Abstract
Limited information is available regarding horse-associated antimicrobial resistant (AR) Escherichia (E.) coli. This study was designed to evaluate the frequency and characterize the pattern of AR E. coli from healthy horse-associated samples. A total of 143 E. coli (4.6%) were isolated from 3,078 samples collected from three national racetracks and 14 private horse-riding courses in Korea. Thirty of the E. coli isolates (21%) showed antimicrobial resistance to at least one antimicrobial agent, and four of the AR E. coli (13.3%) were defined as multi-drug resistance. Most of the AR E. coli harbored AR genes corresponding to their antimicrobial resistance phenotypes. Four of the AR E. coli carried class 1 integrase gene (intI1), a gene associated with multi-drug resistance. Pulsed-field gel electrophoretic analysis showed no genetic relatedness among AR E. coli isolated from different facilities; however, cross-transmissions between horses or horses and environments were detected in two facilities. Although cross-transmission of AR E. coli in horses and their environments was generally low, our study suggests a risk of transmission of AR bacteria between horses and humans. Further studies are needed to evaluate the risk of possible transmission of horse-associated AR bacteria to human communities through horse riders and horse-care workers.
Escherichia (E.) coli is a predominant facultative anaerobe that is a Gram-negative commensal microorganism present in the gastrointestinal microflora of humans and animals. Most E. coli strains are non-pathogenic, and some strains play important roles as constituents of microflora in the intestinal tracts of healthy animals. However, pathogenic E. coli, such as enteropathogenic E. coli (EPEC), enterotoxigenic E. coli (ETEC), enteroinvasive E. coli (EIEC), enteroaggregative E. coli (EAEC) and diffuse adhering E. coli (DAEC), cause diseases of the gastrointestinal, urinary or central nervous system in humans [19]. These illnesses are sometimes associated with food poisoning caused by ingestion of contaminated food.
Resistance to antimicrobials in bacterial strains is considered as a serious threat to public health, particularly in developing countries. In the past two decades, the frequency of isolation of antimicrobial resistant (AR) bacteria, including those resistant to fluoroquinolones and cephalosporins, has increased [17]. E. coli is sometimes used as a sentinel strain for monitoring antimicrobial resistance in fecal bacteria because it is most commonly cultured from a wide range of hosts [9] and easily acquires antimicrobial resistance through genetic mutation or horizontal gene transfer via certain mobile genetic elements, such as transposons, bacteriophages and plasmids [4]. Additionally, many dfr genes responsible for trimethoprim (TMP) resistance have been found in gene cassettes inserted in integrons [33]. Since many gene cassettes of integrons possess diverse antimicrobial resistance genes in Gram-negative bacteria, such as E. coli, horizontal gene transfer by integrons causes the emergence of multi-drug resistant (MDR) bacteria [23].
The prevalence and distribution of AR E. coli from food and pet animals have been studied extensively, and the transmission of AR E. coli between animals and humans has been demonstrated [2526]. However, unlike other animals, much less attention has been given to the prevalence and possible cross-transmission of AR E. coli associated with horses. According to a report by the Korean Racing Association (KRA), the size of the horseback-riding industry is rapidly increasing annually and the estimated number of horse riders was about 420,000 in 2013 Korea [14]. This may suggest an increased chance of transmission of zoonotic pathogens originating from horses to humans due to the increased contacts with horses. Thus, it is important to evaluate this risk owing to the potential public health threat.
In the present study, horse-associated E. coli were isolated and identified from samples acquired from horses and their environments in national racetracks and private horse-riding courses in Korea during 2013. The frequency of AR E. coli and their AR profiles and molecular fingerprints were determined to evaluate their distribution and clonalities in horses and horse-associated environments. The current study provides the first data describing the dissemination of AR E. coli in horses in Korea that will be invaluable to estimation of the potential risk of transmission of AR E. coli from horses to humans.
A total of 3,078 swab and specimen cup samples were collected from three national racetracks (Seoul, Busan-Gyeongnam and Jeju race parks) and 14 private horse-riding courses (Gyeonggi-do, n = 6; Chungcheongnam-do, n = 1; Jeollabuk-do, n = 3; Jeollanam-do, n = 2, Gyeongsangbuk-do, n = 2) in Korea from July to October in 2013. Healthy skin (n = 645), nasal cavity (n = 644) and fecal (n = 637) samples were collected from horses, while environmental samples were collected from feed boxes (n = 646), drinking water (n = 495) and bedding (n = 11). Swab methods were used to collect superficial samples (skin and feed box) and nasal cavity samples as follows: (1) healthy skin: a swab was placed on the healthy skin of the horse neck region and swept 3 to 5 times along 15 cm of the surface; (2) feed box: the residual feed was removed and a swab sample was collected from the surface as described above; and (3) nasal cavity: a swab was passed into horse's nostril to a depth of at least 10 cm and rotated to absorb nasal secretions. All swab samples were immediately placed into individual sterile collection tubes containing Amies transport medium (YUHAN LAB TECH, Korea). The rest of the samples (feces, drinking water and bedding) were aseptically collected and placed into sterile specimen cups (Medikorea, Korea). All individual samples were transported to the laboratory on ice within 6 h of collection. On arrival, the samples were immediately processed as described below.
All samples were subjected to the non-selective pre-enrichment step as described below. Briefly, the tip of the swab stick (swab samples: skin, nasal cavity and feed box) or 1 g (or 1 mL) of the specimen cup sample (feces, drinking water and bedding) was put in 10 mL of buffered peptone water (BPW; Becton, Dickinson and Company, USA) and vigorously vortexed. The pre-enrichment medium was incubated at 37℃ for 24 h. After incubation, 1 mL of BPW was transferred into 9 mL of Escherichia coli broth (ECB) and incubated at 37℃ for 24 h for the selective growth of coliforms or E. coli. The culture in the ECB was then streaked onto MacConkey agar (Becton, Dickinson and Company, USA) plates and incubated at 37℃ for 24 h. Putative E. coli colonies were selected according to a standard protocol previously established in our laboratory. For further confirmation, E. coli were identified by strain-specific polymerase chain reaction (PCR) targeting the 16s ribosomal RNA region [29].
Antimicrobial susceptibility was determined by a standard disk diffusion test [31] using the following antimicrobial disks (Becton, Dickinson and Company): ampicillin (AM; 10 µg), amoxicillin/clavulanic acid (AMC; 20/10 µg), ceftazidime (CAZ; 30 µg), cefotetan (CTT; 30 µg), imipenem (IMP; 10 µg), gentamicin (GM; 10 µg), tetracycline (TE; 30 µg), ciprofloxacin (CIP; 5 µg), nalidixic acid (NA; 30 µg), sulfamethoxazole/trimethoprim (SXT; 1.25/23.75 µg), chloramphenicol (C; 30 µg), aztreonam (ATM; 30 µg), ceftriaxone (CRO; 30 µg), cefotaxime (CTX; 30 µg), amikacin (AN; 30 µg) and streptomycin (S; 10 µg). The interpretation of antimicrobial resistance, intermediate resistance or susceptibility was accomplished following the Clinical and Laboratory Standards Institute (CLSI) guidelines [7]. E. coli ATCC 25922 (American Type Culture Collection, USA) was used as a reference strain. The MDR isolates were defined as E. coli isolates resistant to three or more different categories of the evaluated antimicrobials [15].
To confirm the TMP resistance of candidate E. coli isolates, the minimal inhibitory concentrations (MICs) of TMP were determined by the standard agar dilution method according to the guidelines of the CLSI [6]. Isolates with a MIC of 16 µg/mL or higher were considered to be resistant to TMP. E. coli ATCC 25922 was used as a reference strain.
Isolates showing resistance to AM, S, TE and SXT were PCR screened for the presence of the following antimicrobial resistance genes: AM resistance genes (SHV and TEM) [22], S resistance genes (strA-B and aadA) [27], TE resistance genes (tetA and tetB) [20], sulfamethoxazole (SMX) resistance gene (sul1) [30] and TMP resistance genes (dfrA1, A9, A7/17 and A12/13) [1016]. To differentiate dfrA7 and dfrA17 genes, the PCR products of dfrA7/17 genes were digested with Pst1 restriction enzyme before gel electrophoresis. Since the Pst1 restriction site is only present in the dfrA17 gene, the two genes can be easily differentiated by the band pattern of restricted PCR fragments [16].
The integrase genes were amplified using the PCR primers hep35-TGCGGGTYAARGATBTKGATTT and hep36-CARCACATGCGTRTARAT, which were specific for the conserved regions present outside of the integron-encoded integrase genes intI1, intI2 and intI3 [31]. The class of the integrons was determined by restriction analysis of the PCR fragments (restriction fragment length polymorphism). Briefly, the PCR fragments were restricted with HinfI restriction enzyme and the band patterns of restricted fragments were analyzed by gel-electrophoresis. intI1 generates a single band of 491 bp, while intI2 produces two bands of 191 and 300 bp and intI3 generates two bands of 119 and 372 bp, respectively [31].
The type of O-antigen of each isolate was determined by the slide agglutination method as described by Guinee et al. [12] using polyvalent and monovalent antisera (JoongKyeom, Korea). H-antigen typing was conducted by the test tube method using the bacteria cultured in liquid medium with H2, H4, H7, H11, H16, H19, H21 and H51 antisera as previously described [10].
The genetic relatedness among the AR E. coli isolates was determined by standard pulsed-field gel electrophoresis (PFGE) using CHEF MAPPER (Bio-Rad Laboratories, USA) according to the manufacturer's instructions. Briefly, AR E. coli isolates cultured overnight in Tryptic Soy Broth (Becton, Dickinson and Company) were streaked onto Tryptic Soy Agar (Becton, Dickinson and Company) and incubated at 37℃ for 14 to 18 h. The bacterial colonies of each isolate were then suspended in 0.8% saline and adjusted to 4.0 McFarland. Next, suspensions were embedded in 1.0% agarose plugs and lysed with proteinase K (Sigma-Aldrich, USA). The lysed plugs were then digested for 2 h with 50 U of XbaI restriction enzyme (New England Biolabs, USA) at 37℃. Digested plugs were subsequently placed on 1.0% SeaKem Gold agarose (Lonza, USA) and PFGE was carried out at 6.0 V for 19 h with a ramped pulse time of 6.76 to 35.38 sec in 0.5× Tris-Borate-EDTA (TBE) buffer at 14℃. BioNumerics software (Applied Maths, Belgium) was used to establish a DNA similarity matrix using the dice coefficient (0.5% optimization, 1.0% tolerance) and the un-weighted pair group method.
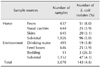
A total of 143 E. coli (4.6%) isolates were obtained from 3,078 horse-associated samples (Table 1). Ninety six isolates (5.0%) were obtained from horses, 51 from fecal samples, 25 from nasal cavity swab samples and 20 from healthy skin swab samples. Additionally, 47 isolates (4.1%) were from facility environments, while 19, 25 and 3 isolates were obtained from drinking water, feed box and bedding samples, respectively (Table 1).
The number of E. coli isolates showing resistance to each antimicrobial is shown in Table 2. Thirty E. coli isolates (21%) were resistant to at least one antimicrobial, while all isolates were susceptible to CAZ, IMP, CIP, NA, C, CRO, CTX and AN. Antibiogram analysis revealed that the frequencies of AR E. coli isolates were 10.5% (15 isolates) and 8.4% (12 isolates) for S and TE, respectively, followed by 6.3% (9 isolates) for SXT. The other 11 isolates resistant to AM, AMC, GM, ATM and CTT accounted for minor portions of the organisms identified in this study. Only four isolates were identified as MDR E. coli, which showed resistance to more than three classes of antimicrobials. The frequencies of antimicrobial resistance to each antimicrobial were higher in E. coli isolated from horses than those from environmental samples, except for AMC (Table 2).
Gene-specific PCR of the AR E. coli isolates from the four most frequently recovered AR phenotypes (AM, S, TE and SXT) was conducted to detect AR genes responsible for their AR phenotypes (Table 3). Among the E. coli isolates resistant to AM, three (60.0%) harbored the TEM gene. The strA-B genes were widely distributed among S-resistant isolates (86.7%). Interestingly, the tetA gene (66.7%) was more prevalent than the tetB gene (8.3%) in TE-resistant E. coli isolates in this study. Only two SXT-resistant E. coli isolates (22.2%) harbored the sul1 gene responsible for SMX resistance. The dfrA1 gene was the most prevalent TMP resistance gene, followed by the dfrA9 gene (22.2%) and dfrA17 gene (11.1%) (Table 3).
All 30 AR isolates were screened for the presence of integrase genes. Only four isolates harbored an integrase gene (all class 1 integrase gene, intI1). These isolates were all obtained from horses (three from horse feces and one from the nasal cavity). Although only two were defined as MDR isolates based on the definition in this study, they all carried at least two antimicrobial resistance genes (Table 4).
Out of the 143 E. coli isolates, only 41 (28.7%) were defined by their serotypes based on the serotyping methods used in this study. The 41 isolates were clustered into 19 serotypes including O28ac (O28ac/H-, 4 isolates) and O148 (O148/H- and O148/H7, 4 and 1 isolates, respectively) (data not shown).
Since the serotyping method used in this study revealed serotypes from only three of the 30 AR isolates, all of the AR isolates were subjected to PFGE analysis to determine their genetic relatedness. Two AR isolates did not show electrophoresed bands and were therefore excluded from the analysis. Except for 5 isolates clustered into two clonal sets (Type G and L), all AR isolates showed distinct genotypes that indicated weak genetic relatedness (Type A to Y) (Fig. 1). In the case of type G, two E. coli isolates showed the same antibiogram profiles and were isolated from the feces of two different horses on the same horse-riding course. In the case of type L, three E. coli isolates showing slightly different antibiogram profiles were acquired from different sample sources (feces, feed box and nasal cavity) at the same national racetrack (Fig. 1).
To date, many studies have evaluated the prevalence of AR bacteria in food and pet animals and the risk of transmission to humans [2526]. However, only a few studies have investigated leisure and sports animals, such as horses, for antimicrobial resistant microorganisms. The recent increase in the horse racing and riding industries in Korea [14] indicates an increased possibility of introducing horse-related pathogens into human communities. In this study, we investigated the frequency of antimicrobial resistant E. coli isolated from horses and surrounding environments and characterized AR E. coli to evaluate the risk of transmission to humans. This is the first study conducted to isolate and characterize AR bacteria from horses using samples collected nationwide, including from three national horse racetracks in Korea.
E. coli is one of the most commonly isolated bacteria from animal related specimens [9]. However, the isolation rates from horse related samples were generally low in the current study (overall average: 4.6%). E. coli are first secreted from the animal intestine by fecal shedding, then spread to other material by contact transmission. Except for the primary source of E. coli (feces, 8.0%) and their first contact material (bedding, 27.3%), E. coli isolation rates from horses and their surrounding environments were very low (< 4%). These findings indicate that all of the investigated horse related facilities maintain a good hygienic management that minimizes the transmission of fecal contaminants. All of the facilities we visited kept a high level of hygiene by immediate removing dropped feces, frequently replacing bedding and periodically cleaning the facilities.
Out of the 143 E. coli isolated, 30 (21%) showed resistance to at least one antimicrobial compound. This frequency was much less that observed for E. coli isolated from fecal samples of hospitalized horses (81.7%), but similar to that for healthy horses (24.5%) [1]. When E. coli isolated from horses and environments was compared, the AR rate was higher in isolates collected directly from horses. In addition, MDR E. coli and E. coli carrying class I integrase gene, a gene associated with multi-drug resistance in bacteria, were only isolated from horses. These results are somewhat different from a previous study in which the frequencies of AR E. coli from animals were similar to or higher than those from environments in food animal farms [24]. Therefore, the lower AR ratio of environmental isolates in this study might suggest good hygienic management in the horse facilities minimized fecal contamination of the environment as mentioned above.
The most frequently detected phenotypes of antimicrobial resistance in AR E. coli were against S, TE and SXT in the current study. This pattern is very similar to the results from a previous study conducted in northwest England [1], and suggests a relationship with the amount of antimicrobials used in equine medicine. In veterinary medicine, streptomycin is the first-line antimicrobial for Gram-negative bacterial infection in horses [28]. Oxytetracycline, which is the most commonly used antimicrobial, use applied in an injectable form in combination with a sulfa antimicrobial agent to treat bacterial respiratory infections in horses [32]. Similarly, Enterococcal spp. isolated from the same samples used in this study also showed high antimicrobial resistance to TE (18.6%, unpublished data). SXT has also been used extensively for oral administration to horses due to the minor side-effects on the normal microflora of the horse intestine [8].
As shown in Table 3, many of the AR E. coli isolated in this study harbored corresponding antimicrobial resistance genes (60–100% in each AR group). The AR E. coli without the antimicrobial resistance genes may have other kinds of antimicrobial resistance genes not screened in this study, or alternative resistance mechanisms such as a biofilm formation [13]. Consistent with the results of a previous study [2], the TEM gene was most prevalent in AM-resistant E. coli isolates. Most AR E. coli resistant to S, the most prevalent phenotype of antimicrobial resistance in this study, contained strA-B genes (13/15), which are known to confer a higher level of resistance to E. coli than the aadA gene [27]. Our findings indicate that E. coli harboring strA-B genes are prevalent in healthy horses in Korea. The portion of genes responsible for TE resistance in E. coli is different from that in other countries [5]. While the tetB gene was the prevalent resistance gene in TE-resistant E. coli isolated from horses in the United States [5], most TE-resistant E. coli harbored the tetA gene in this study. Additionally, all TMP-resistant E. coli harbored at least one of the dfr genes, which are usually encoded on mobile genetic elements including plasmids or transposons [3]. The most predominant dfr gene they harbored was dfrA1gene (88.9%, Table 3), which is consistent with the results of a study conducted in northwest England [1]. However, the dfrA17 gene was reported to be the predominant antimicrobial resistance gene to TMP in E. coli isolated from hospitalized horses at the university of Liverpool, UK [2]. Taken together, these results suggest that horse riders and horse-care workers could be transmitters of these AR E. coli to other humans.
Class 1 integron, which is known to be an important genetic element carrying TMP resistance genes in E. coli, is horizontally transferred by conjugative plasmids [33]. Lee et al. [16] reported that most of the TMP-resistant E. coli isolates harbored dfr genes encoded in intI. Class 1 integron is also known to carry multiple resistance genes in enterobacteria [18]. Similarly, all four E. coli isolates carrying the class 1 integron harbored at least two different antimicrobial resistance genes, and two of these were MDR E. coli based on the phenotypical definition (resistant to more than three antimicrobials) in this study. These findings indicate that integrase genes are strongly related to multi-drug resistance, as previously suggested [23].
Out of the 143 isolates, 41 were serotyped into 19 different serological groups, while the remaining isolates were un-typed by the anti-sera used in this study (data not shown). The 19 defined serological groups included two clinically important serotypes, O28ac and O148, in humans [21]. O28ac is associated with EIEC, which cause non-bloody diarrhea and dysentery by invading and multiplying within colonic epithelial cells. O148 is related to ETEC, which cause travelers' diarrhea [21]. Yun et al. [34] previously reported the prevalence of O28ac and O148 to be 3.1% and 1.1%, respectively, in E. coli isolated from thoroughbred brood mares in Korea. In the current study, the prevalence of the O28ac serotype in E. coli isolated from healthy horses and environments was similar (2.8%) to that observed in a study conducted by Yun et al. [34], but the prevalence of O148 serotype was slightly higher (3.5%) than that from thoroughbred brood mares in the previous study (data not shown).
Since serotyping only revealed the serotypes of three out of 30 AR E. coli isolates, PFGE analysis was performed for all AR isolates to analyze the clonal relatedness among isolates. Our results revealed no clear evidence of clonal expansion of AR E. coli in horses and their environments. However, two types of clones showed cross-transmission between horses or horses and their associated environments within the same facilities. These results indicate that horses could be carriers of AR E. coli to environments and other animals. Thus, these findings suggest a potential possibility of transmission of AR E. coli from horses to humans via close contact as previously demonstrated between companion animals and humans [11].
In conclusion, this is the first study to isolate and characterize AR E. coli from healthy horses and their environments by nationwide sampling in Korea. The results indicate that all of the investigated racetracks and private horse-riding courses maintain a high level of hygienic management and there was no clonal transmission of AR E. coli among horse facilities. However, the E. coli isolated from horses showed a considerably high level of antimicrobial resistance, including multidrug resistance. Due to the frequent contact with horses, our study indicates that horse-care workers and riders may be exposed to a potential risk of infection with AR and pathogenic bacteria carried by horses. Therefore, further studies are needed to evaluate the risk of transmission of AR bacteria between horses and horse riders or workers in horse industries.
Figures and Tables
 | Fig. 1Pulsed-field gel electrophoresis (PFGE) analysis of antimicrobial-resistant E. coli isolates. All the genomic DNA samples were digested with XbaI followed by standard PFGE analysis (see Materials and Methods). Levels of similarity were determined using Dice coefficient (0.5% optimization, 1.0% tolerance) and the un-weighted pair group method. Individual PFGE patterns are summarized with their isolate ID, antimicrobial resistance profiles, sample sources and PFGE types. *Identification number of each E. coli isolate was given as the serial number of the sampling facility followed by the isolate number in the facility. †Antimicrobial- resistance profiles. ‡Reference strain for PFGE analysis. §Not resistant to any tested antimicrobials. TE, tetracycline; SXT, sulfamethoxazole/trimethoprim; AMC, amoxicillin/clavulanic acid; AM, ampicillin; CTT, cefotetan; S, streptomycin; GM, gentamicin; ATM, aztreonam. |
Table 2
Antimicrobial resistance (AR) profiling of E. coli isolated from different samples

*,†A total of 30 isolates (21%) were defined as AR E. coli from horses (n = 25; 13 from feces, 6 from skins and 6 from nasal cavities, respectively) and environmental samples (n = 5; 2 from drinking water and 3 from bedding, respectively). Note that AR E. coli showing resistance to more than one antimicrobial agent were redundantly counted in each antimicrobial resistant test. AM, ampicillin; AMC, amoxicillin/clavulanic acid; GM, gentamicin; TE, tetracycline; SXT, sulfamethoxazole/trimethoprim; ATM, aztreonam; S, streptomycin; CTT, cefotetan; MDR, multi-drug resistance.
Acknowledgments
This study was supported by a grant (Z-1541778-2013-13-01) from Animal and Plant Quarantine Agency, Ministry of Agriculture, Forestry and Livestock, Republic of Korea in 2013. An additional support was provided by the BK21 PLUS Program for Creative Veterinary Science Research, Seoul National University, Korea.
References
1. Ahmed MO, Clegg PD, Williams NJ, Baptiste KE, Bennett M. Antimicrobial resistance in equine faecal Escherichia coli isolates from North West England. Ann Clin Microbiol Antimicrob. 2010; 9:12.

2. Ahmed MO, Williams NJ, Clegg PD, Baptiste KE, Bennett M. Antibiotic resistance patterns in faecal E. coli: a longitudinal cohort-control study of hospitalized horses. In : Pana M, editor. Antibiotic Resistant Bacteria – A Continuous Chanllenge in the New Millennium. InTech: Rijecka;2012.
3. Amyes SG, Smith JT. R-factor trimethoprim resistance mechanism: an insusceptible target site. Biochem Biophys Res Commun. 1974; 58:412–418.

4. Bennett PM. Plasmid encoded antibiotic resistance: acquisition and transfer of antibiotic resistance genes in bacteria. Br J Pharmacol. 2008; 153:Suppl 1. S347–S357.

5. Bryan A, Shapir N, Sadowsky MJ. Frequency and distribution of tetracycline resistance genes in genetically diverse, nonselected, and nonclinical Escherichia coli strains isolated from diverse human and animal sources. Appl Environ Microbiol. 2004; 70:2503–2507.

6. Clinical and Laboratory Standards Institute. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard–Eighth Edition. CLSI document M07-A8. Wayne: Clinical and Laboratory Standards Institute;2009.
7. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing: Nineteenth Informational Supplement. CLSI document M100-S19. Wayne: Clinical and Laboratory Standards Institute;2009.
8. van Duijkeren E, Vulto AG, Slot van Oldruitemborgh-Oosterbaan MM, Mevius DJ, Kessels BGF, Breukink HJ, van Miert ASJPAM. A comparative study of the pharmacokinetics of intravenous and oral trimethoprim/sulfadiazine formulations in the horse. J Vet Pharmacol Ther. 1994; 17:440–446.

9. Erb A, Stürmer T, Marre R, Brenner H. Prevalence of antibiotic resistance in Escherichia coli: overview of geographical, temporal, and methodological variations. Eur J Clin Microbiol Infect Dis. 2007; 26:83–90.

10. Gibreel A, Sköld O. High-level resistance to trimethoprim in clinical isolates of Campylobacter jejuni by acquisition of foreign genes (dfr1 and dfr9) expressing drug-insensitive dihydrofolate reductases. Antimicrob Agents Chemother. 1998; 42:3059–3064.

11. Guardabassi L, Schwarz S, Lloyd DH. Pet animals as reservoirs of antimicrobial-resistant bacteria. J Antimicrob Chemother. 2004; 54:321–332.
12. Guinée PA, Agterberg CM, Jansen WH. Escherichia coli O antigen typing by means of a mechanized microtechnique. Appl Microbiol. 1972; 24:127–131.

13. Ito A, Taniuchi A, May T, Kawata K, Okabe S. Increased antibiotic resistance of Escherichia coli in mature biofilms. Appl Environ Microbiol. 2009; 75:4093–4100.

14. Kim JY. The horse industry in Korea: its present condition and prospect. Adv Sci Technol Lett. 2015; 99:256–260.

15. Kos VN, Desjardins CA, Griggs A, Cerqueira G, Van Tonder A, Holden MTG, Godfrey P, Palmer KL, Bodi K, Mongodin EF, Wortman J, Feldgarden M, Lawley T, Gill SR, Haas BJ, Birren B, Gilmore MS. Comparative genomics of vancomycin-resistant Staphylococcus aureus strains and their positions within the clade most commonly associated with methicillin-resistant S. aureus hospital-acquired infection in the United States. MBio. 2012; 3:e00112–e00112.
16. Lee JC, Oh JY, Cho JW, Park JC, Kim JM, Seol SY, Cho DT. The prevalence of trimethoprim-resistance-conferring dihydrofolate reductase genes in urinary isolates of Escherichia coli in Korea. J Antimicrob Chemother. 2001; 47:599–604.

17. Levy SB, Marshall B. Antibacterial resistance worldwide: causes, challenges and responses. Nat Med. 2004; 10:12 Suppl. S122–S129.

18. Martinez-Freijo P, Fluit A, Schmitz FJ, Grek VSC, Verhoef J, Jones ME. Class I integrons in Gram-negative isolates from different European hospitals and association with decreased susceptibility to multiple antibiotic compounds. J Antimicrob Chemother. 1998; 42:689–696.

19. Nataro JP, Kaper JB. Diarrheagenic Escherichia coli. Clin Microbiol Rev. 1998; 11:142–201.
20. Ng LK, Martin I, Alfa M, Mulvey M. Multiplex PCR for the detection of tetracycline resistant genes. Mol Cell Probes. 2001; 15:209–215.

21. Persson S, Olsen KE, Scheutz F, Krogfelt KA, Gerner-Smidt P. A method for fast and simple detection of major diarrhoeagenic Escherichia coli in the routine diagnostic laboratory. Clin Microbiol Infect. 2007; 13:516–524.

22. Pitout JD, Thomson KS, Hanson ND, Ehrhardt AF, Moland ES, Sanders CC. beta-Lactamases responsible for resistance to expanded-spectrum cephalosporins in Klebsiella pneumoniae, Escherichia coli, and Proteus mirabilis isolates recovered in South Africa. Antimicrob Agents Chemother. 1998; 42:1350–1354.

23. Recchia GD, Hall RM. Gene cassettes: a new class of mobile element. Microbiology. 1995; 141:3015–3027.

24. Sayah RS, Kaneene JB, Johnson Y, Miller R. Patterns of antimicrobial resistance observed in Escherichia coli isolates obtained from domestic- and wild-animal fecal samples, human septage, and surface water. Appl Environ Microbiol. 2005; 71:1394–1404.

25. So JH, Kim J, Bae IK, Jeong SH, Kim SH, Lim SK, Park YH, Lee K. Dissemination of multidrug-resistant Escherichia coli in Korean veterinary hospitals. Diagn Microbiol Infect Dis. 2012; 73:195–199.

26. Soufi L, Abbassi MS, Sáenz Y, Vinué L, Somalo S, Zarazaga M, Abbas A, Dbaya R, Khanfir L, Ben Hassen A, Hammami S, Torres C. Prevalence and diversity of integrons and associated resistance genes in Escherichia coli isolates from poultry meat in Tunisia. Foodborne Pathog Dis. 2009; 6:1067–1073.

27. Sunde M, Norström M. The genetic background for streptomycin resistance in Escherichia coli influences the distribution of MICs. J Antimicrob Chemother. 2005; 56:87–90.

28. Thakur A, Vashist H, Sharma RB. A review on tuberculosis. Eur J Biomed Pharm Sci. 2015; 2:1106–1126.
29. Tsen HY, Lin CK, Chi WR. Development and use of 16S rRNA gene targeted PCR primers for the identification of Escherichia coli cells in water. J Appl Microbiol. 1998; 85:554–560.

30. Van TT, Chin J, Chapman T, Tran LT, Coloe PJ. Safety of raw meat and shellfish in Vietnam: an analysis of Escherichia coli isolations for antibiotic resistance and virulence genes. Int J Food Microbiol. 2008; 124:217–223.

31. White PA, McIver CJ, Deng YM, Rawlinson WD. Characterisation of two new gene cassettes, aadA5 and dfrA17. FEMS Microbiol Lett. 2000; 182:265–269.
32. Woody BJ, Hoskins JD. Ehrlichial diseases of dogs. Vet Clin North Am Small Anim Pract. 1991; 21:75–98.

33. Yu HS, Lee JC, Kang HY, Jeong YS, Lee EY, Choi CH, Tae SH, Lee YC, Seol SY, Cho DT. Prevalence of dfr genes associated with integrons and dissemination of dfrA17 among urinary isolates of Escherichia coli in Korea. J Antimicrob Chemother. 2004; 53:445–450.

34. Yun SW, Kwon DY, Choi SK, Lee HS, Cho GJ. Characteristics and antimicrobial susceptibility of Escherichia coli isolated from horse. Korean J Vet Res. 2010; 50:231–237.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download