Abstract
We performed biomechanical comparison of a xenograft bone plate-screw (XBPS) system for achieving cadaveric lumbar transpedicular stabilization (TS) in dogs. Twenty dogs' cadaveric L2-4 lumbar specimens were harvested and their muscles were removed, but the discs and ligaments were left intact. These specimens were separated to four groups: the L2-4 intact group as control (group I, n = 5), the L3 laminectomy and bilateral facetectomy group (LBF) (group II, n = 5), the LBF plus TS with metal plate-screw group (group III, n = 5) and the LBF plus TS with XBPS group (group IV, n = 5). Five kinds of biomechanical tests were applied to the specimens: flexion, extension, left-right bending and rotation. The averages of the 16 stiffness values were calculated and then these were statistically analyzed. The statistical results show that the XBPS system contributes spinal stability and this system can be a good choice for achieving TS.
Since Roy-Camille first introduced the pedicle screw system for achieving stability in the spine, various type instruments have been developed for transpedicular stabilization (TS) [7]. Of these instruments, the bone screw-plate is an effective, reliable instrument for TS [6]. The transpedicular system was first described by Boucher [2], and the pedicle system was first used by Harrington [4] for spinal stabilization. The pedicle systems provide stabilization between the vertebral segments and so it contributes to fusion [8,9].
It has been reported that xenograft bones can be used in spinal surgery and xenograft bones contribute to osteoinduction and osteogenesis; they help the fusion formation between the segments more than metal instruments do during a long time period after spinal surgery [1]. However, the ideal integrity and stiffness values of these systems were not mentioned previously by an in vitro study [1]. In addition, to the best of our knowledge, the xenograft bone plate-screw (XBPS) system for lumbar transpedicular stabilization has not previously been reported on by any in vitro study in dogs. Therefore, this study aimed to show the contribution of the XBPS system for achieving transpedicular stabilization of L2-4 lumbar dog cadaveric specimens following laminectomy and bilateral facetectomy.
Twenty dog's cadaveric L2-4 lumbar specimens (all were large breeds of approximately the same size and all the dogs were non-pathologic) were harvested and their muscles were removed, but the discs and ligaments were left intact in the specimens. These specimens were separated into four groups of equal size: the L2-4 intact group as control (group I, n = 5), the L3 laminectomy and bilateral facetectomy (LBF) group (group II, n = 5), the LBF plus TS with the metal plate-screw (MPS) system group (group III, n = 5) and the LBF plus TS with the XBPS system group (group IV, n = 5).
The XBPSs were prepared from cadaveric cattle tibia. The screws were machined to a conical form with a width of 4 mm, a length of 3 cm and a pitch of 1 mm (Yunnan Machine Tool Works, China). The plates were rectangular and their sizes were machined to 5.5-6 cm long with a width of 1 cm and a thickness of 3 mm (Yunnan Machine Tool Works, China) (Fig. 1A). The metal screws and plates had same size as the XBPSs' (Fig. 1B). Neither the XBPSs nor MPSs had any specific preparation after they were machined.
Preparation of the specimens included only dissection of the lumbar muscles, but the discs, ligaments and other tissues were kept intact from the dissection. The specimens in group I were tested following preparation. LBF was performed on the group II specimens to create instability. In group III and group IV, the L2-4 facet surfaces were flattened after LBF to place the plates and we drilled through the pedicle and vertebral corpus. The plates were placed on this surface and screwed to the pedicle. The xenograft and metal screws were firmly tightened with a screwdriver.
A tensile-compression testing machine (Hounsfield Test Equipment, UK) was used for the biomechanical tests (Fig. 2A). The specimens were tested under five different kinds of load: flexion, extension, left and right bending and rotation. A special apparatus shown in Fig. 2B was prepared for transforming the vertical movement to the moment load.
The movements performed for the tests were non-destructive, and rotation was the last test because rotation was the most stressful test for loosening and instability.
The load values were recorded in 1 mm intervals up to 16 mm; using the moment-force relation, the forces were converted to the moment with using the radian angle definition, and the displacements were converted to angles (Fig. 3). The small angle assumption was used for simplification of the conversion.
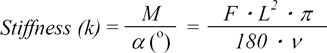
The stiffness values of each specimen were calculated in two steps:
Where (v) =1, 2, 3... 16
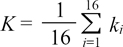
Second, the average of these 16 stiffness values was obtained as the overall stiffness of the specimen:
In the range of movements mentioned above, there was an almost linear relation between the angle and moment. Therefore, stiffness was considered as constant in this range of movement. The slope of the least square fit line of the displacement-force curve yielded the same stiffness value along with the average of the stiffness values.
The stiffness values of each specimen for the different loadings were acquired and then this acquired data was statistically evaluated in two steps: First; for classification of the data, the software (Statistica'99; StatSoft, USA) was used and the classification was performed with applying the Euclidian distance. The Euclidian distance provided four main clusters (Fig. 4). Second, by taking the average of 3 specimens, each group was represented by a unique stiffness value and these values are illustrated as a bar graphic in Fig. 5 and the error bars represent the standard deviation.
After applying the Euclidian distance, the similarities of the groups were 95% for group I, 90% for group II, 72% for group III and 83% for group VI (Fig. 4). A summary of the results of this data is shown below. The average stiffness values and standard deviations of group I, II, III and IV are given in Fig. 5.
The rotation test had higher stiffness values than the other tests (Fig. 5) because it was the most restrictive test in the lumbar zone.
As can be clearly seen from Fig. 5, of all groups, group III was the stiffest group and group II was the weakest group for all the movements. The average stiffness value of group II was 46% lower than that of group I, which indicated an instability problem. Compare to group I, group III had maximum stiffness values for right bending (279%) and minimum stiffness values for rotation (47%).
The stiffness values of group IV were not higher than those of group III, except for rotation. Compare to group I, group IV had maximum stiffness values at right bending (114%) and minimum stiffness values in flexion (25%). But, for the average stiffness values of all the tests, group III was 131% stiffer than group I, and group IV was 47% stiffer than group I. Considering the all biomechanical data, except that at rotation, group IV showed the best stability.
Transpedicular bone plate-screw systems have been used for spinal stabilization, but there is no consensus about the reliability and clinical application of these systems [6]. In addition, there have been no answers with the detailed information on which instrument is the best choice in spinal surgery. All the systems include screws, connecter rods, plates and crossing connecters, but the optimum rigidity of these systems is still unclear [1]. Therefore, the stiffness values of the XBPS (group IV) in the TS of the L2-L4 cadaveric dog lumbar specimens were biomechanically compared in this study. Clinic stability of the spine has been described as prevention of spinal displacement and damage to the nerves root and spinal cord from surgical trauma and other etiologic causes [10]. Clinically, it is difficult to describe the spinal stability in the normal spine [3]. Hence, the group I stiffness values were used as a control group and this group data was evaluated as the normal stiffness values. Taking these stiffness values into consideration, we carried out biomechanical and statistical comparisons of the groups in this study. Instability is abnormal movements of the vertebral segments with the forces that it can be applied during a clinical examination [10]. Many lumbar spine pathologies (cyphosis, scoliosis, disc pathologies, bone tumors, non-dislocated fractures degenerative vertebral disease etc.) and invasive spinal surgery procedures (multi-segment laminectomy, corpectomy, facetectomy etc.) can cause instability of the vertebral segments [3,5]. In this presented study, LBF was performed in group II to create instability on the lumbar segments, and the biomechanical results showed that group II was the weakest group with the lowest stiffness values for all the movements. The average stiffness values in group II were 46% lower than those of group I, and the latter group was considered to have an instability problem.
It has been emphasized in several reports that the MPS systems provide maximum rigidity when the external load increases on the spine [1,10]. In this study, of all the groups, group III was the stiffest group. Using the average stiffness values of all the tests, group III was 131% stiffer than group I and group IV was 47% stiffer than group I.
In TS, the usage of the MPS system has some disadvantage such as loosening, bending, breaking or pulling out of the screws and plates, and the maximum inter-segmental rigidity and abnormal loading on the non-stabilized segments [1,10]. Therefore, as was reported by Benzel [1], the usability of bone as a spinal implant or instrument in the spinal surgery is possible. Compare to the group I average stiffness values, the use of the XBPS system in group lV played an important role in TS.
As a conclusion, considering the maximum stiffness values of group III and the disadvantages of the MPS system, the XBPS system with its excellent stiffness values can be a good choice for achieving TS.
Figures and Tables
Fig. 1
(A) Xenograft bone plates and screws used for transpedicular stabilization. (B) Metal plates and screws used for transpedicular stabilization.
References
1. Benzel EC. Biomechanics of Spine Stabilization: Principles and Clinical Practice. 1995. New York: McGraw-Hill;89–107.
3. Brodke DS, Bachus KN, Mohr RA, Nguyen BK. Segmental pedicle screw fixation or cross-links in multilevel lumbar constructs. a biomechanical analysis. Spine J. 2001. 1:373–379.

4. Harrington PR. The management of scoliosis by spine instrumentation: An evaluation of more than 200 cases. South Med J. 1963. 56:1367–1377.
5. Hasegawa K, Takahashi HE, Uchiyama S, Hirano T, Hara T, Washio T, Sugiura T, Youkaichiya M, Ikeda M. An experimental study of a combination method using a pedicle screw and laminar hook for the osteoporotic spine. Spine. 1997. 22:958–962.

6. Johnsson R, Axelsson P, Gunnarsson G, Strömqvist B. Stability of lumbar fusion with transpedicular fixation determined by roentgen stereophotogrammetric analysis. Spine. 1994. 24:687–690.

7. Kumano K, Hirabayashi S, Ogawa Y, Aota Y. Pedicle screws and bone mineral density. Spine. 1994. 19:1157–1161.

8. Myers BS, Belmont PJ Jr, Richardson WJ, Yu JR, Harper KD, Nightingale RW. The role of imaging and In Situ biomechanical testing in assessing pedicle screw pull-out strength. Spine. 1996. 21:1962–1968.

9. Sandén B, Olerud C, Petrén-Mallmin M, Larsson S. Hydroxyapatite coating improves fixation of pedicle screws. A clinical study. J Bone Joint Surg Br. 2002. 84:387–391.
10. White AA, Panjabi MM. Clinical Biomechanics of the Spine. 1990. Philadelphia: Lippincott;84–126.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download