Abstract
Male factors can be identified as the cause of infertility in 30~40% of couples and a contributing factor in 50% of cases. This situation means the reproduction ability in human is directly related not only to the underlying diseases of infertility but also to the general health status. Therefore, clinical approaches should be made by a comprehensive evaluation including a detailed history, careful physical examination, qualified semen analysis, and second-line specific tests under a thorough understanding of the anatomy and physiology of the reproductive organ, on both sides of the couple in parallel. Additionally, it is very important to evaluate male factors with rapid, noninvasive, and cost-effective modalities. This article will provide a review of clinical causes of male infertility as well as how to perform a comprehensive evaluation in infertile couples.
Figures and Tables
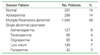
Table 3
Reference values of semen analysis

*Multicentre population-based studies utilizing the methods of morphology assessment in this manual are now in progress
Data from assisted reproductive technology programmes suggest that, as sperm morphology fails below 15% normal forms using the methods and definitions descrived in this manual, the fertilization rate in vitro decreases
References
1. Park NC, Park YS, Hwang KH, Chung MK, Yoon JB. Male Infertility: The Clinicostatistical Analysis of Recent 10 Years Cumulative Data. Korean J Urol. 1996. 37:939–946.
2. Lee HY. Andrology (Korean edition). 1987. Seoul: Seoul National University Press;40–88.
3. The Korean Andrological Society. Textbook of Andrology (Korean edition). 2003. Seoul: Koonja Publishing;11–98.
4. The Korean Urological Association. Urology (Korean edition). 2001. 3rd ed. Seoul: Korea Medical Book Publisher;510–518.
5. Nieschlag E, Behre HM, editors. Andrology: Male reproductive health and dysfunction. 2000. 2nd ed. New York: Springer;90–124.
6. Peter JB, Christopher GS, Larry IL. Comprehensive office evaluation in the new millenium. Urol Clin N Am. 2002. 29:873–894.
7. Tanagho EA, McAninch JW, editors. Smith's general urology. 2004. 6th ed. San Francisco: Lange;678–712.
8. Mark S, Jonathan PJ. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Male Infertility. Campbell-Walsh Urology. 2007. 9th ed. Philadelphia: WB Saunders;609–653.
9. Park NC. Genetic aspect of azoospermia: diagnosis and counseling. Kor J Fertil Steril. 2001. 28:S. 45–56.
10. Lee HJ, Park NC. Analysis of Chromosomal Abnormality in Male Infertility. Korean J Urol. 1998. 39:396–402.
12. Kim SW, Kim KD, Paick JS. Microdeletions within the azoospermia factor subregions of the Y chromosome in patients with idiopathic azoospermia. Fertil Steril. 1999. 72:349–353.

13. World Health Organization. The influence of varicocele in parameters of fertility in a large group of men presenting to infertility in a large group of men presenting to infertility clinics. Fertil Steril. 1987. 57:1289–1293.
14. Paduch DA, Skoog SJ. Current management of adolescent varicocele. Rev Urol. 2001. 3:120–133.
15. Kolettis PN, Sabenegh E. Significant medical pathology discovered during a male infertility evaluation. J Urol. 2001. 166:178–180.

16. World Health Organization. WHO manual for the standardized investigation, diagnosis and management of the infertile male. 2000. 1st ed. Cambridge: Cambridge University Press.
17. World Health Organization. Laboratory manual for the examination of human semen and sperm cervical mucus interaction. 1999. 4th ed. Cambridge: Cambridge University Press.
18. Park NC. Sperm banking. Kor J Fertil Steril. 1997. 24:S. 30–39.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download