Abstract
Overactive bladder (OAB) is a medical condition characterized by urgency, with or without urge urinary incontinence, frequency, and nocturia in the absence of genitourinary pathologies or metabolic factors that can explain these symptoms. The current management of OAB is complex, and a wide range of options for conservative treatment have been offered, including bladder training, biofeedback, behavioral changes, oral or intravesical anticholinergic agents, S3 sacral neuromodulation, and peripheral electrical stimulation. The clinical efficacies of these treatments remains an open issue, and several experimental and clinical studies have been carried out during the last years. However, a minor group of OAB patients prove to be refractory to these conservative managements and need further evaluation involving sophisticated urodynamic testing and cystoscopy to carefully define the nature of the lower urinary tract dysfunction and to rule out other causes underlying the symptoms. Thus, the management of refractory OAB, which accounts for 10% of the whole spectrum of OAB, is extremely difficult. The aforementioned therapeutic tools have not always been completely satisfactory in these refractory OAB. Here, the author reviews the mechanism of micturition reflex and the current therapies, particularly highlighting the potential benefit of neuromodulation for refractory OAB.
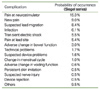
Figures and Tables
References
1. Bernstein AJ, Peters KM. Expanding indications for neuromodulation. Urol Clin North Am. 2005. 32:59–63.

2. Aboseif S, Tamaddon K, Chalfin S, Freedman S, Kaptein J. Sacral neuromodulation as an effective treatment for refractory pelvic floor dysfunction. Urology. 2002. 60:52–56.

3. Groen J, Bosch JL. Neuromodulation techniques in the treatment of the overactive bladder. BJU Int. 2001. 87:723–731.

5. de Groat WC, Araki I, Vizzard MA, Yoshiyama M, Yoshimura N, Sugaya K, Tai C, Roppolo JR. Developmental and injury induced plasticity in the micturition reflex pathway. Behav Brain Res. 1998. 92:127–140.

6. de Groat WC, Ryall RW. The identification and characteristics of sacral parasympathetic preganglionic neurones. J Physiol. 1968. 196:563–577.

8. Leng WW, Chancellor MB. How sacral nerve stimulation neuromodulation works. Urol Clin North Am. 2005. 32:11–18.

9. Kruse MN, Noto H, Roppolo JR, de Groat WC. Pontine control of the urinary bladder and external urethral sphincter in the rat. Brain Res. 1990. 532:182–190.

10. de Groat WC, Theobald RJ. Reflex activation of sympathetic pathways to vesical smooth muscle and parasympathetic ganglia by electrical stimulation of vesical afferents. J Physiol. 1976. 259:223–237.

11. Yoshimura N, de Groat WC. Neural control of the lower urinary tract. Int J Urol. 1997. 4:111–125.

12. Schmidt RA, Jonas U, Oleson KA, Janknegt RA, Hassouna MM, Siegel SW, van Kerrebroeck PE. Sacral Nerve Stimulation Study Group. Sacral nerve stimulation for treatment of refractory urinary urge incontinence. J Urol. 1999. 162:352–357.

13. Hassouna MM, Siegel SW, Nyeholt AA, Elhilali MM, van Kerrebroeck PE, Das AK, Gajewski JB, Janknegt RA, Rivas DA, Dijkema H, Milam DF, Oleson KA, Schmidt RA. Sacral neuromodulation in the treatment of urgency-frequency symptoms: a multicenter study on efficacy and safety. J Urol. 2000. 163:1849–1854.

14. Jonas U, Fowler CJ, Chancellor MB, Elhilali MM, Fall M, Gajewski JB, Grunewald V, Hassouna MM, Hombergh U, Janknegt R, van Kerrebroeck PE, Lylcklama a nijeholt AA, Siegel SW, Schmidt RA. Efficacy of sacral nerve stimulation for urinary retention: results 18 months after implantation. J Urol. 2001. 165:15–19.

15. Siegel SW, Catanzaro F, Dijkema HE, Elhilali MM, Fowler CJ, Gajewski JB, Hassouna MM, Janknegt RA, Jonas U, van Kerrebroeck PE, Lycklama a Nijeholt AA, Oleson KA, Schmidt RA. Long-term results of a multicenter study on sacral nerve stimulation for treatment of urinary urge incontinence, urgency-frequency, and retention. Urology. 2000. 56:6S. 87–91.

16. Pettit PD, Thompson JR, Chen AH. Sacral neuromodulation: new applications in the treatment of female pelvic floor dysfunction. Curr Opin Obstet Gynecol. 2002. 14:521–525.

17. Spinelli M, Bertapelle P, Cappellano F, Zanollo A, Carone R, Catanzaro F, Giardiello G, De Seta F. Gins Group. Chronic sacral neuromodulation in patients with lower urinary tract symptoms: results from a national register. J Urol. 2001. 166:541–545.

18. Hedlund H, Schultz A, Talseth T, Tonseth K, van der Hagen A. Sacral neuromodulation in Norway: clinical experience of the first three years. Scand J Urol Nephrol Suppl. 2002. 210:87–95.

19. Siegel SW. Management of voiding dysfunction with an implantable neuroprosthesis. Urol Clin North Am. 1992. 19:163–170.
20. Janknegt RA, Weil EH, Eerdmans PH. Improving neuromodulation technique for refractory voiding dysfunctions: two-stage implant. Urology. 1997. 49:358–362.

21. Chai TC, Mamo GJ. Modified techniques of S3 foramen localization and lead implantation in S3 neuromodulation. Urology. 2001. 58:786–790.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download