Acupuncture is sensory stimulation that affects the central nervous system by increasing the release of neuropeptides from nerve endings [2,9]. Acupuncture and Chinese herbs are treatment methods used in Traditional Chinese Medicine (TCM). Acupuncture has been used for treatment of neurological [7] and musculoskeletal diseases such as intervertebral disk disease [6,10] and spinal cord injury [12,14]. The combination of acupuncture and Chinese herbs for treatment of intervertebral disk disease (IDD) is related in literature [4,13].
Cervical IDD represents 14 to 16% of the IDD that occurs in dogs [11]. Symptoms include severe pain and ataxia of pelvic limbs to tetraparesis. Non-ambulatory tetraparesis occurs in approximately 11% of dogs with cervical IDD [1]. The treatment of choice includes medical treatment for the first episode that does not exhibit severe paresis and surgical treatment when chronic pain or severe neurologic conditions exist [1,11].
According to TCM, the health of the body depends on energy or Qi. There are 2 opposite forms of Qi, Yin and Yang, which can be considered analogous to anabolism and catabolism, respectively. The functioning relationship between parasympathetic and sympathetic influences of the autonomic nervous system can also be compared to Yin and Yang, respectively [5].
According to TCM, IDD is considered a painful obstruction syndrome and related to stagnation of energy (Qi) and blood (Xue). This situation is often exacerbated by cold and windy weather conditions. Vertebral column diseases are related to kidney energetic deficiency of either Yin or Yang. Other conditions can also cause IDD, such as trauma and/or repetitive exercise, latent blood deficiency in the post estrus period, and a natural decline of Kidney energy that occurs in geriatric dogs [8,13]. This report describes clinical, myelographic and tomographic findings after a dog with cervical IDD underwent treatment with electroacupuncture and Chinese herbs.
A nine year old female miniature Pinscher weighting 4.1 kg was referred to the Faculty of Veterinary Medicine at the Veterinary Hospital of University of São Paulo. When the dog was referred it had a clinical evolution of 30 days and was presenting non-ambulatory tetraparesis and cervical pain. It was submitted to treatment (oral administration) composed of chloridrate of tramadol (Tramal; 2 mg/kg, 8 h; Pharmacia, Brazil), dypirone (Novalgina; 25 mg/kg, 8 h; Hoechst, Brazil), prednisone (Meticorten; 1 mg/kg, 12 h; Schering Plough, Brazil). Prednisone was replaced by meloxicam (0.1 mg/kg, 24 h; Maxicam, Brazil) with only pain control and without ambulation recovery. Neurological evaluation showed a cervical syndrome with increased spinal reflexes on the thoracic and pelvic limbs (superior neuron motor lesion), deep pain perception, no proprioception on the thoracic limbs and left pelvic limb, and increased spasticity of thoracic limbs. Additionally, the dog was incapable of sternal position.
Myelographic findings showed dorsal extradural compression at C1-C2 and C3-C4 and ventral extradural compression at C3-C4 (Fig. 1). A transverse computed tomography image confirmed extradural compression at C3-C4 (Fig. 2).
Because the owner did not want immediate surgical treatment, all conventional drugs were stopped and the dog was only treated with 10 electroacupuncture applications and Chinese herbal medicine. The acupuncture points and Chinese herbs were selected based on TCM diagnosis and the author's clinical experience. Clinical evaluation was conducted before each application, weekly, with the last 2 evaluations occurring at 14 day intervals.
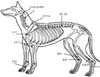
The acupuncture points (Fig. 3) used in this case were as follows: LI (Large Intestine) 4, LI11, GV (Governing Vessel) 14, LI15, BL (Bladder) 23, KI (Kidney) 3 transfixed with BL60, GB (Gallbladder) 39 transfixed with SP (Spleen) 6 and local cervical points. Pairs of acupuncture points were connected with an electrode to form a set, which was then subjected to current at a frequency of 3 Herz (Hz) alternated with 100 Hz for 3 sec each, over a period of 20 min [3]. LI4 and LI11, located on the same side, made up the first and second sets, GV14 and LI15, located on the right side, made up the third set, BL23 formed the forth set, KI3/BL60 and GB39/SP6 the fifth and sixth sets and the four cervical local points made up the seventh and eighth sets. The dog was positioned at a lateral recumbency and contained with the help of the owner. The animal underwent electroacupuncture once a week for 8 weeks, then every 14 days for the last 2 applications. The whole electroacupuncture treatment was performed during 12 weeks.
TCM diagnosis was performed by evaluation of clinical history and based on findings such as initial pain, tetraparesis, irregular estrus with a small amount of aqueous blood, weak femoral pulse, pale red tongue, the dog being chilly and having a large trunk, demonstrating aggressive behavior and chronic evolution of symptoms.
TCM diagnosis indicated a Qi and Xue deficiency shown by a weak pulse and pale tongue combined with the characteristics of estrus. The Qi/Xue deficiency may also have been facilitated by wind and cold invasion. GV14 was chosen to dispel wind and neck pain; LI4, LI11, LI15 and the local cervical points were chosen to alleviate Qi/Xue stagnation. TCM also diagnosed a Yang Qi deficiency of the kidneys due to vertebral column disease, chronic evolution, and the dog being chilly [8,13]. The acupuncture points BL23 and KI3 were chosen to enhance Kidney energy; BL60 was chosen as a distal point to alleviate the cervical problem by drawing out pathogenic Qi and placing healthful Qi into the bladder channel; GB 39 was used because it is an influential point for marrow and SP6 was used to disperse dampness and enhance Qi, Xue, Spleen and Kidney energies. The following traditional Chinese herbal formulas (Table 1) were chosen for treatment: Du Huo Ji Sheng Tang and Guei Fu Di Huang Wan, followed by a Xue tonic formula, Gui Pi Tang [13,15]. The first formula was chosen to expel wind and dampness, enhance kidney and liver energy, help Qi/Xue circulation and alleviate pain. To enable the first formula to enhance the Yang Qi of the kidneys, it was supplemented with Guei Fu Di Huang Wan. In addition to the two formulas described above, Gui Pi Tang was chosen to enhance Xue, due to a severe deficiency in the dog. The method of preparation is indicated by the last word in each formula,for example: Tang indicates that herbs were underwent decoction and Wan indicates that herbs were reduced to powder then mixed with rice or honey and made into pill form.
The dog exhibited lower spasticity of thoracic limbs after the first acupuncture treatment. One week after the first treatment the dog was capable of sternal position. Shortly before the third treatment the dog recovered support of pelvic limbs and intermittent support of thoracic limbs. The owner reported ambulation without assistance 15 days after the initial treatment. Before the fourth treatment the dog recovered proprioception of the left thoracic limb. Throughout the remaining 10 treatments, the dogs locomotion and proprioception improved and only a slight deficiency in the right thoracic limb persisted. After 6 months of follow-up the dog was stable in locomotion and proprioception and had no episodes of pain. The clinical evolution of this dog demonstrates that acupuncture and Chinese herbal treatment was responsible for its motor rehabilitation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download