Franquin JC, Clive J, Tutschka P. Helium-neon laser effects on conditioning-induced oral mucositis in bone marrow transplantation patients. Cancer. 1995. 76:2550–2556.

35. Cowen D, Tardieu C, Schubert M, Peterson D, Resbeut M, Faucher C, Franquin JC. Low energy Helium-Neon laser in the prevention of oral mucositis in patients undergoing bone marrow transplant: results of a double blind randomized trial. Int J Radiat Oncol Biol Phys. 1997. 38:697–703.

36. Sartori S, Trevisani L, Nielsen I, Tassinari D, Panzini I, Abbasciano V. Randomized trial of omeprazole or ranitidine versus placebo in the prevention of chemotherapy-induced gastroduodenal injury. J Clin Oncol. 2000. 18:463–467.

37. Komaki R, Lee JS, Kaplan B, Allen P, Kelly JF, Liao Z, Stevens CW, Fossella FV, Zinner R, Papadimitrakopoulou V, Khuri F, Glisson B, Pisters K, Kurie J, Herbst R, Milas L, Ro J, Thames HD, Hong WK, Cox JD. Randomized phase III study of chemoradiation with or without amifostine for patients with favorable performance status inoperable stage II-III non-small cell lung cancer: preliminary results. Semin Radiat Oncol. 2002. 12:46–49.
38. Lee D, Jain VK. The use of recombinant human keratinocyte growth factor (palifermin) to ameliorate treatment-induced mucositis. Support Cancer Ther. 2003. 1:20–22.

39. Brizel DM, Murphy BA, Rosenthal DI, Pandya KJ, Gluck S, Brizel HE, Meredith RF, Berger D, Chen MG, Mendenhall W. Phase II study of palifermin and concurrent chemora-diation in head and neck squamous cell carcinoma. J Clin Oncol. 2008. 26:2489–2496.

40. Wu HG, Song SY, Kim YS, Oh YT, Lee CG, Keum KC, Ahn YC, Lee SW. Therapeutic effect of recombinant human epidermal growth factor (rhEGF) on mucositis in patients undergoing radiotherapy, with or without chemotherapy, for head and neck cancer: a double-blind placebo-controlled prospective phase 2 multi-institutional clinical trial. Cancer. 2009. 115:3699–3708.

41. Common Terminology Criteria for Adverse Events v3.0 (CTCAE). Cancer Therapy Evaluation Program, National Cancer Institute;
http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download