Abstract
This study was conducted to evaluate new acupuncture protocols for the clinical treatment of cervical spinal cord diseases in 19 dogs. Three treatment options containing Jing-jiaji (cervical jiaji) were developed to treat neck pain, hemiparesis, and tetraparesis depending on the severity. The interval between the neurological disease onset and treatment (duration of signs), time to improvement after treatment, and recovery time were compared in dogs by body weight, age, and dry needle acupuncture (AP) with or without electro-AP (EAP). The duration of signs was longer in dogs weighing greater than 10 kg than in those weighing less than 10 kg (p < 0.05). Improvement and recovery times did not vary by body weight. Additionally, improvement and recovery times did not vary by age. The improvement and recovery times were longer in the AP+EAP group than the AP group (p < 0.05). Acupuncture with Jing-jiaji was effective in cervical spinal cord diseases in different sized dogs and in middle-aged and senior dogs. This report standardized AP treatment containing Jing-jiaji for canine cervical problems and evaluated its effects. The newly standardized AP methodology offers clinical practitioners an effective way to improve the outcomes of cervical neurological diseases in dogs.
Cervical spinal cord diseases are common neurological disorders in dogs. The severity of these disorders can be graded into five levels based upon the following clinical signs: grade 1, neck pain; grade 2, ambulatory tetraparesis (or hemiparesis); grade 3, non-ambulatory tetraparesis (or hemiparesis); grade 4, tetraplegia; and grade 5, tetraplegia without deep pain [3]. Treatments are usually divided into two categories: conservative therapies and surgical treatments. Conservative therapies are noninvasive and include medication, rehabilitation, and confinement. Surgical treatments such as decompression and fixation are considered invasive. The choice of treatment depends on the severity of the disease, condition of the dog, and economic considerations. Certain dogs need surgery, whereas some owners choose to try noninvasive therapy such as acupuncture (AP) [412].
Acupuncture is a less-invasive method for the treatment of cervical spinal disorders. However, there is no standard protocol and the underlying Chinese medical theories about the existence of meridians, Qi deficiency, and Qi stagnation, which are most commonly encountered in cervical spinal deficiency, have yet to be confirmed scientifically. The AP protocol utilized depends on the diagnosis according to traditional Chinese veterinary medicine (TCVM) and veterinarians' experiences [89]. There are many commonly used AP points (acupoints) for cervical spinal disorders, including local points (acupoints around the lesion) and distant points (acupoints distal to the lesion).
In this study, a new AP protocol was applied to localized cervical problems. We sought to simplify the points and standardize the protocol for treating different levels of cervical neurological deficits. The specific purpose of this study was to evaluate the effects of new AP protocols for the treatment of cervical spinal cord diseases in 19 dogs.
Clinical neurology case records were retrospectively collected from the University Veterinary Hospital for 2009 to 2014. Lesions in all 19 dogs were localized to the cervical spinal cord, resulting in neck pain. The dogs had histories of neck stiffness, screaming, or poor cervical range of motion. However, they continued to suffer hemiparesis or tetraparesis. Dogs presented with ataxic gait affecting four limbs or non-weight bearing paresis in ipsilateral limbs or all four limbs. They had been treated with medication, cage confinement, or surgery without improvement. All of the dogs were X-rayed to rule out structural dislocations. Additionally, four dogs underwent MRI (Vet-MR 0.2 Tesla; Esaote, Italy), and one underwent MRI and CT (Activion 16; Toshiba, Japan). The dogs were referred for at least four TCVM treatments consisting of AP or AP combined with Chinese herbal medicines. No other medication related to pain or paresis was prescribed during TCVM treatment.
The selected acupoints were divided into local points and distant points. Local points involved Jing-jiaji (JJJ, cervical jiaji) points. Distant points included LI4 (He Gu), SI3 (Hou Xi), LIV3 (Tai Chong), BL11 (Da Zhu), and TH5 (Wai Guan) (Table 1, Fig. 1).
The local points were stimulated using stainless steel needles (0.3 mm in diameter, 25 mm in length; Yu Guang, Taiwan) with a perpendicular insertion depth of 0.5–1.0 cm. Distant points were stimulated using stainless steel needles (0.27 mm in diameter, 13 mm in length; Yu Guang) with a perpendicular insertion depth of 0.25–0.50 cm.
The choice of acupoints and method used depended on the grade of severity, onset period, and weakness of limbs. The grading of severity was recorded as described previously [3]. Briefly, grade 1 comprised neck pain/stiffness and no other deficit, grade 2 included ambulatory tetraparesis (or hemiparesis) and grade 3 was non-ambulatory tetraparesis (or hemiparesis). Treatment option 1 was used in dogs presenting with any grade of severity. Treatment option 2 was used in dogs presenting with chronic, long-term signs lasting longer than 2 weeks. Treatment option 3 was used for dogs exhibiting weak thoracic limbs. There were no grade 4 or 5 cases in this study. Treatment option 1, dry needling in local points C1-C3-C5 (JJJ) and in distant points SI3, LIV3 and LI4; Treatment option 2, option 1 with EAP in local points JJJ; and Treatment option 3, option 2 with EAP in distant points BL11+TH5 (BL11 to TH5 connected).
With the dry needle method, needles were inserted and remained in place for 15 min. With EAP, the procedure was identical to that of AP, except that electrical stimulation was applied to the needle while inserted. An electrostimulator (Ching Ming TENS Model-05B; Ching Ming, Taiwan) was used to provide stimulation for 15 min at 0.2 Vp-p (voltage peak to peak) with a frequency of 20 Hz (interrupted wave type). The intensity of electrostimulation was adjusted according to the dog's response to avoid discomfort. EAP points included two pairs of points, a bilateral JJJ and BL11 (Da Zhu) and TH5 (Wai Guan). The AP treatment was performed two times per week initially, then once per week after significant improvement was achieved.
Chinese herbs, which consisted of Double PII (Jing Tang, USA; the classical antecedent was Da Huo Luo Dan) and Cervical Formula (Jing Tang; no classical antecedent) (Table 2), were given to 15 of 19 dogs. The dosage was 1 g per 5 to 10 kg of body weight, which was administered orally twice daily until recovery. In four cases, Chinese herbs were not prescribed. Specifically, one dog had a hypersensitivity to the Chinese herbs (case 11) and three dog owners were reluctant to apply Chinese herbal treatments (cases 3, 13 and 17).
Dogs treated less than four times (at the owner's discretion) without any improvement were excluded from the analysis. The duration of signs prior to TCVM treatment (defined as the time period from disease onset TCVM treatment start) was recorded. After TCVM treatment, improvement time (defined as the time needed to walk without assistance in paretic cases or pain alleviating in neck pain cases) and recovery time (defined as the time required to return to normal daily life or absence of pain in neck pain cases) were recorded [7].
SPSS (ver. 18.0; SPSS, USA) was used to analyze the data. Statistical differences were considered significant at p < 0.05.
Nineteen dogs were identified with cervical spinal signs and symptoms. Signalment, lesion location, examination, diagnosis, severity, treatment methods, and time courses were retrieved from the medical records (Table 3). The improvement in grade 1 cases (neck pain) progressed from improved neck stiffness and screaming to increased range of neck motion and increased activity, such as wagging tail freely, reduced pain medication or free from pain medication, to willingness to play (no pain). In grade 2 cases (ambulatory tetraparesis), the improve process went from gait ataxia to a well-coordinated gait. In grade 3 cases (non-ambulatory tetraparesis), the improvement proceeded from increased activity, lateral recumbence to sternal positioning, trying to stand, ataxic gait, small strides, and walking well to a little running.
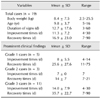
The mean body weight was 8.4 kg (range, 2.5–25.5) and the average age was 9.8 years (range, 5–16). The mean duration of signs before TCVM integration was 12.7 ± 17.6 days (range, 3–60), the mean improvement time was 11.3 ± 7.2 days (range, 4–30) and the mean recovery time was 16.9 ± 23.0 days (range, 7–90).
The clinical findings included neck pain/stiffness in five dogs, ambulatory tetraparesis in three dogs, non-ambulatory tetraparesis in nine dogs, and non-ambulatory hemiparesis in two dogs. In grade 1 cases (n = 5), the mean improvement time was 8 days (range, 4–14), while the mean recovery time was 25.6 days (range, 11–75). In grade 2 cases (n = 3), the average improvement time was 7 days, and the average recovery time was 14 days (range, 7–14). In grade 3 (including tetraparesis and hemiparesis) cases (n = 11), the mean improvement time was 14 days (range, 4–30) and the mean recovery time was 35.7 days (range, 7–90) (Table 4). All dogs in this group recovered and walked without assistance.
Because the data were not normally distributed, they were analyzed using the Kruskal-Wallis test. The duration of signs to TCVM integration was significantly longer (p < 0.05) in dogs weighing greater than 10 kg (n = 5) than in those weighing less than 10 kg (n = 14). There was no difference in improvement time or recovery time based on body weight. Age [≥ 10 years (n = 9) or < 10 years (n = 10)] had no significant effect on the duration of signs, improvement, or recovery times. The two treatment methods, EAP plus AP (n = 8) and AP only (n = 11), did not differ significantly in the duration of signs. However, the improvement and recovery times were significantly longer in the AP+EAP group (p < 0.05). The effects of treatments with AP or AP+EAP were compared by severity in Table 5. The three different severity grades had similar improvement times following AP treatment, while for the duration of signs, grade 1 > grade 2 > grade 3. The recovery times of grade 3 dogs were longer than for grade 1 and grade 2 dogs. With AP+EAP treatment, improvement time for grade 1 dogs was similar to that of grade 3, but the recovery times were far longer than for grade 3 dogs, while the duration of signs was longer than for grade 3 dogs. Dogs in group 3 receiving AP + EAP had similar durations of signs and improvement times. However, the recovery times were longer in the dogs receiving option 3 treatment.
Among the 19 dogs, the duration of signs, improvement time, and recovery time did not differ between groups receiving AP with Chinese herbs (n = 15) and AP without Chinese herbs (n = 4). Additionally, there was no significant difference between 2 groups with respect to neurological localization at C1–C5 (n = 12) and C6–T2 (n = 7) or for the final diagnosis IVDD (intervertebral disc disease) (n = 11) and IVDD with spondylosis deformans (n = 7). Table 6 compares different variables related to treatment progress. The duration of signs, improvement times, and recovery times in the C1–C5 localization group were longer than in the C6–T2 group and in the IVDD group than in the IVDD+spondylosis deformans group.
There is much less literature available pertaining to TCVM treatment for cervical spinal cord diseases in dogs than there is for traditional Chinese medical treatment of human cervical spinal cord disease. In humans, JJJ points are used in AP for neck pain and cervical spinal cord compression [1422]. The locations of JJJ points differ for humans and dogs [519]. We found no literature on JJJ points used as local acupoints for the treatment of cervical spinal cord diseases in dogs. Based on our experience, the TCVM treatment protocol and AP point selection depended on each individual case. In this study, we sought to standardize protocols as simply as possible for the cervical spinal cases we treated.
In traditional Chinese medicine, stimulation of JJJ points harmonizes the GV (governing vessel) and BL (bladder) channels [21]. In anatomy, stimulation of JJJ points triggers a reflex arc, resulting in sympathetically induced, segmental, superficial, and visceral vasodilation [111]. Another important effect of local point stimulation is that it activates local immune-inflammatory systems [10]. The stimulation site also releases bradykinin, and thus, increases local vascular permeability to allow other inflammatory mediators access to the area. Because of the high concentration of nerve endings and dense microvasculature around the acupoints, these effects are greater than the effects of local stimulation on stimulation sites [15].
In dogs, superficial needling may not attain the best point identification, and the JJJ points are very near the cervical spinal cord. It is easy to palpate the lateral transverse processes and insert the needles into JJJ points. Given that there is a needling sensation, changes in needle depth at the JJJ points do not make cause obvious differences in the therapeutic efficacy during treatment of certain cervical spinal problems [2]. This is why we chose the JJJ as local points.
In anatomy, the purpose of stimulation to SI3, LI4, and LIV3 is to stimulate the distal extremities to arouse conscious proprioception. Stimulation through the afferent nerves enters the spinal cord and passes up to the brain, after which it travels via the efferent nerves down to the extremities to re-educate the nerves and facilitate their healing [1318]. Concurrent stimulation of BL11+TH5 strengthens weak thoracic limbs. For one of the dogs with grade 1 disease, option 2 was chosen and successfully relieved pain. Although the dog had grade 1 severity in terms of neurology, neck pain is sometimes not well tolerated by dogs over the long term. For this dog, application of AP+EAP was considered.
There were large variances in mean improvement and recovery times. The variance could be related to the individual conditions of the dogs, their healing abilities, and their individual responses to AP. We did not track specific dog breeds.
In humans, JJJ points are used for neck pain [14]. For dogs, we found that JJJ points were also beneficial for the treatment of tetraparetic dogs. From a clinical point of view, the prominent improvements were pain relief and recovery of ambulation. Two treatments were necessary for neck pain relief and four treatments (twice a week) were needed for improvement in ambulation.
Among the larger, heavier dogs (n = 5), two had delays in starting TCVM (cases 12 and 13). These dogs were treated for neck pain at a local animal hospital for two months before being referred for TCVM because of their poor responses to treatment and the side effects of the analgesics. Since there were no differences in improvement and recovery times, the AP protocol had the same impact on both lighter, smaller dogs (2.5-9.0 kg) and heavier, larger dogs (14.0-25.5 kg).
Because there were no differences in duration of signs, improvement times, and recovery times between the two age groups of dogs, the AP protocol had the same effects on both younger dogs (5-9 years) and older dogs (10-16 years).
In addition to duration of signs, the severity of the disease was also taken into account when considering whether to add EAP to the protocol. In anatomy, the purpose of EAP stimulation connecting BL11 to TH5 is to enforce the stimulation of AP to the thoracic limbs. In this study, 20 Hz (interrupted wave) was applied for 15 min. An in vivo study in cats revealed that peripheral stimulation at 20 Hz maximized the release of substance P [6]. Substance P, which acts via neurokinin-1 receptors, promotes the proliferation of neural cells and is associated with the regulation of neurogenesis [16]. The improvement and recovery times were both longer when electrical stimulation was done. One possible reason is that there were more dogs with grade 3 severity in the AP+EAP group. In the AP group, dogs with different severity grades had similar improvement times, but the recovery times were longer in dogs with grade 3 severity than in those with lesser severity grades. Thus, with AP treatment, dogs with severe grade 3 disease needed a longer time to heal (recover) even though the duration of signs was short. In the same grade 3 group, AP treatment resulted in shorter improvement and recovery times than AP+EAP treatment, probably because of the shorter duration of signs. These findings indicate that a delay in treatment at this severity grade, even when receiving AP+EAP, resulted in a longer time being required to heal. Dogs in the same grade 3 group receiving AP+EAP had a similar duration of signs and improvement times, but the recovery times were longer in dogs with weak thoracic limbs. Thus, dogs with grade 3 and thoracic limb weakness needed more time to heal.
Only one dog with grade 1 severity received AP+EAP because of the long duration of signs. Its improvement time was similar to that of dogs with grade 3 severity, but its recovery time was longer than that of dogs with grade 3 severity receiving AP+EAP. These findings indicate that even though the severity grade was low, once the duration of signs was long, it affected the prognosis. Another possibility is that adding EAP benefits neurogenesis (good for grade 3). AP alone benefits analgesia (good for grade 1). Further study with more cases is necessary to verify these assumptions. In this study, no dogs with grade 2 received AP+EAP because of the acceptable effects produced by AP. We anticipate that dogs with grade 2 severity (ambulatory tetraparesis), a certain duration of signs and without thoracic limb weakness will have a good prognosis upon AP+EAP treatment. Further study is required to determine whether or not dogs with long-term (more than 2 weeks) or only short-term (less than 1 week) grade 2 severity should be treated with AP+EAP for a better neurological response.
Dogs with IVDD+spondylosis deformans had shorter improvement and recovery times than those with IVDD alone. One possible reason is a shorter duration of signs before treatment in IVDD+spondylosis deformans dogs. Therefore, a shorter onset of disease was associated with a better outcome, even when two disorders presented together. Similarly, dogs with more severe C6–T2 lesions had shorter improvement and recovery times than those with C1–C5 because of the shorter onset of disease before treatment.
According to TCVM, the mechanism underlying AP eliminates stagnation of Qi or blood. When stagnation resolves, Qi flows freely; thus, pain ends and the function resumes. In this study, two Chinese herb formulas were prescribed to improve the flow of Qi, Double PII (Jing Tang) and Cervical Formula (Jing Tang). The treatment principles of Double PII are to break down stasis in the spine, move Qi, and relieve pain. The Cervical Formula is a cervical transporter, blood activator, and Qi mover that dissipates stagnation and relieves neck pain [20]. Although there was no obvious statistical difference between AP treatment combined with Chinese herbs or without in this study, we anticipate that improvement and recovery times would be shorter when treatment included Chinese herbs (Table 6); however a larger study should be conducted to confirm this.
All 19 dog owners were asked to bring their dogs to the veterinary clinic for reexamination to check their conditions every few weeks or months. All of the dogs were successfully treated using this AP protocol with no relapse as of completion of the study and subsequently over a period ranging from 1.5 years (case 19) to 5 years (case 12). We do not recommend this AP protocol in cases of significant structural change, such as ruptured nerves, severe cervical vertebral dislocation, or cervical spinal cord compression due to a tumor because such cases usually have poor prognosis, even after aggressive treatment such as surgery.
In the case of tetraparesis, other factors related to improvement and recovery include rehabilitation and care. In the early stages of the treatment, encouragement to stand and walk with assistance (such as walking with a sling or cart) is crucial to educate the nerves and train the muscles. When dogs exhibit marked improvement, vigorous physical rehabilitation by underwater treadmill training or sling assisted walking is highly recommended to help increase muscle strength [17]. In this study, dogs with body weight over 10 kg received underwater treadmill rehabilitation (cases 1, 11 and 19), while those with body weight under 10 kg underwent sling aided walking (cases 2, 5, 6, 7, 9, 15, 17 and 18).
There are many methods to treat cervical spinal diseases resulting in neck pain or tetraparesis in dogs, including TCVM. Among the 19 successfully treated dogs in this study, the new standardized AP protocol led to a marked improvement after only four sessions of twice weekly treatment. The dog with fibrocartilaginous embolism needed at least two sessions for improvement and six sessions to recover. Additionally, dogs with IVDD needed at least four sessions to improve and seven sessions to recover, while those with IVDD and spondylosis deformans required three sessions to improve and five sessions to recover.
We objectively evaluated the effects of AP from the functional clinical perspective; however, more studies with greater numbers of subjects are needed to confirm our results and document the bio-molecular changes and mechanisms of treatment.
Figures and Tables
 | Fig. 1Locations of acupoints used for cervical spinal cord diseases in dogs. JJJ (Jing-jiaji) acupoints are located bilaterally on the neck. LI4 (He Gu) acupoints are located on dorsal fore paws. SI3 (Hou Xi) acupoints are positioned on lateral fore paws. LIV3 (Tai Chong) acupoints are situated on dorsal hind paws. BL11 (Da Zhu) acupoints are found on the front back area, and TH5 (Wai Guan) acupoints are located on the forearms. |
Table 1
Location and indication of acupoints used for cervical spinal cord diseases

*The width of the last rib is equal to 1 cun in small animals [19].
Table 3
Signalment, lesion location, examination, diagnosis, severity, treatment methods and different time courses in 19 dogs

Acknowledgments
The authors thank the National Taiwan University Statistical Education Center for statistical aid.
References
1. Cabioglu MT, Arslan G. Neurophysiologic basis of Back-Shu and Huatuo-Jiaji points. Am J Chin Med. 2008; 36:473–479.

2. Cheng W, Chen J, Guo B. Effect of different needling depths on the therapeutic efficacy of acupuncture at cervical Jiaji points (Ex-B 2) for cervical spondylosis. Shanghai J Acupunct Moxib. 2013; 32:36–37.
3. Chrisman CL. Spinal cord disorders. In : Xie H, Chrisman C, Trevisanello L, editors. Traditional Chinese Veterinary Medicine for Neurological Diseases. Proceedings of the 13th Annual International TCVM Conference. Reddick: Jing Tang Publishing;2011. p. 225–322.
4. Chrisman CL. Treatment of neurological disorders with traditional Chinese veterinary medicine. In : Platt SR, Olby NJ, editors. BSAVA Manual of Canine and Feline Neurology. 4th ed. Gloucester: British Small Animal Veterinary Association;2013. p. 496–507.
5. Deadman P, Al-khafaji M, Baker K. The extra points. A Manual of Acupuncture. 2nd ed. Hove: Journal of Chinese Medicine Publications;2007. p. 574–575.
7. Hillman RB, Kengeri SS, Waters DJ. Reevaluation of predictive factors for complete recovery in dogs with nonambulatory tetraparesis secondary to cervical disk herniation. J Am Anim Hosp Assoc. 2009; 45:155–163.

8. Janssens LAA. The treatment of canine cervical disc disease by acupuncture: a review of thirty-two cases. J Small Anim Pract. 1985; 26:203–212.

9. Janssens LAA. Acupuncture for the treatment of thoracolumbar and cervical disc disease in the dog. Probl Vet Med. 1992; 4:107–116.
10. Kendall DE. Part I: a scientific model of acupuncture. Am J Acupunct. 1989; 17:251–268.
11. Kendall DE. Part II: a scientific model of acupuncture. Am J Acupunct. 1989; 17:343–360.
12. Kline KL. Complementary and alternative medicine for neurologic disorders. Clin Tech Small Anim Pract. 2002; 17:25–33.

13. Leung L. Neurophysiological basis of acupuncture-induced analgesia—an updated review. J Acupunct Meridian Stud. 2012; 5:261–270.

14. Liu Y, Hu J, Zhang H, Huang G, Zhou L. Clinical study on analgesic effect of acupoint injection at cervical jiaji points for the treatment of cervical spondylosis of nerve root type. Chin J Tradit Med Traumatol Orthop. 2009; 17:28–29.
15. Omura Y. Patho-physiology of acupuncture treatment: effects of acupuncture on cardiovascular and nervous systems. Acupunct Electrother Res. 1975; 1:51–140.
16. Park SW, Yan YP, Satriotomo I, Vemuganti R, Dempsey RJ. Substance P is a promoter of adult neural progenitor cell proliferation under normal and ischemic conditions. J Neurosurg. 2007; 107:593–599.

17. Sherman J, Olby NJ, Halling KB. Rehabilitation of the neurological patient. In : Platt SR, Olby NJ, editors. BSAVA Manual of Canine and Feline Neurology. 4th ed. Gloucester: British Small Animal Veterinary Association;2013. p. 481–495.
18. Smith FW Jr. Neurophysiologic basis of acupuncture. Probl Vet Med. 1992; 4:34–52.
19. Xie H, Preast V. Xie's Veterinary Acupuncture. Ames: Wiley-Blackwell;2007.
20. Xie H, Frank LR, Preast V, Trevisanello L. Chinese Veterinary Herbal Handbook. 3rd ed. Reddick: Jing Tang Publishing;2011.
21. Zhang LY, Zhao GJ. Research and application of Huatuo-Jiaji points. Chin Acupunct Moxib. 1998; 18:695–697.
22. Zhang Y, Wang C, Guo Y. The progress of clinical research on cervical spondylosis treated with acupoint injection in recent five years. Chin Acupunct Moxib. 2012; 32:477–479.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download