Abstract
Diagnosis of an adrenal tumor without typical clinical signs related to hyperadrenocorticism and elevated alkaline phosphatase is challenging. This report describes a sex hormone-secreting adrenal tumor in a 10-year-old castrated male Shih Tzu evaluated through repetitive ultrasonographic examination. An adrenocorticotropic hormone stimulation test revealed elevated concentrations of androstenedione and 17-hydroxyprogesterone but a normal cortisol concentration. A mass was surgically excised and adenoma was diagnosed histopathologically. In the present case, adrenal tumor was strongly suspected based on a gradual increase in adrenal size and a change from peanut shape to an irregular mass on repetitive ultrasonography. Repetitive ultrasonographic examination of the adrenal gland is recommended when an abnormal ultrasonographic appearance of adrenal gland is identified, even in an asymptomatic dog.
Adrenal tumors are classified as functional or non-functional. Functional adrenocortical tumors generally produce cortisol, rarely aldosterone or sex hormones, while medullary tumors produce catecholamines [369]. Non-functional adrenal tumors are not uncommon, and 57% of pheochromocytomas have been reported as non-functional [12]. Clinical signs related to an adrenal tumor depend on the hormones secreted. The majority of adrenocortical tumors secreting cortisol induce clinical signs related with hyperadrenocorticism, including polyphagia, polydipsia, polyuria, abdominal distension, and bilateral alopecia [5]. Sex hormones, particularly 17-hydroxyprogesterone, are suspected as the cause of atypical Cushing's syndrome [5]. In veterinary medicine, four dogs with sex hormone-producing adrenal tumors have been reported, and they showed typical clinical signs related to hyperadrenocorticism [1013]. This report describes the case of a dog with a sex hormone-secreting adrenocortical adenoma that was unaccompanied by clinical signs of hyperadrenocorticism.
A 10-year-old castrated male Shih Tzu was presented for a general health check. No abnormal findings were detected on complete blood count, serum chemistry, and electrolytes. Abdominal radiographs showed a normal liver size (panel A in Fig. 1). The width of left adrenal gland was 6 mm while that on the right side was 6.3 mm and had a peanut shape on ultrasonography (panel A in Fig. 2). Two months later, the right adrenal gland was markedly enlarged (width 10.8 mm) and showed a mixed echo texture but without change of the peanut shape on ultrasonography (panel B in Fig. 2). There were no abnormal changes in clinical condition, serum chemistry, or radiographs. Basal (3.9 µg/dL; reference range, 2.0–6.0 µg/dL) and post-adrenocorticotropic hormone (ACTH) stimulation test cortisol concentrations (16.4 µg/dL; reference range, 6.0–18.0 µg/dL) were within the normal ranges. The results of a low-dose dexamethasone suppression test (LDDST) were 0.7 µg/dL at 4 h and < 0.5 µg/dL at 8 h (reference range, < 1 µg/dL). Cortisol-secreting hyperadrenocorticism was ruled out.
In spite of the asymptomatic condition, about 20 months after the initial presentation, hepatomegaly was detected on radiographs (panel B in Fig. 1). The right adrenal gland had changed into a mass-like lesion containing an anechoic cyst. The mass was approximately 20.5 mm × 28.1 mm and had an irregular margin (panel C in Fig. 2). Color Doppler mode imaging showed a definite blood signal within and around the mass, but no evidence of vascular invasion of the mass. No abnormal findings were detected in the left adrenal gland or other organs. A non-functional adrenal gland tumor, aldosterone or sex hormone-secreting tumor, or a pheochromocytoma were included in the differential diagnosis. An ACTH stimulation test (IDEXX Laboratories, USA) was reinstituted to identify the secretion of aldosterone and sex hormones. The basal and post-ACTH test concentrations of androstenedione and 17-hydroxyprogesterone were elevated (Table 1), and a sex hormone-secreting adrenal cortical tumor was tentatively diagnosed.
Computed tomography (CT; Somatom Emotion; Siemens, Germany) was performed to determine the possibility of surgical mass excision based on vascular invasion and metastasis observations. Contrast CT images of the mass were acquired during the arterial (9 sec) and venous phases (28 sec) following injection of 880 mg I/kg iohexol (Omnihexol 300; Korea United Pharm, Korea) at a rate of 3 mL/sec. The hypoattenuating right adrenal mass, about 20 mm × 20 mm in diameter was heterogeneously enhanced after contrast injection (Fig. 3). The mass was located near the caudal vena cava but did not invade the vessel. No other abnormal findings or metastatic lesions were detected.
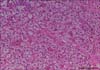
On laparotomy, the right adrenal gland appeared as a reddish mass with a relatively smooth contour and had a definite margin without adhesion to adjacent organs or vascular invasion. Histopathologic examination of the adrenal mass revealed tumor cells containing a large cytoplasm with many lipid droplets and small, one-to-several hyperchromatic nuclei. Some scattered tumor cells showed large eosinophilic cytoplasm and polyhedral nuclei, which compressed the glomerulosa and fasciculata zonae, and adrenal medulla, resulting in small remnants of those layers. Within and around the tumor lesion, anastomosis and neovascularization had developed in areas where tumor cells had invaded and lined capillary walls. On the basis of these findings, the mass was confirmed to be an adrenocortical adenoma with resulting severe atrophy of the fasciculata and glomerulosa zonae (Fig. 4). The dog was discharged 3 days later.
Adrenal cortical tumors are the cause of hyperadrenocorticism in 10 to 20% of cases [79]. Serum alkaline phosphatase level can be used as a clue for the presence of hyperadrenocorticism because approximately 90% of cases of this disease show an elevated serum alkaline phosphatase level; although hormone testing is essential to diagnose hyperadrenocorticism [5].
The ACTH stimulation test is one of the screening tests suitable for application in cases suspected to have adrenocortical tumor because most such tumors secrete cortisol. However, sensitivity of the ACTH stimulation test is relatively low (60–95%); therefore, hyperadrenocorticism cannot be ruled out based on the results of the ACTH stimulation test [510]. In cortisol-producing adrenocortical tumors, serum cortisol concentrations at 4 or 8 h of the LDDST are maintained within the normal range with no suppression [4]. The cortisol concentrations, in this case, were normal on the ACTH stimulation test but were markedly suppressed at 4 and 8 h of the LDDST. These endocrine examination results were far from the changes typically identified in a cortisol-producing adrenocortical tumor. Thus, secretion of other hormones such as aldosterone and sex hormones was suspected. Sex hormone-secreting adrenal tumors produce atypical Cushing's syndrome [5]. The four previously reported dogs with sex hormone-producing adrenal tumors showed normal results on the cortisol-related hormone tests but showed typical clinical signs such as polyuria, polydipsia, polyphagia, and elevated alkaline phosphatase, which are indicative of hyperadrenocorticism [1013]. All previous cases were determined to be adenocarcinomas. The present case had an adrenocortical adenoma producing androstenedione and 17-hydroxyprogesterone. In this case, it was a challenge to diagnose the adrenal tumor due to the lack of clinical signs that are typically related to hyperadrenocorticism.
In this case, ultrasonography provided important clues about the adrenal tumor by revealing morphological changes such as adrenal shape and size. The normal adrenal gland has a peanut shape and a width less than 6 mm in small breed dogs [1211]. In cases of adrenal enlargement, based on width, adrenal tumors and pituitary-dependent hyperadrenocorticism (PDH) can be considered. However, PDH tends to show bilateral adrenal enlargement with maintenance of the peanut shape [7]. An adrenal tumor usually has a unilateral adrenal mass, and, if producing cortisol, it can lead to atrophy of the opposite side adrenal gland. In the present case, the size of right adrenal gland progressively increased and the shape changed into a mass. Even though the dog did not exhibit abnormal clinical signs, the ultrasonographic changes in adrenal size and shape were strongly indicative of an adrenal pathology. The other side adrenal gland maintained its normal size and shape in the present dog. Our ultrasonographic findings were compatible with the previous two cases of sex hormone-producing adrenocortical tumors [13].
The histological type of an adrenal tumor cannot be assured from ultrasonographic findings, and histopathologic examination of the biopsied or surgically excised adrenal gland is needed to diagnose an adrenal tumor. In addition to such examination, vascular invasion and metastasis should be carefully evaluated because invasion into adjacent vessels can be a decisive factor when evaluating malignancy, as well it is a major determinant for removing an adrenal mass surgically and is useful in predicting a patient's prognosis [1911]. Ultrasonography can effectively show vascular invasion by an adrenal tumor, and it is reported to have 100% sensitivity and 96% specificity for detecting a thrombus in the caudal vena cava [3]. However, in cases of vascular invasion not accompanied by a thrombus, sensitivity and specificity of ultrasonography (76% and 96%, respectively) are lower than those for CT (92% sensitivity and 100% specificity) [311]. Vascular invasion or thrombus were not detected solely through ultrasonography in this case; CT was also used. Metastasis to lung and liver, common metastatic sites of adrenal tumors [89], was ruled out through radiography, ultrasonography, and CT before surgical planning. Surgical excision of the adrenal tumor was performed due to the case's prognosis.
The present report describes ultrasonography and CT features of a sex hormone-producing adrenocortical adenoma. This case is the first report of a sex hormone-secreting adrenal adenoma that did not induce clinical signs. Adrenal tumor was strongly suspected based on the gradual increase in adrenal size and the change from a peanut shape to a mass on repetitive ultrasonography. During planning for surgical excision, CT played an important role in excluding vascular invasion and metastasis. Repetitive ultrasonographic examination of the adrenal gland is recommended when an abnormal ultrasonographic appearance of the adrenal gland is observed, even in an asymptomatic dog.
Figures and Tables
Fig. 1
Right lateral abdominal radiographs of the dog at first presentation (A) and approximately 20 months later (B). Note the increased liver size in (B) compared with that in (A). Liver size was determined based on the gastric axis (white line).

Fig. 2
Serial ultrasonography of the right adrenal gland at the first presentation (A), at 2 months (B), and approximately 20 months later (C). The size of the right adrenal gland (arrow) had increased and had changed to form a mass-like lesion with heterogeneous echotexture (*) and an irregular margin.

Fig. 3
Transverse image (A) and multiplanar reconstructed oblique sagittal plane image (B) from post-contrast abdominal computed tomography. Right adrenal mass was close to the wall of the caudal vena cava but did not invade it. Ao, aorta; RK, right kidney; CVC, caudal vena cava; M, mass.

Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (2015R1A2A2A01003313), Republic of Korea.
References
1. Besso JG, Penninck DG, Gliatto JM. Retrospective ultrasonographic evaluation of adrenal lesions in 26 dogs. Vet Radiol Ultrasound. 1997; 38:448–455.

2. Choi J, Kim H, Yoon J. Ultrasonographic adrenal gland measurements in clinically normal small breed dogs and comparison with pituitary-dependent hyperadrenocorticism. J Vet Med Sci. 2011; 73:985–989.

3. Davis MK, Schochet RA, Wrigley R. Ultrasonographic identification of vascular invasion by adrenal tumors in dogs. Vet Radiol Ultrasound. 2012; 53:442–445.

4. Feldman EC, Nelson RW, Feldman MS. Use of low- and high-dose dexamethasone tests for distinguishing pituitary-dependent from adrenal tumor hyperadrenocorticism in dogs. J Am Vet Med Assoc. 1996; 209:772–775.
5. Gilor C, Graves TK. Interpretation of laboratory tests for canine Cushing's syndrome. Top Companion Anim Med. 2011; 26:98–108.

6. Gójska-Zygner O, Lechowski R, Zygner W. Functioning unilateral adrenocortical carcinoma in a dog. Can Vet J. 2012; 53:623–625.
7. Grooters AM, Biller DS, Theisen SK, Miyabayashi T. Ultrasonographic characteristics of the adrenal glands in dogs with pituitary-dependent hyperadrenocorticism: comparison with normal dogs. J Vet Intern Med. 1996; 10:110–115.

8. Kyles AE, Feldman EC, De Cock HEV, Kass PH, Mathews KG, Hardie EM, Nelson RW, Ilkiw JE, Gregory CR. Surgical management of adrenal gland tumors with and without associated tumor thrombi in dogs: 40 cases (1994-2001). J Am Vet Med Assoc. 2003; 223:654–662.

9. Massari F, Nicoli S, Romanelli G, Buracco P, Zini E. Adrenalectomy in dogs with adrenal gland tumors: 52 cases (2002-2008). J Am Vet Med Assoc. 2011; 239:216–221.

10. Norman EJ, Thompson H, Mooney CT. Dynamic adrenal function testing in eight dogs with hyperadrenocorticism associated with adrenocortical neoplasia. Vet Rec. 1999; 144:551–554.

11. Schultz RM, Wisner ER, Johnson EG, MacLeod JS. Contrast-enhanced computed tomography as a preoperative indicator of vascular invasion from adrenal masses in dogs. Vet Radiol Ultrasound. 2009; 50:625–629.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download