Abstract
Radiosurgery is a highly precise form of radiation therapy for the treatment of vascular lesions, certain primary or metastatic neoplasms, or functional disorders. Either intracranial or extracranial, which are inaccessible or unsuitable for surgical or other management. As the basis of radiation physics for radiosurgery, this article introduces radiation history, the method of radiation production, interaction mode of radiations with human, transfer of radiation energy to the tissue, and dose planning to generate a desirable dose distribution on the target site. Biologically, the goal of radiosurgery is to cause a precise damage only to the limited tissue within the target volume without exceeding the acceptable rate of complications. As the therapeutic ratio is a function of the volume irradiated, the total dose and dose per fraction used, and the level of acceptable risk, radiation oncologists or practitioners should consider various radiobiologic factors when using radiosurgery to obtain the maximum therapeutic ratio.
Figures and Tables
Figure 1
Schematic diagram illustrating parts of radiation physics involved in radiosurgery. In order to understand the principle of radiosurgery four parts of radiation physics principles are involved in the radiosurgery procedure: radiation production; interaction with matter; dose deposition; and dose planning.

Figure 3
Schematic diagram illustrating the interaction mode from X or γ-ray. X or γ-ray interact with the absorber to produce high speed electrons by three important mechanisms known as the photoelectric effect, Compton scattering, and pair production. The high speed electron produces a track along which ionization and excitation of atoms occur, and molecular bonds are broken, resulting in chemical change and finally producing biological damage.

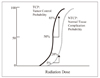
Figure 4
Comparison of dose distribution for three different radiations (Co-60 γ-ray, 6MV X-ray, proton). If the target is located in deep seated area in the patient, γ-rays and x-rays would be unsatisfactory since they deposit more dose outside the target region than within it. By contrast, the single proton beam deposits more dose to the target than to the normal tissues along its entry path (10).
References
1. Coffey RJ, Lunsford LD. Winn HR, Mayberg MR, editors. Stereotactic radiosurgery using the 201 cobalt-60 source Gamma Knife. Neurosugery clinics of north america. 1990. Philadelphia: WB Saunders Company;933–954.

2. Levy RP, Fabrikant JI, Frankel KA, Phillips MH, Lyman JT. Winn HR, Mayberg MR, editors. Charged-particle radiosurgery of the brain. Neurosugery clinics of north america. 1990. Philadelphia: WB Saunders Company;955–990.

3. Friedman WA. Winn HR, Mayberg MR, editors. LINAC radiosurgery. Neurosugery clinics of north america. 1990. Philadelphia: WB Saunders Company;991–1008.

4. Romanelli P, Heit G, Chang SD, Martin D, Pham C, Adler J. Cyberknife Radiosurgery for Trigeminal Neuralgia. Stereotact Funct Neurosurg. 2003. 81:105–109.

5. Turner JE. Turner JE, editor. About atomic physics and radiation. Atoms, radiation, and radiation protection. 1995. 2nd ed. Hoboken: John Wiley & Sons;1–13.

6. Gerward L. Paul Villard and his Discovery of Gamma Rays. Physics in Perspective. 1999. 1:367–383.

7. Khan FM. Khan FM, editor. Clinical Radiation Generators. The physics of radiation therapy. 1994. 2nd ed. Baltimore: Williams & Wilkins;45–68.
8. Johns HE, Cunningham JR. Johns HE, Cunningham JR, editors. The interaction of inoizing radiation with matter. The physics of radiology. 1983. 4th ed. Springfield: Charles C Thomas Publisher;133–166.
9. Bova FJ. Winn HR, Mayberg MR, editors. Radiation Physics. Neurosugery clinics of north america. 1990. Philadelphia: WB Saunders Company;909–931.

10. Lutz W. Alexander E, Loeffler JS, Lunsford LD, editors. Radiation physics for radiosurgery. Stereotactic radiosurgery. 1993. 1st ed. New York: McGraw-Hill;7–15.
11. Leksell L. The stereotaxic method and radiosurgery of the brain. Acta Chir Scand. 1951. 102:316–319.
12. Leksell L. Cerebral radiosurgery: Gammathalamotomy in two cases of intractable pain. Acta Chir Scand. 1968. 134:585–595.
13. Marks JE, Baglan RJ, Prassad SC, Blank WF. Cerebral radionecrosis: incidence and risk in relation to dose, time, fractionation and volume. Int J Radiat Oncol Biol Phys. 1981. 7:243–252.

14. Marks LB, Spencer DP. The influence of volume on the tolerance of the brain to radiosurgery. J Neurosurg. 1991. 75:177–180.

15. Kutcher GJ, Burman C, Brewster L, Goiten M, Mohan R. Histogram reduction method for calculating complication probabilities for three-dimensional treatment planning evaluations. Int J Radiat Oncol Biol Phys. 1991. 21:137–146.

16. Nakamura JL, Verhey LJ, Smith V, Petti PL, Lamborn KR, Larson DA, Wara W, McDermott MW, Sneed PK. Dose conformity of gamma knife radiosurgery and risk factors for complications. Int J Radiat Oncol Biol Phys. 2001. 51:1313–1319.

17. Kjellberg RN, Hanamura TA, Davis KR, Lyons SL, Adams RD. Bragg-peak proton-beam therapy for arteriovenous malformations of the brain. N Engl J Med. 1983. 309:269–274.

18. Loeffler JS, Alexander E, Siddon RL, Saunders WM, Colemen CN, Winston KR. Stereotactic radiosurgery for intracranial arteriovenous malformations using a standard linear accelerator. Int J Radiat Oncol Biol Phys. 1989. 17:673–677.

19. Eric J, Hall JB. Radiobiology for the radiologist. 2000. 5th ed. Philadelphia: Lippincott Company;67–111.
20. Hall EJ, Brenner DJ. The radiobiology of Radiosurgery: rationale for different treatment regimens for AVMs and malignancies. Int J Radiat Oncol Biol Phys. 1993. 25:381–385.

22. Flickinger JC, Kondziolka D, Pollock B. Complications from arteriovenous malformation radiosurgery: multivariate analysis and modeling. Int J Radiat Oncol Biol Phys. 1997. 38:485–490.

23. Kondziolka D, Niranjan A, Lunsford LD, Flickinger JC. Radiobiology of radiosurgery. Prog Neurol Surg. 2007. 20:16–27.

24. Buatti JM, Friedman WA, Theele DP, Bova FJ, Mendenhall WM. The lazaroid U-74389G protects normal brain from stereotactic radiosurgery-induced radiation injury. Int J Radiat Oncol Biol Phys. 1996. 34:591–597.

25. Hornsey S, Morris CC, Myers R. The relationship between fractionation and total dose for X-ray induced brain damage. Int J Radiat Oncol Biol Phys. 1990. 18:1437–1442.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download