Abstract
This study was conducted to analyze the prevalence and quantitative loads of Salmonella spp. on pig farms in Chiang Mai, Lamphun, Thailand to assess loading levels before slaughtering. The serotype diversity, antimicrobial-resistance pattern and pulse-field type of Salmonella spp. were also characterized to assess the dynamic propagation of the pathogen. The Salmonella-positive prevalence was 246/805 (30.56%), and the quantitative loads varied from 1.48~4.04 Log10MPN/g, with a mean ± standard deviation of 2.11 ± 0.57. AMP/S/TE (ampicillin/streptomycin/tetracycline) was the highest frequency antimicrobial resistance pattern found in this study. In addition, Salmonella Rissen was the primary serotype in this region. PFGE results indicated the occurrence of infection by cross contamination among pig farms. Our study showed that pork is easily contaminated with this pathogen. Farm control programs must be based on strict biosecurity and hygienic measures, which could further reduce the contamination pressure at slaughterhouses or retail shops.
Salmonella spp. comprises one of the most important bacterial-zoonotic pathogens, causing acute food-borne diseases in humans [28], and is recognized as a major public health problem [10]. Salmonellosis is the group of clinical conditions caused by Salmonella spp., and an estimated 80.3 million cases of foodborne Salmonellosis occur worldwide annually [23]. Clinically, Salmonellosis in humans may start with an acute onset of fever, nausea, headache, vomiting and profuse diarrhea within 8~48 h of ingesting the pathogen. The severity of the disease depends on the ingested dose and the host's immune status [14]. Although contaminated eggs and raw or undercooked poultry are the primary sources of Salmonellosis in humans, pork causes an estimated 15~20% of all cases [16]. While contamination can occur during any process along the food production line [1,21], infected pigs on the farm are the origin of the contaminated pork that leads to human infections [12].
Several studies have assessed Salmonella prevalence on farms. García-Feliz reported a Salmonella prevalence of 43.1% in finishing pig herds in Spain [9]. In contrast, Visscher reported a Salmonella prevalence of 5.58% in fattening pigs in Lower Saxony, Germany [28]. However, Salmonella spp. data is insufficient for quantitative measurement and development of strategies to reduce the risk of this pathogen.
Pig farmers routinely use antibiotics for both treatment and prophylactic purposes. Excessive and incorrect uses of antibiotics are probably a primary cause of increasing bacterial resistance [23,27]. In addition, further study of the antibiotic resistance profiles of isolates is needed to develop antibiotic resistance profiles of pigs for porcine and human cases.
Pathogen characterization is essential for investigation of foodborne bacteria epidemiology. Serotyping is one of the most common techniques used for Salmonella characterization. However, this technique has a lower discriminatory power than molecular techniques such as pulsed field gel electrophoresis (PFGE). PFGE has long been accepted as a molecular characterization method for a wide range of bacterial species, including Salmonella. This technique clearly and precisely distinguishes bacterial genotypic diversity and is more appropriate for epidemiological investigations of foodborne pathogens, such as Salmonella spp. [8].
The objectives of this study were to determine the prevalence and quantitative loads of Salmonella spp. at the farm level in Chiang Mai - Lamphun to assess loading levels before going to the slaughterhouse and define the diversity of Salmonella spp. by phenotypic and serotypic characterizations. In addition, the pulse-field types were assessed to determine dynamic propagation, including origin, evaluation and common source of infection or transmission patterns of Salmonella spp. in the study area.
The present study was performed on six farms (A~F) in Chiang Mai - Lamphun (Thailand). A total of 606 fecal samples were randomly collected from the rectum of pigs by the individual finger palpation method. Fecal samples from pigs aged 4, 8, 12, 18 and 24 weeks, sows and boars were collected for further microbiological assay for detection and quantification purposes. In addition, 199 environmental samples were collected, including swabs from the floor of the animal house, feeder, nipple-drinker, and worker's hands and boots (100 cm2/samples). Samples were also collected from the drinking water, feed and pests (such as flies). All samples were shipped in an icebox to the Central Laboratory, Chiang Mai University, for Salmonella isolation within 24 h of collection.
Isolation and identification of Salmonella spp. was conducted following the ISO 6579:2002 Amendment 1:2007, Annex D technique (Detection of Salmonella spp. in animal feces and environmental samples from the primary production stage) to determine the prevalence and numbers of positive samples [13].
For the qualitative assay, solid samples of fresh feces, feed and flies were obtained. Next, nine times the amount of buffered peptone water (BPW; Merck, Germany) was added as pre-enrichment media (25 g of solid sample was added to 225 mL of BPW). The mixture was then homogenized using a stomacher machine for 2 min. Following incubation at 37℃ for 24 h, an aliquot of 0.1 mL was transferred to a Modified Semi-solid Rappaport-Vassiliadis (MSRV; Oxiod, UK). The samples were then incubated at 42℃ for 24 h, after which the material from this agar was streaked onto xylose lysine deoxycholate agar (XLD; Oxiod) and brilliant-green phenol red lactose sucrose agar (BPLS; Merck) and incubated at 37℃ for 24 h. The presumptive Salmonella colonies were further processed for biochemical tests, including measurement of triple sugar iron (TSI; Oxiod), urease and motile indole lysine decarboxylase (MIL; Merck).
Environmental samples such as drinking-water were also added into nine times the quantity of BPW as pre-enrichment media and incubated at 37℃ for 24 h. Next, aliquots of 0.1 mL and 1 mL were transferred to 9.9 mL of Rappaport-Vassiliadis broth (RV; Merck) and 9 mL of tetrathionate broth (TT; Merck), respectively. After incubation at 42℃ for 24 h for RV and 37℃ for 24 h for TT, material taken from each broth was streaked onto selective solid media (XLD and BPLS agar), and a biochemical test for presumptive colonies was conducted.
Environmental swab samples were subjected to the same procedure used for drinking-water samples, except that these samples were prepared with 100 mL of BPW, rather than nine times the weight, in the pre-enrichment process.
In the quantitative assays, the number of Salmonella was determined using the most probable number (MPN) technique. From each positive sample, which was kept refrigerated, three replicates in three portions (3 × 0.1 mL, 3 × 0.01 mL and 3 × 0.001 mL) were taken aseptically and added individually to tubes with BPW. All processes of Salmonella identification were performed as qualitative tests, and all suspected colonies from selective media were continually confirmed as Salmonella by biochemical tests. Salmonella-positive results were used to estimate Salmonella quantification with the MPN calculator [17].
A total of 200 Salmonella-positive isolates were randomly serotyped as appropriate by the WHO National Salmonella and Shigella Center Laboratory (NSSC), Nonthaburi, Thailand. In addition, each serotype was submitted to antimicrobial susceptibility testing. Susceptibility to a panel of ten antimicrobial agents was investigated and interpreted by disk diffusion [4]. If isolates showed intermediate resistance [4], they were grouped with the susceptible isolates to avoid overestimation of resistance. The antibiotics were abbreviated as follows: ampicillin (AMP); amoxicillin-clavulanic acid (AUG); chloramphenicol (C); ciprofloxacin (CIP); cefotaxime (CTX); nalidixic acid (NA); norfloxacin (NOR); streptomycin (S); tetracycline (TE); sulfamethoxazole-trimethoprim (SXT) (Oxoid).
DNA fingerprinting of the first major serotype isolated in this study was conducted using PFGE at the Infectious Diseases Molecular Epidemiology Laboratory (IDMEL) of Ohio State University. Twenty-five isolates were selected at random and subjected to PFGE according to the CDC's standardized PulseNet protocol for Salmonella [19]. The PulseNet "Universal" standard strain Salmonella enterica serovar Braenderup H9812 was used as a reference marker, and XbaI was used as a digestion enzyme. Gel images were transferred to Bionumerics software ver. 3.5 for cluster analysis. Cluster analysis was performed using the unweighted pair group method, with optimization with 1.0% band position tolerances and 2.5% optimization values. Similarity coefficients were obtained within Bionumerics by calculating Dice coefficients. PFGE banding patterns with a similarity index >75% were grouped within the same genotypic cluster.
The data were collected and analyzed for descriptive statistical analysis of Salmonella in both prevalence and numbers by Microsoft Excel and PHstat2. A Chi-square test and ANOVA were used to compare the proportion of the presence of Salmonella and the mean of the MPN numbers, respectively, in each group of samples by StataSE9.0 (StataCorp, USA).
The overall prevalence of Salmonella spp. in pig farms in Chiang Mai - Lamphun was 30.56% (246/805). For the fecal samples, 34.98% (212/606) of the positives samples were included. These were classified into seven groups included in this study. According to the Chi-square test, the greatest prevalence was in finishing pigs aged 12 weeks (57.73%, 95% CI: 47.90~67.56). The prevalence of Salmonella-positive samples in the environment was 17.08% (34/199), which was lower than that of the fecal samples. No positive results were observed in the feed samples, and the prevalence of Salmonella in the environmental samples was not significantly different among the six farms (p > 0.05).
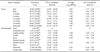
We were unable to re-isolate Salmonella spp. from 87 samples (74 fecal samples and 13 environmental samples) during the quantification assays. Consequently, some sample types could not be quantified, including the drinking-water, worker's hands and fly samples. In the remaining 159 positive samples, the number of Salmonella ranged from 1.48~4.04 Log10MPN/g, with a mean ± standard deviation (SD) of 2.11 ± 0.57 (data not shown). In addition, there was no significant difference between sample groups (Table 1).
Table 2 shows the serodiversity of 200 randomly selected Salmonella strains. Up to 20 serotypes were found in this study. The highest frequency isolate was Salmonella Rissen (28%), followed by Salmonella Typhimurium (15.5%) and Salmonella I. 4,5,12 : i : - (13.5%). Salmonella I. 4,12 : i : -, Salmonella IV. ser 43:z4z23, Salmonella Agona, Salmonella Krefeld and Salmonella Mbandaka were present at the lowest frequencies (0.5% each). In addition, 9 of 20 serotypes were found in both the fecal and environmental samples. However, 9 and 2 serotypes were unique to the fecal and environmental samples, respectively.
Fig. 1 shows the percentage of antimicrobial resistant Salmonella strains (n = 200). Most isolates were resistant to ampicillin (AMP) (81.5%), followed by tetracycline (TE) (74.5%), streptomycin (S) (70.5%) and sulfa-trimethoprim (SXT) (35.5%). However, none of the isolates showed resistance to norfloxacin (NOR), ciprofloxacin (CIP) or amoxicillin-clavulanic acid (AUG).
The distribution of antimicrobial resistance patterns is summarized in Table 3. This study found 25 different resistance patterns among the 200 isolates. One hundred sixty-nine isolates showed resistance to at least one antimicrobial drug, while 31 isolates were susceptible to all drugs tested. Most samples in this study showed patterns common to both fecal and environmental samples (145 isolates in eight resistance-patterns), followed by samples showing resistance patterns only observed in fecal samples (53 samples in 15 resistance-patterns). Only two patterns were observed in only one isolate from each environmental sample. The highest frequency antimicrobial resistance pattern among the tested isolates in this study was AMP/S/TE (ampicillin/streptomycin/tetracycline).
Salmonella Rissen, the most common type observed in this study, was randomly selected (n = 25) from fecal samples for pulse-field gel electrophoresis characterization. The PFGE XbaI macrorestriction banding patterns consisted of 10~12 DNA fragment bands. PFGE generated two major genotypic clusters (X-Y) with a dice coefficient index cut-off point of 75% (Fig. 2). The similarity among cluster X was about 75~100%, and represented the predominant group in this study, which comprised 18 isolates (from farms A, B and D in 8, 2, and 8 isolates, respectively). The Salmonella Rissen isolated from farm A and B showed identical DNA fingerprint profiles clustered in only one genotypic group (cluster X). Cluster Y contained two indistinguishable isolates from farm C. Interestingly, among samples from farm D, all isolates (8/8) from cluster X and all isolates from cluster Y (5/5) belonged to different pig type samples, suggesting a different source of infection among starters and sows in farm D. Finally, the antimicrobial resistance patterns of isolates from the same farm were partially different, except for six isolates from farm A and two isolates from farm C, which showed a similar pattern.
The overall prevalence of Salmonella spp. was 30.56%, comprised of 34.98% from fecal samples and 17.08% from environmental samples. The prevalence of Salmonella in the fecal samples was similar to the 43.1% prevalence reported in finishing pigs from a study of fattening units in Spain [9], with comparable isolation technique. However, our study revealed substantially lower prevalence than other studies in Northern Thailand, which recorded prevalence in pre-slaughter pigs of 55% [20] and 63% [6]. These differences might be due to the timing of sampling ("on farm" in our study and pre-slaughter in their study), with the stress during transportation and lairage potentially increasing the shedding of Salmonella from the intestinal lumen [15,26]. In contrast, a study of finishing pigs conducted in Germany revealed lower prevalence (5.65%) than our study [28]. Fecal swabs from the rectum may not be sufficient to compare with the amount of feces (up to 25 g) collected in our study, and good management practices in Germany may reduce pathogen levels on farms.
Upon comparison of sample types, prevalence from environmental samples was generally lower than fecal samples, except for flies and worker's boot samples. Flies are a major vehicle for foodborne pathogens, and boots of workers easily come into contact with animal feces; thus, their prevalence may be higher than that of other environmental samples.
In this study, Salmonella spp. could not be recovered from 87 samples using quantitative assays, although corresponding portions of the same samples were positive in the qualitative assays. The heterogeneous distribution and the overall low number of Salmonella in the samples may have been due to a failure of re-isolation procedures [16]. The MPN range of the remaining Salmonella-positive samples was quite low (1.48~4.04 Log10MPN/g for the fecal samples and 1.56~3.38 Log10MPN/g for the environmental samples). However, under the right conditions, even 1 CFU can grow to several million [25]. Therefore, relatively low levels of Salmonella at any point in the production process can have a large impact if they have the opportunity to proliferate to hazardous numbers under improper conditions [21]. Some such conditions may include longer waiting times in lairage, contributing to increased shedding of the pathogen from the intestinal lumen [15,23], inadequate processing of the carcasses in the slaughterhouse, such as evisceration, resulting in carcass contamination [3,15,26], and temperature abuse in retail shops, leading to increasing contamination levels [2,5,7,11,15].
This study demonstrated that two major serotypes, Salmonella Rissen and Salmonella Typhimurium, were the most common observed during pig production in Chiang Mai - Lamphun, Thailand. These serotypes have been reported as the dominant serotype in pigs in the same region [6,18], and Salmonella Rissen was also the most common Salmonella serotype found in healthy humans in Upper Northern Thailand [18]. The serodiversity of Salmonella-positive samples from feces and the environment were quite similar, suggesting that the environment is a potential source of Salmonella infection in pigs [28]. The post-infected animal could be highly susceptible to re-infection when exposed to the environment [6]. Interestingly, Salmonella Typhimurium was only found in fecal samples, which differs from several studies in which Salmonella Typhimurium was also present in the environment [6,21,28]. Organisms in these samples may have been destroyed by exposure to sunlight or disinfectants, or there may have been no common source of infection with this serotype between pigs and the environment. In this study, some serotypes were found only in environmental samples, suggesting that other sources not sampled in this study played roles as important shedders, such as wild birds, lizards or invertebrates.
We also demonstrated the widespread occurrence of antimicrobial resistance. Specifically, resistance (21.5% to 81.5%) to ampicillin, tetracycline, streptomycin, sulfa-trimethoprim and chloramphenicol was observed, which is concordant with the results of previous studies of Salmonella epidemiology in pigs, pork and humans in Belgium and Thailand [22,27]. Antimicrobial drugs from the same groups as ampicillin, streptomycin, tetracycline and sulfa-trimethoprim have been widely used on pig farms in Thailand. Sub-dosing or extra-label usage could explain the high rates of resistance [23,24,27]. In contrast, chloramphenicol was banned from animal production more than 10 years ago; however, resistance to this antibiotic could be due to horizontal gene transmission [27]. The observed absence of resistance to norfloxacin, ciprofloxacin and amoxicillin-clavulanic acid may have been due to the limited use of these antimicrobial drugs in pig production in Thailand. The highest frequency resistance was reported in AMP/S/TE, and in both sample types (pigs and environment). This finding suggests that there is horizontal transmission of the antimicrobial resistance-gene between Salmonella strains from feces to the environment.
PFGE profiling was used to identify similarities of Salmonella in the Salmonella Rissen isolates. The results also indicated the occurrence of cross contamination among pig farms. There were 12 isolates with identical PFGE patterns (similarity indexes of ≥95) from two different farms (A & D) classified in the same group (cluster X). This finding demonstrated that sources of Salmonellosis may spread over a wide area via the same supply chain (e.g., gilt, feed or feed-ingredients) or a common source of infection among farms (e.g., a transportation truck). In addition, all isolates from farm D were separated into two distinguishable genotypic groups among starters and sows, indicating no common source of infection between the two age groups. This may indicate that there is no common source of infection between the fattening and farrowing units, which are located approximately 10 km apart. However, in this study, infection in pigs resulting from environmental exposure could not be determined precisely. Thus, further investigation might be needed to assess the genotypic profiles of the positive environmental samples. When we compared the PFGE results and antimicrobial resistance patterns, the same antimicrobial resistance patterns with the same farm origin were observed, contrary to a previous study by Pulsrikarn et al. [22], who demonstrated that there was no association between PFGE and antimicrobial resistance patterns. This finding suggests that horizontal resistance gene transmission may be occurring among these farms.
Salmonella on farms is the first-origin of Salmonellosis in human cases, and is unlikely to be alleviated effectively in the short term. Farm control programs must be based on strict biosecurity and hygiene measures to minimize the risk of Salmonella exposure to many potential infection sources. Moreover, these findings highlight the need for continuous monitoring, along with greater focus on problem solving at the farm level, which can reduce the contamination pressure downstream at slaughterhouses and retail shops.
Figures and Tables
Fig. 1
The percentage antimicrobial resistance of Salmonella strains (n = 200) from pig farms in Chiang Mai, Lamphun, Thailand.

Fig. 2
Dendrogram representing PFGE-XbaI identified in the 1st majority serotype with antimicrobial resistance patterns of Salmonella Rissen (n = 25) from farms A~D in Chiang Mai, Lamphun, Thailand, with similarity determined by the Dice co-efficient and UPGMA clustering. The antibiotic resistance patterns include 10 antibiotics: ampicillin (AMP); amoxicillin-clavulanic acid (AUG); chloramphenicol (C); ciprofloxacin (CIP); cefotaxime (CTX); nalidixic acid (NA); norfloxacin (NOR); streptomycin (S); tetracycline (TE); sulfamethoxazole-trimethoprim (SXT).

Table 1
Distribution and quantification of Salmonella-positive samples isolated from pig farms in Chiang Mai, Lamphun, Thailand
Acknowledgments
This research is financially supported by the National Science and Technology Development Agency (NSTDA) Project ID: P-10-10409. The author would like to thank the farms and their staff for participating in this study. We would also like to thank the students and technicians who helped with sample collection and processing, the WHO National Salmonella and Shigella Center Laboratory (NSSC), Thailand, and colleagues at Chiang Mai University and the Ohio State University for their significant contribution.
References
1. Berends BR, Van Knapen F, Mossel DA, Burt SA, Snijders JM. Impact on human health of Salmonella spp. on pork in The Netherlands and the anticipated effects of some currently proposed control strategies. Int J Food Microbiol. 1998; 44:219–229.

2. Berends BR, Van Knapen F, Mossel DAA, Burt SA, Snijders JMA. Salmonella spp. on pork at cutting plants and at the retail level and the influence of particular risk factors. Int J Food Microbiol. 1998; 44:207–217.

3. Berends BR, Van Knapen F, Snijders JM, Mossel DA. Identification and quantification of risk factors regarding Salmonella spp. on pork carcasses. Int J Food Microbiol. 1997; 36:199–206.

4. CLSI. Performance Standards for Antimicrobial Disc Susceptibility Test; Approved standard-Ninth Edition. CLSI document M2-A9. Wayne: Clinical and Laboratory Standards Institute;2006.
5. Delhalle L, Saegerman C, Farnir F, Korsak N, Maes D, Messens W, De Sadeleer L, De Zutter L, Daube G. Salmonella surveillance and control at post-harvest in the Belgian pork meat chain. Food Microbiol. 2009; 26:265–271.

6. Dorn-in S, Fries R, Padungtod P, Kyule MN, Baumann MP, Srikitjakarn L, Chantong W, Sanguangiat A, Zessin KH. A cross-sectional study of Salmonella in pre-slaughter pigs in a production compartment of northern Thailand. Prev Vet Med. 2009; 88:15–23.

7. Escartín EF, Lozano JS, Rodríguez O, Gonzáles NM, Torres JA. Incidence and level of Salmonella serovars in raw pork obtained from mexican butcher shops. Food Microbiol. 1995; 12:435–439.

8. Foxman B. Molecular Tools and Infectious Disease Epidemiology. 1st ed. Burlington: Academic Press;2012. p. 23–40.
9. García-Feliz C, Collazos JA, Carvajal A, Vidal AB, Aladueña A, Ramiro R, De La Fuente M, Echeita MA, Rubio P. Salmonella enterica infections in Spanish swine fattening units. Zoonoses Public Health. 2007; 54:294–300.

10. Giovannini A, Prencipe V, Conte A, Marino L, Petrini A, Pomilio F, Rizzi V, Migliorati G. Quantitative risk assessment of Salmonella spp. infection for the consumer of pork products in an Italian region. Food Control. 2004; 15:139–144.

11. Gonzales-Barron UA, Redmond G, Butler F. A risk characterization model of Salmonella Typhimurium in Irish fresh pork sausages. Food Res Int. 2012; 45:1184–1193.

12. Hauser E, Hebner F, Tietze E, Helmuth R, Junker E, Prager R, Schroeter A, Rabsch W, Fruth A, Malorny B. Diversity of Salmonella enterica serovar Derby isolated from pig, pork and humans in Germany. Int J Food Microbiol. 2011; 151:141–149.

13. International Standard Organization. ISO 6579:2002(E). Microbiology of food and animal feeding stuffs - Horizontal method for the detection of Salmonella spp. 4th ed. Geneva: ISO;2002.
14. Jawetz E, Melnick JL, Adelberg EA. Review of Medical Microbiology. 16th ed. Los Altos: Lange Medical Publication;1984. p. 244–248.
15. Lo Fo Wong DMA, Hald T, van der Wolf PJ, Swanenburg M. Epidemiology and control measures for Salmonella in pigs and pork. Livest Prod Sci. 2002; 76:215–222.
16. Mürmann L, dos Santos MC, Cardoso M. Prevalence, genetic characterization and antimicrobial resistance of Salmonella isolated from fresh pork sausages in Porto Alegre, Brazil. Food Control. 2009; 20:191–195.

17. Oblinger JL, Koburger JA. Understanding and teaching the most probable number technique. J Milk Food Technol. 1975; 38:540–545.
18. Padungtod P, Kaneene JB. Salmonella in food animals and humans in northern Thailand. Int J Food Microbiol. 2006; 108:346–354.
19. Patchanee P, Molla B, White N, Line DE, Gebreyes WA. Tracking Salmonella contamination in various watersheds and phenotypic and genotypic diversity. Foodborne Pathog Dis. 2010; 7:1113–1120.

20. Patchanee P, Zessin KH, Staak C, Srikijkarn L, Taravijitkul P, Tesaprateep T. Pre-slaughther infection of Salmonella spp. and consideration of using the DANISH MIX-ELISA for monitoring Salmonella in pigs. Chiang Mai Vet J. 2003; 1:33–38.
21. Prendergast DM, Duggan SJ, Gonzales-Barron U, Fanning S, Butler F, Cormican M, Duffy G. Prevalence, numbers and characteristics of Salmonella spp. on Irish retail pork. Int J Food Microbiol. 2009; 131:233–239.

22. Pulsrikarn C, Chaichana P, Pornruangwong S, Morita Y, Yamamoto S, Boonmar S. Serotype, antimicrobial susceptibility, and genotype of Salmonella isolates from swine and pork in Sa Kaew province, Thailand. Wetchasan Sattawaphaet. 2012; 42:21–27.
23. Rostagno MH, Callaway TR. Pre-harvest risk factors for Salmonella enterica in pork production. Food Res Int. 2012; 45:634–640.
24. Schwaiger K, Huther S, Hölzel C, Kämpf P, Bauer J. Prevalence of antibiotic-resistant enterobacteriaceae isolated from chicken and pork meat purchased at the slaughterhouse and at retail in Bavaria, Germany. Int J Food Microbiol. 2012; 154:206–211.

25. Stephens PJ, Joynson JA, Davies KW, Holbrook R, Lappin-Scott HM, Humphrey TJ. The use of an automated growth analyser to measure recovery times of single heat-injured Salmonella cells. J Appl Microbiol. 1997; 83:445–455.

26. Swanenburg M, van der Wolf PJ, Urlings HAP, Snijders JMA, van Knapen F. Salmonella in slaughter pigs: the effect of logistic slaughter procedures of pigs on the prevalence of Salmonella in pork. Int J Food Microbiol. 2001; 70:231–242.

27. Van Boxstael S, Dierick K, Van Huffel X, Uyttendaele M, Berkvens D, Herman L, Bertrand S, Wildemauwe C, Catry B, Butaye P, Imberechts H. Comparison of antimicrobial resistance patterns and phage types of Salmonella Typhimurium isolated from pigs, pork and humans in Belgium between 2001 and 2006. Food Res Int. 2012; 45:913–918.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download