Introduction
In April 1985 the first cases in the United Kingdom of a new disease of cattle were seen; bovine spongiform encephalopathy (BSE) which has commonly become known as "mad cow disease." This disease was characterized by gray matter vacuolation and fibrils similar to those observed in sheep scrapie [
10,
20]. Epidemiological studies established the most probable cause of the outbreak of the new disease as changes in the rendering process for the offal used in animal feed. This allowed some agent-either scrapie agent from infected sheep carcasses or a previously uncharacterized BSE agent-to contaminate high protein cattle feed [
22,
24]. Between 1981 and 1982 most of the rendering plants had changed their process such that there was no longer a solvent based fat-extraction step followed by steam distillation of the solvent. Solvents have been shown to inactivate the scrapie agent [
8]. Without the steam distillation step, the offal failed to reach the high steam temperature known to destroy the scrapie agent (138℃ for 1 hour 3 bars) [
3,
8,
19].
The change in offal processing preceded the subsequent outbreak of BSE in 1986-7. It is possible that the agent was always present in this type of feed, but that the reduction in fat content with hydrocarbons and the subsequent steam treatment of the product kept the number of infectious particles down so that a clinical disease was not seen (the disease symptoms being dose related). In Scotland, where the hydrocarbon extraction continued to be used during high protein feed production, the number cases of BSE was significantly fewer per head of cattle in England [
23].
The magnitude of the BSE epidemic was probably amplified by infected cattle being included in the rendering process. It does appear, however, that BSE is not readily transmitted either horizontally or vertically [
21], and as a result of feed ban in July 1988 the size of the epidemic has been self-limiting to a large extent [
24]. Indeed, the incidence of disease in cattle born after the feed ban took effect has dropped dramatically through years [
23,
24]. However, it is not clear whether or not maternal transmission of BSE does occur [
9].
The start of the BSE epidemic was followed by reports of spongiform encephalopathies in a variety of animals including many exotic animals housed in zoos and wildlife parks [
7,
12,
15,
26]. These infections were all associated with ruminant-derived feed [
13] or from maternal transmission [
12]. These infections all produced the same lesion profiles when injected into mice as BSE and feline spongiform encephalopathy (FSE) [
4]. The transmission of spongiform encephalopathy across the species barrier by oral dosing is of great concern to the government in all over the world. However, it appears that primates are protected by a considerable species barrier; indeed from transmission data with marmoset, primates are more likely to contact scrapie than BSE [
1]. Since epidemiological studies have never linked human transmissible spongiform encephalopathy (TSE) with exposure to sheep scrapie and transgenic mice expressing that human prion protein (PrP) are not more susceptible to BSE than non-transgenic controls [
6] it is possible that humans are not threatened by BSE zoonosis. In early 1996, however, the CJD (Creutzfeldt-Jakob disease) Surveillance Unit reported ten cases of a human TSE; CJD in unusually young patients [
25], which prompted the European Union (EU) to ban export of British beef and beef derived products in world-wide. Mouse transmission and strain typing studies from four of these cases are performed at the Institute of Animal Health. These results showed the same lesion profiles when injected info mice as BSE [
2,
5].
In this review cases of Japanese BSE are reported. Risk Assessment and Risk Management in the Japanese BSE incidents are discussed.
History of Japanese BSE
In January 2001, Japan banned the import of beef and processed beef products from 18 countries, including those in EU, to prevent BSE from entering Japan. Scientific Steering Committee (SSC), which is in charge of nutritional safety in the EU, evaluated the risk-level of BSE in Japan as three on a scale of one to four according to the sources close to the SSC, but the report has yet to materialize.
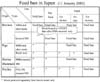
On August 6, 2001, one five-year-old milking cow was slaughtered at the abattoir which showed difficulty in standing. We examined the brain at the National Institute of Animal Health (NIAH) and according to the results, we confirmed August 15 it was negative, but later on, we carried out brain tissue tests in which we found spongy lesions in the tissue of the brain (
Table 1).
The sample was delivered to the Institute again, and the Institute confirmed the presence of the holes, and then we confirmed signs of (BSE) positive on September 10 through another test, such as Bio-Rad ELISA and Prionics.
British government scientists determined that a 5-year-old Holstein at a dairy farm in Shiroi, near Tokyo, carried the disease, formally called bovine spongiform encephalopathy, or BSE.
Accordingly, Japanese Government, Ministry of Agriculture, Forestry and Fisheries (MAFF) reported first Japanese Case to OIE (World Organization for Animal Health), as written below.
Disease Name: Bovine Spongiform Encephalopathy
(suspicion) Code: B115
Suspicion: A five year old Holstein cow kept on a dairy farm in Chiba prefecture was slaughtered on 6 August 2001 at an abattoir. As the cow had dystacia, a brain sample was taken and sent to the National Institute of Animal Health and subjected to Prionics Check Test with a negative result on 15 August. A brain sample from this cow was also sent to the prefecture Livestock Hygiene Service Center and subjected to histopathological examination and found to have vacuoles on 24 August. The same brain sample was sent to the NIAH on 6 September for histopathological examination with the same result. The same sample was subjected to immunohistochemical examination with a positive result on 10 September.
Measures taken: Immediately after the BSE is suspected, the herd has been placed under quarantine by the prefecture veterinary inspector.
On October 2 Ministry of Health, Labor and Welfare (MHLW) asked processed food manufacturers to stop using extract or enriched additives, such as beef essence and collagen, from cattle meat and bone as they may contain a pathogen that causes variant CJD (vCJD).
In November of 2001 beef prices in Tokyo have plummeted by 20 percent, and meat packing companies have started prominently labeling their imported beef as domestic beef, because Japanese Government compensated for their beef processed before October 18.
On December 1 the cow, slaughtered at a meat processing plant in Saitama Prefecture, is expected to be declared the nation's third case of BSE - following infected dairy cows found in Shiroi, Chiba Prefecture and Sarufutsu-mura, Hokkaido - at the meeting of experts. According to the ministry, the cow was raised by a dairy farmer in Miyagi-mura, Gumma Prefecture. When it turned five years and eight months of age, which is old for a dairy cow, it was sent to the slaughter house. The cow was tested for BSE before it was processed, but the test did not show anything clinically unusual, the officials said. However, after it was slaughtered, two tests on materials from the cow using the ELISA resulted in positive reactions on the same day. The test was conducted at a meat hygiene inspection center in Saitama. The MHLW Yokohama quarantine center conducted another test next day using the more accurate Western blot method, and the result was also positive.
On December 21 the Japanese Ministry then asked the EU to draw up another risk-assessment for BSE since Japan would be automatically designated as a country at high risk if Tokyo fails to make the request by the end of the year. In Japan, if you want consumers to regain confidence in meat products, you need absolute transparency, accountability and a trustworthy control system through the whole process (from breeding the cattle to inspecting their meat).
On December 25, 2001, in Japan, a poll conducted December 15-16 by the Yomiuri Shimbun newspaper found 68% of Japanese have stopped eating meat or are eating less beef since the farm ministry confirmed the first case of the disease in a cow in Chiba Prefecture on September 22.
Farm ministry investigations in September found 165 households in 15 prefectures in Japan engaged in livestock farming had fed MBM, as well as blood and bone meal feed, to a total of 5,129 cows. MBM was then officially banned for use in feeding cattle on September 18. It was also banned for other livestock on October 15.
Japanese Government Policy
Eight major policies were implemented since October 2001.
Surveillance in farm by veterinarian, 4.5mi cows/yr.
Prion test at healthy 1.3mi cows/yr. at this time there is no tracing system.
Elimination of SRM(specified risk material)
Ban of MBM (meat- and - bone meals) for production, sale use.
Prion test for fallen stocks. 100,000 cows (aged more than 24 months old)/yr. tests.
Transparent information and traceability.
-
New Measures
Food Safety Basic Law.
Government Reorganization (Food Safety Commission: FSC) (Table 2). Details of organization of FSC is shown in the same website (http://www.fsc.go.jp/english/index. html).
SRM removal
Removal of SRMs has been mandatory since October 2001, and being carried out at all slaughterhouses in Japan, as of March 2005. SRM removal is believed to cut the infectious doses by 99.4%. Therefore, if SRMs can be removed with complete certainty, the risk of meat becoming contaminated by BSE prions can be reduced dramatically [
17].
In Japan, use of cattle heads (excluding the tongue and cheek flesh), spinal cord, distal part of ileum, spinal column including dorsal root ganglion for food products is prohibited for all cattle by the law. However, it is not practical to consider that a complete SRM removal is implemented in slaughter houses because of the residual spinal cord left behind during spinal cord removal, possible contamination of dressed carcasses, and contamination of central nervous tissues by pitching. The result of surveillance concerning the removal rates of spinal cord before back-spreading in 7 Meat Hygiene Inspection Office directed by NHLW are as follows: 5 offices employing the spinal cord aspiration method indicated average 80.6 ± 17.1% (52.5~99.1%) and 2 offices employing the spinal cord extrusion method indicated average 75% (72.0, 78.0%). In addition, the residual spinal cord after back-spreading was disposed of manually [28]
Absence or presence of tissues other than SRM in which abnormal prion protein accumulates cannot be determined at this point because of the detection limit of the infection experiments by which SRM was identified and uncertainity derived from incomplete understanding of mechanisms underlying BSE infection. These ideas are supposed to be the grounds on which the World Health Organization recommends exclusion of any BSE-cattle tissue from the human food chain.
Traceability
In Japan, in December 2003, based on the "Special measures law on management and transmission of information for individual recognition of cattle", the traceability system has been made compulsory to document information, including birth record, which allows individual recognition at the production and slaughtering stages and determination of accurate ages. This allows a separate investigation on the degree of risk of BSE infections before or after implementation of various regulation.
In addition, this regulation has also been implemented at the distribution level since December 2004. Taking into account its significance to create transparency for consumer to directly obtain information of beef, securing and verification of the traceability system are deemed essential from now on.
Risk management
While BSE in cattle was first reported in 1986 in the United Kingdom, the first case in Japan was not detected until 2001. Since then, the Japanese Government has intensified BSE surveillance in cattle and located 19 more cases in subsequent years (
Table 3).
The experience in continental Europe shows that a comprehensive strategy in combating BSE is not available on the drawing board. Measures taken to resolve BSE incidences in Japan have to be persistently assessed, systematically modified and appropriately adapted to conditions in Japan.
As the first country to have detected BSE cases in Asia, Japan was obligated to promptly implement a variety of countermeasures after encountering the first BSE cases in cattle. Of many countermeasures, the most important approach focused on the feed issue; prompt imposition of a ban on specified high-risk raw materials such as brain- and spinal cord-derived meals was quickly adopted. Apart from the feed issue, we are still continuing to incorporate additional measures to neutralize BSE in Japan.
All the 20 BSE cases that have been diagnosed up to October 2005 were dairy cows. Of these, 16 cases were located at slaughterhouses while the remaining 4 cases were fallen farm-stock. Since unregulated imports of MBM from BSE-affected countries into Japan had been practiced extensively in the 80s and early 90s, contaminated feed were likely given to animals. If infected animals had not been diagnosed then, they might be eventually terminated as feed (SRM) and could have yielded domestically infected MBM; A raw material which is churned into homemade MBM would serve as a possible source of BSE dissemination in Japan.
The controversy in OIE recommendations of import and export of beef are the basics for conflicts within the framework of WTO/SPS (sanitary and phytosanitary agreement): if measures more stringent than the OIE recommendations are adopted, scientific arguments (risk assessment) have to be provided. While risk assessments for different countries are under evaluation, the GBR (geographical BSE risk) - assessment of the EU is currently being considered. With regard to the import bans - especially concerning beef - the risks of communication are very problematic. If Japanese beef is considered safe for consumption, it is difficult then to explain the status of American beef as being more risky than Japanese beef.
For the measures concerning consumer protection, we are considering a re-evaluation of the approach to testing young cattle. As suggested by some Swiss scientists, we have to provide details of the limitations of the test to consumers/retailers. Instead of beef, the brain of animals is tested with the possibility of detecting relevant BSE agents within the brain tissues, which in young animals approximates to zero. In fact, we are currently reviewing pithing in the slaughterhouse.
Beginning in 2004, we have implemented surveillance of all fallen stock (100,000 tests for cattle over 24 months of age) to establish an overall status of BSE-infection in Japan. The European experience has revealed that risk-bearing BSE cases harbor the infected animals (with clinical signs of BSE) in fallen stock and slaughtered adult cattle related to emergency/diseases; the probability of BSE infection in the risk-bearing population (including fallen stocks and emergency/disease-induced slaughtered adult cattle) is in fact 20 times higher than that of the normally slaughtered adult population. In our attempt to correlate the BSE incidence in risk-bearing populations, details of the actual fallen stock and emergency/disease-induced slaughtered adult cattle in Japan are now being reviewed.
After the finding of a BSE case in the United States (U.S.), an Ad Hoc Subcommittee (in response to BSE in the U.S.) of the Foreign Animal and Poultry Disease Advisory Committee was formed. The said subcommittee convened in Washington D.C. under the chairmanship of Prof. U. Kihm (Switzerland), and according to his report delivered to US government and explained in the Japanese FSC in March 2004, he recommended 5 objectives: ① reduce the risk of public health for consumer protection; ② limit recycling and amplification of BSE agents; ③ establish the level of effectiveness of measures through surveillance; ④ prevent any advertent introduction of BSE from abroad in the future; and ⑤ contribute to prevention of the epidemic on a global scale.
The proposed U.S. ban on SRM eliminates high-risk BSE tissues (i.e. SRM from cattle over 30 months of age) from food supplies to humans in accordance to the OIE standards. However, the said subcommittee recommended that specified SRM (derived from brains and spinal cords of cattle over 12 months of age) be excluded from both the human food chain and animal feed production lines. Until the levels of BSE risk have been established, the subcommittee meanwhile concedes that exclusion of central nervous system tissues, skulls and vertebral columns from cattle over 30 months of age as well as intestines from cattle of all ages for use in human food is a temporary rational compromise.
For the purpose of facilitating overall surveillance reliability, said subcommittee recommends testing all cattle older than 30 months of age in the above-mentioned high-risk populations, besides strengthening the passive surveillance system. Moreover, said subcommittee considers testing of all cattle slaughtered for human consumption (performed in Japan) to be unjustified in terms of protecting human and animal health. However, to support the overall surveillance system and encourage reporting to authorities at the farm level, random testing of healthy slaughtered cattle over 30 months of age should be strongly considered.
Said subcommittee acknowledges that the authorities have recognized the importance of effective identification and traceability systems, which usefully furnish not only the cost-effective means of rapidly tracing affected animals but for government compliance of said recommendations.
Since the outbreak of BSE in the U.S. a trade issue on dairy and beef products between the U.S. and Japan has developed. With regard to this issue, a Japan-U.S. BSE working group was established, and a final report was compiled on July 22, 2004. In this report, Japan asserts that the objectives of BSE testing are the elimination of infected cattle from the food chain to ensure the safety of meat for consumption. Meanwhile, the U.S. affirms that the OIE recognized the objectives of BSE testing to help define whether BSE is present in the U.S. cattle population, and if so, provide estimates of the level of BSE and monitor the effectiveness of BSE prevention and control measures. Taking into account the fact that the detection of abnormal prion proteins under a certain age (in months) is difficult through BSE testing, we emphasized implementation of a double check where SRM from all cattle should be removed to compensate for technical limitations of the testing as a fail-safe measure. Moreover, the U.S. reaffirms that SMR removal is indeed the best way to protect consumers from exposure to abattoir-derived BSE-infected cattle.
In this perspective, Japan and the U.S. agreed that SRM should be removed in such a manner as to avoid cross-contamination of edible tissue during slaughter, dressing, and processing. Removed SRM should be disposed of according to laws of the respective countries. The U.S. explained that the quality systems verification program of its Agriculture Marketing Service (AMS) is used to provide independent verification of industry management systems and other quality standards. This program could provide assurances that U.S. beef exported to Japan meets the prescribed safety requirements.
In this report, the U.S. provided scientific documentation that clearly demonstrated that cattle could be accurately monitored to ages of 30 months and more. In addition, the U.S. is embarking on a National Animal Identification System, whereby the age-in-month and identification of cattle can be precisely traced. The AMS quality systems verification programme can be used to certify exported beef and beef products that satisfied meat conditions required by Japan and the U.S. regulatory requirements.
Through discussion of a spectrum of controversial subjects within the working group, both parties converged on the following major requirements: ① that there is a limitation to 100% testing of consumption-destined animals; ② SRM elimination is extremely important for food safety; and ③ the risks of contamination by SRM in abattoirs have be neutralized. Other remaining subjects are opened for future discussion.
Because the media assumed that the Japan-U.S. negotiations focused merely on BSE testing and SRM elimination, they misinterpreted that the Japanese market was then opened to American beef when FSC agreed to the limitation of animal testing, and the ages for SRM elimination. They might have been misled by the emphasis of major issues on these two subjects in previous reports.
Along the same line of thought, the Japanese Consumer Association (JCA) misconceived that BSE-testing and SRM elimination were the basic measures for securing the safety of beef for consumption. In fact, some in the JCA are still insisting that "100% BSE-testing" is a prerequisite for the importation and distribution of domestic beef for consumption in Japan. Although the FSC has yet to make up its mind on abbreviation of the BSE-testing in young cattle, I would like to emphasize that there is no scientific basis to continue with the 100% BSE-test for securing the food safety levels for beef and relevant edible bovine products. Elimination of SRM can not guarantee the total safety of beef. At this moment, the extent of SRM risk has only been indicated by several reports employing tests with a limited sensitivity. There is still a possibility that the items in the SRM list will increase in the future, and this indiscriminately applies to Japanese cattle as well. Although current practices of SRM elimination partially guarantee total food safety, additional latent problems and imminent issues remain as potential headaches to be addressed. If the index of SRM elimination can not guarantee reliable food safety, we have but to resort to total elimination of tissues from high risk-bearing and BSE-infected animals. However, current BSE tests have their limitations and can not yet completely detect high-risk and/or infected animals. Under such circumstances, tissues/wastes and remains of diseased, affected fallen stocks and cohort animals have to be eliminated to prevent BSE invading the human food chain systems. The failure to detect any cohort should never be allowed to occur, and with regular and persistent updating of available stringent records, we are at least adopting the correct and useful approach as a reawakening strategy to securing food safety. In this perspective, traceability based on a National Identification System is required.
Abattoir compliance for the elimination of SRM is an issue different from cross-contamination of food and animal feed during processing. Restriction of this information coupled with limited communications on imminent risks may inflict damage on humans in a "worse and belated" fashion. Therefore, we have to stipulate guidelines for securing/standardizing food safety based on guaranteed traceability, elimination of cross-contamination of food and feed, as well as BSE-testing and abattoir compliances for total SRM elimination.
Control measures taken by Japanese government
OIE code requires the implementation of control measures as follows,
-
public awareness programs and contingency plans for BSE.
ban on feeding animals with ruminant by-products.
bovine spongiform encephalopathy surveillance programs.
diagnostic services, including the result of tests for BSE and transmissible spongiform encephalopathy (TSEs).
Details of measures are described accordingly.
A. Public awareness: programs and contingency programs
The public awareness programs include training courses, mass-communication media, publications, internet systems and meetings, but well organized awareness campaign seems to be required even in Japan. A contingency plan is available in the government office. It is considered essential to test the plans through stimulation exercises and training courses at regular intervals, and to review the plans annually.
B. Ban on feeding ruminants with feed stuffs derived from ruminants
In 1996, official instruction prohibited the use of feeds derived from ruminants. However, implementation of this official instruction is apparently incomplete. In 2001, a legal ban was imposed on feeds containing proteins from mammals for feeding ruminants (
Fig. 1). In April 1996, the Government issued an administrative guidance banning the use of products containing ruminant animal tissues, such as MBM in feed for ruminant animals. With regard to imported feed, even before October 2001, every feed importer has been obligated by Feed Safety Law to submit information including its name, the kinds of feed it imports and other details. However, because of compound feed production relies heavily on imported ingredients an accurate grasp of the extent of worldwide BSE contamination is lacking, raw materials used to manufacture compound and mixed feed will be added to risk factor. The use of MBM has been completely banned since October 2001.
C. Rendering of ruminant by-products
There are 21 rendering plants in Japan and approximately 320,000 tones for cattle, 704,000 tones for cattle, 576,000 tones of pig and 576,000 tones of poultry are rendered annually. Only 3.4% to 13.4% of these materials are steam-heated at 133℃ for 20 min at a pressure of 3 bar. OIE codes for production of bovine MBM require steam-heat at 133℃ for 20 min at a pressure of 3 bar. Even in these condition approximately 0.1% of BSE agents will survive after the steamed heat.
D. Notification of suspected cases of BSE and scrapie
In 1996 BSE and scrapie are notifiable in Japan and these have implemented routine surveillance programs [
14].
E. Diagnostic services
Japanese Government uses a combination of tests such as histopathology (HP), enzyme-linked immunosorbent assay (ELISA), Western blot (WB) and immunohistochemistry (IHC) (
Fig. 2).
National reference laboratory for BSE are located in Tsukuba: National Institute of Animal Health, and Tokyo: National Institute of Infectious Diseases. The development of simplified diagnostic kits for BSE should be encouraged with a view to reducing the cost of each test so as to drastically increase the number of tests not only in Japan but also in surrounding countries.
In May 2001, testing was initiated at slaughterhouses in Japan on cattle at risk.
Since October 2001, all slaughtered cattle in Japan undergoing an ELISA screening test, followed by a confirmation test using the Western blot method and a microscopic pathological/immunohistochemical examination. As of August 2005, approximately 5 million animals have undergone testing, resulting in fifteen cows testing positive for BSE infection.
Investigations for improvement and development of rapid BSE test methods are being employed in European countries, the U.S., and Japan. And rapid testing methods with greater sensitivity are expected to become available. It is considered that the lower the detection limit is, the younger the detectable BSE-cattle will be.
Moreover, demonstration of the presence or absence of infection before slaughtering can be expected if testing using tissues or blood samples removed from live cattle become available. This will allow the detection and exclusion of BSE cattle without bringing them into slaughter house and incurring the risk of SRM cross-contamination, and lead us close to the goal described in the report (16) by the SSC in EU: Exclude infected animals from the human food chain to protect consumers from the risk of BSE infection.
F. Focused efforts on key issues in TSE-research:
Focused efforts in TSE research in Europe will be supported on a limited number of key issues. The same manner is applied in Japanese Scientific Society and the Government. The projects must build critical mass and be designed to lead to rapid results. Research projects will be implemented through Concerted Actions, Thematic Networks, and RTD/Demonstration Projects. Projects should reflect dedicated efforts that clearly address one of the following issues:
① In vivo tests for pre-clinical diagnosis in humans and animals: Specific, sensitive methods to detect and quantify prion diseases (e.g. surrogate markers, prion-binding proteins or receptors, strain typing).
② Inactivation and prevention: Longevity of the agent including natural conditions (e.g. in pastures and soils); inactivation and disposal of contaminated material.
③ Animal TSEs and Transmission: BSE in sheep, differentiation of BSE from scrapie; PrPsc path from peripheral tissues to CNS; silent carriers: (existence mechanisms and infectivity in fluids and tissues).
④ Human TSEs and risk assessment: Risk assessment of actual human exposure to BSE (including possible regional aspects); mathematical modeling of the human epidemic; safety of human blood, organ transplants, therapeutics and surgical instruments; therapeutics and prophylaxis (e.g. preventive immunization).
Future of Japanese BSE
In Japan it clearly demonstrates the downward trend of positive BSE cases detected over the last years, with more than 50% reduction since 2004. Based on the improved situation, there could be a similation to have a roadmap on the BSE strategy in the short, medium and long-term. In setting on strategy the greatest importance is attached to maintaining the high level of consumer protection built up over the years in the field of prevention, control and eradication of TSEs. The balance of evidence is increasingly pointing toward the need to re-consider the current priorities in the field of food safety and animal health.
Amendment in the short and medium term (2006~2010)
A. Special Risk Material: Assure the safe removal of SRM but modify list/age based on new & evolving scientific opinion. The initial list of SRM was established based on the scientific knowledge before 1995 and the precautionally principal. Since then, the overall situation has been improved and new scientific data has become available. On 27-28 April 2005, the European Food Safety Authority (EFSA) adopted on opinion on SRM supporting an increase of the current age limit for central nervous tissue from 12 to 21 or 31 months depending on the significance given to the extremely rare BSE cases detected in young animals. This opinion allows us for reflection on an amendment of the current SRM list and in particular on the age limit for the removal.
B. Feed Ban: When certain conditions are met a relaxation of the certain measures of current total feed ban. A ban on the most of mammalian MBM to cattle, sheep and goat was introduced as of September 2001 (
Fig. 1). The starting point when revising the current feed ban should be risk-based but at the same time taking into account the control tools in place to evaluate and ensure the proper implementation of this feed ban. Currently there are no specific restriction with regard to use of domestic tallow in feed (or food) to prevent transmission of TSEs.
The restriction on the use of specified risk material is applicable to the mandatory purification of rendered fat at 0.15% insoluble impurities according to EC regulation No. 1774/2002. A possible need for future provisions on tallow, in particular for use in milk replacers, depends on the result of quantitative risk assessment.
C. Surveillance programs: Continue to measure the effectiveness of the measures in place with abattoir targeting of the surveillance activity. The goal of surveillance is monitoring the effectiveness of control measures such as the feed ban and SRM removal by following the evolution of BSE prevalence. It should be noted as well that, although active BSE monitoring is not a public health protection measure, it has contributed to increased consumer confidence and has played a role in the Risk Communication strategy in Japan. In addition the surveillance results have provided necessary data to evaluate an amendment of SRM. The gradual increase of age limit starting for healthy slaughtered animals and fallen stock. The increase of the age would depend on the results of the ongoing surveillance program.
D. Cohort culling in bovine animals: Strategic goal is to stop the immediate culling of the cohort. The cohort animals are animals without any symptoms but they are assumed to be at a higher risk of being infected with BSE due to an epidemiological link. This includes animals which received the same feed as the positive animal in the first year of their life. Reflection on alternatives to the current destruction of the cohort can be made. A proposed alternative would to deter the culling and destruction at the end of the productive life, as seen within the International OIE Animal Health Code or to allow the slaughtered animals into the food chain following a negative rapid testing result. Although this relaxation would allow breeding and use of milk, the decision to derogate from the culling should be the responsibility of the government in order to take into account of the potential consequences for their export markers. The derogation to defer the culling would be the government's decision. This relaxation would not endanger the current level of consumer protection. A relaxation would not only reduce the economical impact but also the social consequences following the complete destruction of the cohorts being often one of the main reasons to object to the culling policy. However, as the BSE prevalence reduces, the total herd culling for destruction may be the preferred option, in particular to trade to the countries where BSE was absent or very rare.
Amendments in the long-term (2010~)
In case the positive trend continues, taking into account the relaxation of the measures in the short and medium term, further relaxation of measures can be envisaged.
A. Surveillance: The gradual decrease in the level of surveillance can be maintained if the positive trend continues focusing on older animals or birth cohorts from which only limited information is available.
If only BSE cases are detected in animals above 10 years, i.e. born before 1 January 2002, it may be decided to exclude those animals permanently from the feed and food chain (destruction scheme) and provide financial support for the culling of those animals at the end of productive life. The final surveillance strategy would be reduced to the examination of the clinical suspect animals (if there are any) and maintenance surveillance strategy in line with the OIE recommendations.
Special Risk Material: If BSE cases are not detected below a certain age or drop below an agreed prevalence, the obligation to remove the specified risk material minimal list of SRM particularly, nervous tissues of cattle of certain age groups, may be considered as a precautionary measure against future epidemics or sporadic cases.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download