Abstract
In human medicine, diagnosis of diabetic ketoacidosis (DKA) is usually based on measurement of capillary 3-β-hydroxybutyrate (3-HB) with a hand held ketone sensor. This study was conducted to determine if measurement of capillary 3-HB could be useful for the diagnosis and monitoring of canine DKA. Fifteen dogs with diabetic ketosis and 10 with DKA were evaluated. Paired measurements of 3-HB of capillary and venous blood samples were analysed by the electrochemical sensor and reference method. Use of capillary 3-HB measurement during DKA management was then evaluated through simultaneous measurements of capillary 3-HB, urinary AcAc and venous blood gas analysis. Good agreement between capillary and venous 3-HB measurement was detected by the electrochemical sensor and reference method. Monitoring treatment of DKA revealed a significant correlation between capillary 3-HB and acidosis markers, while no significant correlation was observed between AcAc and acidosis markers. A cut-off value of capillary blood 3-HB >3.8 mmol/L for diagnosis of DKA resulted in 70% and 92% sensitivity and specificity. The electrochemical sensor accurately measures 3-HB concentration in both capillary and venous blood samples, is accurate in diagnosing canine DKA, and appears to reflect the patient's metabolic status during DKA treatment.
Diabetic ketoacidosis (DKA) is a severe life threatening complication of diabetes mellitus (DM) characterised by the biochemical triad of hyperglycaemia, metabolic acidosis, and ketosis [8]. Decreased insulin concentration and/or increased insulin resistance coupled with increased counter regulatory hormones concentration caused by concurrent diseases or medications may contribute to increased peripheral lipolysis, and ultimately to the production of ketone bodies such as acetoacetate (AcAc), 3-beta-hydroxybutyrate (3-HB) and acetone [8]. Accumulation of ketoacids beyond a basal concentration leads to development of metabolic acidosis [17,21].
Diabetic ketoacidosis is associated with significant morbidity and mortality in humans and animals [15,16,21,27]; accordingly, delays in diagnosis and treatment are likely to result in increased risk of mortality to these patients [15]. Dogs with DKA require an intensive therapeutic plan involving frequent clinical assessment and laboratory monitoring [19].
To diagnose DKA, a state of ketonemia or ketonuria must be detected, along with acidosis, in blood or urine samples. In human medicine, 3-HB is known to be the predominant ketone body in DKA patients, and the 3-HB : AcAc ratio rises from 1 : 1 in healthy patients to 5 : 1 during DKA [24].
The commonly used urine dipstick test, which is based on a nitroprusside reaction, gives a semiquantitative measure of urinary AcAc, but does not register the presence of urinary 3-HB, the predominant ketone body [8,21]. Urinary or plasma semiquantitative measure of AcAc is associated with a considerable risk of false positive and negative results, both in humans and animals [3,6,23,27,32]. Finally, obtaining a urine sample for a rapid diagnosis may be difficult in emergency cases [3,25,27,32]. For this reason, in human medicine, blood ketones are now measured using a hand-held electrochemical sensor that measures 3-HB in 30 sec using capillary whole blood samples [1,25,27,28]. This method is actually the recommended method for diagnosis and monitoring of the treatment of DKA, and can be used for the home monitoring of diabetic patients [1,10,12,18,25,26,27,28].
Urinary AcAc is still the most commonly used method for diagnosis in veterinary medicine, but in recent years some studies have been performed to investigate the utility of 3-HB concentration for diagnosis of DM or DKA. Hand-held ketone sensors [6,13,14,29] or reference laboratory methods [7,8,31,32] for analysis of venous blood samples were used in these studies, and the results suggested that 3-HB measurement was superior to urinary AcAc for diagnosis of canine and feline DKA [6,13,14,29,31,32]. Therefore, the present study was conducted to evaluate the accuracy of an electrochemical sensor (Optium Xceed; Abbott Laboratories, UK) for measurement of 3-HB from capillary and venous blood samples, and to assess the potential utility of the capillary 3-HB measurement to diagnose and monitor the treatment of canine DKA.
Dogs with diabetic ketosis (DK) or DKA in a population of patients referred to the Veterinary Teaching Hospital of University of Bologna between May 2009 and October 2011 were enrolled in the study. Dogs with DK (DK group) met the following inclusion criteria: blood glucose ≥250 mg/dL) and ketonemia (blood 3-HB ≥0.1 mmol/L) and/or ketonuria (urinary AcAc > negative), absence of metabolic acidosis (pH > 7.3 and bicarbonate (HCO3-) >15 mEq/L) and no clinical signs compatible with DKA (anorexia, severe lethargy, vomiting and dehydration) and were managed on an outpatient basis. Dogs with DKA (DKA group) met the following inclusion criteria: blood glucose ≥250 mg/dL, ketonemia (blood 3-HB ≥0.1 mmol/L) and/or ketonuria (urinary AcAc >negative), metabolic acidosis (pH < 7.3 or bicarbonate <15 mEq/L), at least two clinical signs compatible with DKA (anorexia, severe lethargy, vomiting, and dehydration), and required hospitalization with an intensive therapeutic plan. Approval for this study was given by the Scientific - Ethics Committee, University of Bologna, Italy (PROT: 54464-X/10).
Venous blood samples were collected by jugular or cephalic venepuncture and analysed for routine complete blood count (CBC), biochemical profile, and blood gas analysis (Idexx VetStat, Idexx Laboratories, Italy). Blood samples for blood gas analysis were collected with 2.5 mL heparinised syringes and analysed immediately. Venous blood samples were also used for the detection of 3-HB with a standard laboratory enzymatic method (D-3-Hydroxybutyrate, Ranbut; Randox Laboratories, UK) from the serum obtained after centrifugation (laboratory 3-HB) and with the ketone sensor (Optium Xceed, Optium β-ketone Test Strips; Abbott Laboratories) [5] from whole blood immediately after collection (venous 3-HB).
Capillary blood samples used for glucose and 3-HB measurement were collected from the inner pinna of all animals using the Vaculance method and a Microlet Vaculance lancing device (Microlet Vaculance; Bayer Diagnostics, Switzerland) as previously described [30]. Capillary 3-HB concentrations (capillary 3-HB) were measured using a hand-held sensor (Optium Xceed, Optium β-ketone Test Strips; Abbott Laboratories). This sensor, which was previously validated for dogs [9], was also used for capillary glucose measurement according to the manufacturer's protocols. The assay range was 0.0 mmol/L to 8.0 mmol/L. Above this value, the meter displays a reading of "Hi", which was considered to be equal to 8.0 mmol/L for this study.
Urine was collected by spontaneous urination, cystocentesis or catheterisation for measurement of urinary AcAc by nitroprusside reaction test strips (H-Series Urinalysis Reagent Strips; DIRUI Industrial, China), which allowed semiquantitative measurement of AcAc. This test gives the following results: negative (0), 15 mg/dL (±), 50 mg/dL (1+), 100 mg/dL (2+) and 150 mg/dL (3+).
Evaluation of the accuracy of the electrochemical sensor to measure 3-HB in capillary and venous blood samples was made in the DK and DKA groups by the correlation of simultaneous measurement of capillary 3-HB, venous 3-HB and laboratory 3-HB concentrations. To select the optimum cut-off values for diagnosis or exclusion of a state of DKA, samples from DK and DKA dogs were included during diagnosis.
The use of capillary 3-HB to monitor the disease was assessed in DKA patients by comparing simultaneous measurements of capillary 3-HB with capillary blood glucose, acidosis markers (pH, HCO3- concentration, anion gap) and urinary AcAc. Simultaneous samples were defined as those collected within 10 min, except for urine, for which simultaneous collection was defined as samples collected within 2 h of blood collection.
Patients with DKA were treated with fluid therapy to correct the fluid deficit and electrolyte imbalance, a continuous low dose of an intravenous infusion of regular insulin, and miscellaneous treatment for concomitant disorders [19]. Dogs with DKA were monitored closely. During the first 24 h, capillary blood glucose was monitored hourly, while capillary 3-HB was measured every 4 h and venous 3-HB and laboratory 3-HB, urinary AcAc and blood gas were measured every 8 h. In the next 24~48 h, capillary blood glucose was monitored every 2~3 h, while capillary 3-HB was measured every 4 h and then every 12 h and venous 3-HB and laboratory 3-HB, urinary AcAc and blood gas were measured every 12 h.
Statistical analysis was performed using commercially available software (Graph Prism 5.01; GraphPad Software, USA; MedCalc ver. 10.2.0.0; MedCalc Software, Belgium). Microsoft Excel 2011 was used for tables and descriptive statistics, in which data were described based on medians and ranges. The normality of the variables was assessed using the Shapiro-Wilk test. Since the data did not meet the assumption of Gaussian distribution, non parametric tests were used. The capillary 3-HB values obtained from the 2 groups were compared by the Mann-Whitney U test. The relationship between simultaneous samples of 3-HB from different substrates was evaluated by Spearman's correlation. Bias and limits of agreement were investigated using Bland-Altman plot analysis. A receiving-operating characteristic (ROC) curve was used to determine the area under the curve (AUC) and select the optimum cut-off values for diagnosis or exclusion of a state of DKA. The relationships between capillary 3-HB and urinary AcAc; capillary 3-HB and pH, HCO3-, AG, and glycaemia; urinary AcAc and pH, HCO3-, AG, and glycaemia; glycaemia and pH, HCO3- and AG, were determined using Spearman's correlation. A p value < 0.05 was considered significant.
Twenty-five patients, 15 with DK and 10 with DKA, were enrolled in the study. Based on signalment, no statistical differences were observed between groups. Sixty percent of DKA dogs had received insulin for at least 7 days before initial evaluation and 30% had not been diagnosed with DM and did not receive insulin before referral, while 10% were diagnosed with DM but did not receive insulin before being referred. Predominant reported symptoms in DKA dogs were lethargy (100%), anorexia (100%), vomiting (70%), polyuria/polydipsia (70%), abdominal enlargement (30%), and panting (30%), while 10% had anuria, diarrhoea, hematemesis, gait abnormalities and mucous in faeces. Half (50%) had a subjectively overweight body condition, 30% had a normal body condition and 20% were underweight.
Based on the symptoms and clinicopathological findings, 90% had a precipitant factor diagnosed at the time of evaluation of DKA. Additionally, 60% dogs had one concomitant disorder, 10% was in diestrus, 10% had two concomitant disorders and 10% had four concomitant disorders. Half (50%) of dogs had pancreatitis, while other reported diseases included chronic kidney disease (20%), hyperadrenocorticism, intestinal neoplasia, diestrus, liver disease, paraparesis and gastroenteropathy (10% each). The only dog without concurrent disorders had been diagnosed with DM about one month prior to the study, but was not receiving insulin treatment as per the owner's instructions.
Hydroxybutyrate, blood glucose, urinary AcAc concentration, and blood gas analysis results of DK and DKA patients on admission are reported on Table 1. Blood gas analysis was performed upon initial evaluation for all DKA dogs (Table 1). All dogs had decreased serum HCO3- concentration (100%) and increased AG (100%), while 90% had decreased serum pH, and 90% had decreased pCO2.
All patients (100%) were hyperglycaemic and hyponatremic upon initial evaluation, 70% had a normal potassium concentration and 60% were hypochloremic. Calculated serum osmolality was increased in 60% of dogs. Urinalysis was performed in 100% DKA dogs (Table 2). All dogs had glucosuria (100%), 80% had ketonuria at the time of diagnosis and 20% had negative ketonuria upon diagnosis.
In all DKA patients, 3-HB was measured in capillary and venous blood samples with the ketone sensor and in venous blood samples with the reference method. All (100%) patients had 3-HB values ≥0.5 mmol/L in all three substrates. The median capillary 3-HB value was 4.8 mmol/L (range 0.6~6.5 mmol/L) (Table 1).
The ketone sensor was evaluated in patients with DK or DKA within 81 paired measurements of capillary 3-HB, venous 3-HB, and laboratory 3-HB. The DKA group had significantly higher capillary 3-HB values than the DK group (p = 0.0017).
A good direct correlation between capillary 3-HB and laboratory 3-HB (p < 0.0001, r = 0.80), as well as between venous 3-HB and laboratory 3-HB (p < 0.0001, r = 0.94) was found (Fig. 1). For Bland-Altman analysis, mean differences (mean ± SD, 95% limits of agreement) between venous 3-HB and laboratory 3-HB were -0.11 ± 0.5 mmol/L (-0.88 to 1.11), while they were -0.04 ± 0.69 mmol/L (-1.39 to 1.31) between capillary 3-HB and laboratory 3-HB (Fig. 1).
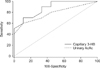
Based on evaluation of the ROC curve, the AUC of capillary 3-HB was 0.90 (95% confidence interval 0.70 to 0.98), while urinary AcAc was 0.78 (95% confidence interval 0.53 to 0.93). Comparison of the ROC curves for the two tests did not reveal a significant difference between the AUCs (Fig. 2). The results indicate that a cut-off value of capillary 3-HB >3.8 mmol/L had 70% and 92% sensitivity and specificity (positive likelihood ratio (LR+) 9.8 and LR - 0.32) for diagnosis of DKA, respectively. A cut-off value of capillary 3-HB <0.5 mmol/L had 100% and 64% sensitivity and specificity (LR+ 2.80 and LR- 0.00) to exclude DKA, respectively. A value of urinary AcAc >1+ suggests a DKA with 60% and 89% sensitivity and specificity (LR+ 5.40, LR- 0.45), respectively (Table 3).
The use of capillary 3-HB to monitor DKA was assessed by correlating simultaneous measurements of capillary 3-HB with capillary blood glucose, acidosis markers and urinary AcAc.
Spearman correlation revealed a significant positive correlation between capillary 3-HB and urinary AcAc (p < 0.0001, r = 0.78), capillary 3-HB and AG (p = 0.036, r = 0.32), and urinary AcAc and AG (p = 0.006, r = 0.47). A negative correlation was found between capillary 3-HB and pH (p = 0.033, r = -0.30), capillary 3-HB and HCO3- concentration (p = 0.014, r = -0.34), and capillary 3-HB and pCO2 (p = 0.017, r = -0.33). Non-significant correlations (p > 0.05) were found between urinary AcAc and pH, HCO3- concentration, pCO2 and blood glucose concentration, blood glucose concentration and capillary 3-HB, pH, AG, HCO3- concentration and pCO2. Spearman correlation results are shown in Table 4.
Diabetic ketoacidosis is an acute complication of DM, and prompt diagnosis of this disease allows better outcome [15]. Diagnosis is based on the detection of hyperglycaemia, metabolic acidosis, and ketonemia or ketonuria. Proposed methods to detect the increase of ketone bodies include 3-HB measurement with laboratory methods [7], which is not practical in emergency settings, the determination of urinary or plasma AcAc with dip stick methods [3,31,32], and the detection of 3-HB using a hand-held ketone sensor [6,14,29]. The detection of urinary AcAc is the most commonly used method, but many studies have demonstrated that this test is associated with a considerable risk of false-positive and false-negative results [3,31,32]. Based on the severity of the disease, a false positive result is less dangerous because the disease can then be excluded by the blood gas analysis. Conversely, a false negative result may result in underestimation of the patient's ketotic state and consequent misdiagnosis of the DKA. Based on a study conducted by Zeugswetter and Pagiz [32], the determination of plasma ketones by the dipstick test appears to have a greater sensitivity than the urinary ketone test and therefore to be a useful tool to rule out DKA. Both tests only detect the presence of AcAc in urine or plasma samples and not the presence of 3-HB; furthermore, the measurement of plasma ketones by the dipstick test is associated with false positive results [3,32].
Based on our results, there was a significant correlation between capillary 3-HB and laboratory 3-HB, which was similar to one reported in human medicine [4]. The collection of a capillary blood sample is a quick and easy procedure to perform [30]. Furthermore, the ketone sensor is a very simple method to use because it only requires 10 µL of capillary blood and 30 seconds to obtain the results. Conversely, collecting urine samples for AcAc measurement in very dehydrated, obese or uncooperative animals can be difficult.
Based on the results of this study, DKA should be strongly suspected in dogs with capillary 3-HB >3.8 mmol/L. Similarly, in human medicine, a cut-off value of capillary 3-HB >3.0 mmol/L is indicative of DKA [27], and studies in veterinary medicine identified a cut-off value of venous 3-HB >3.8 mmol/L [7] and >3.5 mmol/L [6], respectively, as indicative of DKA. Conversely, no cut-off values were detected for urinary AcAc to diagnose DKA, in both human [23,25] and veterinary medicine [6,7].
In our study, capillary 3-HB < 0.5 mmol/L can exclude DKA with 100% sensitivity and 64% specificity. Patients with 3-HB values between 0.5 and 3.8 mmol/L could be in a DK or DKA state, in which case further analyses are warranted. The considerable overlap between the 3-HB values of the DKA and DK group may limit the use of this measurement as a single test to diagnose DKA. This overlap was not unexpected because the metabolic abnormalities associated with the hyperglycaemic state can be viewed as a continuum progressing from the uncomplicated DM to overt DKA.
The results of ROC curve analysis showed that urinary AcAc values greater than 1+ indicate DKA (60% sensitivity and 89% specificity). Based on our findings, false positive and false negative results can occur, which can lead to an underestimation of the severity of the ketotic state. One out of 16 (6%) DK dogs had a urinary AcAc concentration greater than 1+. Furthermore, in the DKA group, 40% of dogs had urinary AcAc less than 1+. Two of these had negative ketonuria upon diagnosis, while only one became moderately ketonuric (urinary AcAc = ±) after 8 h of therapy and then returned to a non-ketonuric state after 16 h. Another dog was moderately ketonuric (urinary AcAc = ±) upon diagnosis, and become non-ketonuric after 16 h, but was still in acidosis with elevated capillary 3-HB. Based on results and individual cases indicate that urinary AcAc concentration can underestimate the patient's ketotic state and might not allow correct diagnosis of DKA, as previously reported [6,7,23].
The results of this study show that the capillary 3-HB appears useful for detection of an impending DKA in patients with uncontrolled DM or in patients with DM that show symptoms referable to ketoacidosis. It is well known that home monitoring of capillary blood glucose can improve the management of diabetic patients in both human and veterinary medicine [2,5]. Similarly, for detection of impending DKA, the self-monitoring of capillary 3-HB in human diabetic patients is recommended [1]. Our results suggest that home monitoring of capillary 3-HB could be useful to avert DKA in canine diabetic patients; however, further studies are recommended to investigate this possibility.
In human medicine, capillary 3-HB is considered a useful and reliable method to monitor the treatment of DKA [10,11,20,26,27]. This method imparts clinicians with the ability for earlier detection of inefficacy of the treatment of DKA relative to ketonuria [11]. Furthermore, this method allows easy and close monitoring and is less unpleasant than urine collection for both the patient and operators [11,20,26].
Hydroxybutyrate is formed from AcAc in the presence of hydrogen ions, with more acidotic animals showing more 3-HB formation [21]. The ratio of 3-HB:AcAc has been shown to increase when pH decreases, and to decrease when ketoacidosis is being recovered [21], which leads to an increase of 3-HB at diagnosis and during inefficient treatment, and to a delayed increase of AcAc in plasma or urine when DKA is going to be resolved. These findings suggest that urinary AcAc monitoring during DKA management might lead to a delay in treatment, as demonstrated in human medicine [20,26]. Our results showed that capillary 3-HB demonstrated a good correlation with acidosis markers (pH and HCO3-), while urinary AcAc was not correlated with pH or HCO3- concentration. Moreover, the blood glucose was not correlated with acidosis markers and is therefore not considered a reliable parameter to monitor the recovery from DKA, as previously described [22]. These results show that, during treatment of DKA, capillary 3-HB level is directly related to the severity of acidosis. 3-HB level is also a more sensitive method for determining a patient's metabolic status during treatment in comparison to urinary AcAc. This aspect has not yet been described in the veterinary literature, but is well known in human patients [20,26]. A possible explanation is that urinary measurements of a substance are not measurements of one time point, but are instead integrated over a long time period.
In the present study, all samples for 3-HB determinations have been collected without problems. Conversely, not all urine samples were collected due to difficulties in collection of those samples from non-catheterised animals. Capillary blood 3-HB measurement is a practical method that showed good correlation with the degree of acidosis during DKA management and appears superior to urinary AcAc for monitoring of these patients.
It should be noted that the present study has a number of limitations, such as the small number of dogs with DKA included. One limitation is that we did not use a clinical score to objectivise the clinical improvement of the patients. A clinical score could be correlated with the laboratory parameters, especially with the capillary 3-HB concentrations upon diagnosis and during treatment. However, it is our subjective impression that the capillary 3-HB concentrations were well correlated with the clinical improvement of the patients. In most cases, when 3-HB and acidosis markers normalized, mental status, appetite, vomiting and diarrhoea improved.
Further studies that include a DKA control population treated via conventional monitoring (urinary AcAc) could demonstrate if 3-HB measurement optimizes or otherwise improves management (i.e. shorter intravenous therapy, shorter hospitalization and better outcome) of DKA patients.
Further studies to investigate the variations of 3-HB and AcAc during the treatment of DKA are recommended. Durocher et al. [8] have demonstrated that 3-HB concentration, expressed as the percentage of total serum ketone concentration, decreases as total serum ketone concentration increases. To the best of our knowledge, no studies have investigated the concentration of 3-HB and AcAc relative to the total serum ketone concentrations upon diagnosis and during the treatment of DKA. Such information could provide important information about the role of the two predominant ketone bodies during canine DKA.
In conclusion, the hand-held ketone sensor appears to be an easy and reliable method for detection of capillary 3-HB or venous 3-HB in diabetic patients with DK or DKA. Moreover, capillary 3-HB appears to be an accurate method for detection of DKA that is significantly correlated with patient metabolic status during treatment of canine DKA relative to urinary AcAc.
Figures and Tables
Fig. 1
Spearman's correlation and Bland-Altam plots of (A) capillary hydroxybutyrate (3-HB) measured with a ketone sensor and venous hydroxybutyrate (3-HB) measured using the laboratory method (p < 0.0001, r = 0.80) and (B) venous 3-HB measured with a ketone sensor and venous 3-HB measured using a laboratory method (p < 0.0001, r = 0.94).

Fig. 2
Receiving operating characteristic curve of capillary 3-HB and urinary AcAc test assessed by comparing dogs with DK and DKA.
Notes
References
1. American Diabetes Association. Hyperglycemic crises in diabetes. Diabetes Care. 2004; 27:Suppl 1. S94–S102.
2. American Diabetes Association. Self-monitoring of blood glucose. Diabetes Care. 1994; 17:81–86.
3. Brady MA, Dannis JS, Wagner-Mann C. Evaluating the use of plasma hematocrit samples to detect ketones utilizing urine dipstick colorimetric methodology in diabetic dogs and cats. J Vet Emerg Crit Care. 2003; 13:1–6.

4. Byrne HA, Tieszen KL, Hollis S, Dornan TL, New JP. Evaluation of an eletrochemical sensor for measuring blood ketones. Diabetes Care. 2000; 23:500–503.
5. Casella M, Wess G, Reusch CE. Measurement of capillary blood glucose concentrations by pet owners: a new tool in the management of diabetes mellitus. J Am Anim Hosp Assoc. 2002; 38:239–245.

6. Di Tommaso M, Aste G, Rocconi F, Guglielmini C, Boari A. Evaluation of a portable meter to measure ketonemia and comparison with ketonuria for the diagnosis of canine diabetic ketoacidosis. J Vet Intern Med. 2009; 23:466–471.

7. Duarte R, Simoes DMN, Franchini ML, Marquezi ML, Ikesaki JH, Kogika MM. Accuracy of serum β-hydroxybutyrate measurements for the diagnosis of diabetic ketoacidosis in 116 dogs. J Vet Intern Med. 2002; 16:411–417.

8. Durocher LL, Hinchcliff KW, DiBartola SP, Johnson SE. Acid-base and hormonal abnormalities in dogs with naturally occurring diabetes mellitus. J Am Vet Med Assoc. 2008; 232:1310–1320.

9. Fracassi F, Hadar GS, Pietra M, Famigli-Bergamini P. Assessment of two portable blood glucose meters for use in cats and dog. J Vet Clin Sci. 2009; 2:108–121.
10. Guerci B, Benichou M, Floriot M, Bohme P, Fougnot S, Franck P, Drouin P. Accuracy of an electrochemical sensor for measuring capillary blood ketones by fingerstick samples during metabolic deterioration after continuous subcutaneous insulin infusion interruption in type 1 diabetic patients. Diabetes Care. 2003; 26:1137–1141.

11. Guerci B, Tubiana-Rufi N, Bauduceau B, Bresson R, Cuperlier A, Delcroix D, Fermon C, Le Floch JP, Le Devehat C, Melki V, Monnier L, Mosnier-Pudar H, Taboulet P, Hanaire-Broutin H. Advantages to using capillary blood β-hydroxybutyrate determination for the detection and treatment of diabetic ketosis. Diabetes Metab. 2005; 31:401–406.

12. Harris S, Ng R, Syed H, Hillson R. Near patient blood ketone measurements and their utility in predicting diabetic ketoacidosis. Diabet Med. 2005; 22:221–224.

13. Henderson DW, Schlesinger DP. Use of a point-of-care beta-hydroxybutyrate sensor for detection of ketonemia in dogs. Can Vet J. 2010; 51:1000–1002.
14. Hoenig M, Dorfman M, Koenig A. Use of a hand-held meter for the measurement of blood beta-hydroxybutyrate in dogs and cats. J Vet Emerg Crit Care. 2008; 18:86–87.

15. Hume DZ, Drobatz KJ, Hess RS. Outcome of dogs with diabetic ketoacidosis: 127 dogs (1993-2003). J Vet Intern Med. 2006; 20:547–555.

16. Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, Wall BM. Management of hyperglycemic Crises in patients with diabetes. Diabetes Care. 2001; 24:131–153.

17. Laffel L. Ketone bodies: a review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab Res Rev. 1999; 15:412–426.

18. Laffel LMB, Wentzell K, Loughlin C, Tovar A, Moltz K, Brink S. Sick day management using blood 3-hydroxybutyrate (3-OHB) compared with urine ketone monitoring reduces hospital visits in young people with T1DM: a randomized clinical trial. Diabet Med. 2006; 23:278–284.

19. Macintire DK. Treatment of diabetic ketoacidosis in dogs by continuous low-dose intravenous infusion of insulin. J Am Vet Med Assoc. 1993; 202:1266–1272.
20. Noyes KJ, Crofton P, Bath LE, Holmes A, Stark L, Oxley CD, Kelnar CJH. Hydroxybutyrate near-patient testing to evaluate a new end-point for intravenous insulin therapy in the treatment of diabetic ketoacidosis in children. Pediatr Diabetes. 2007; 8:150–156.

21. O'Brien MA. Diabetics emergencies in small animals. Vet Clin North Am Small Anim Pract. 2010; 40:317–333.
22. Reineke EL, Fletcher DJ, King LG, Drobatz KJ. Accuracy of a continuous glucose monitoring system in dogs and cats with diabetic ketoacidosis. J Vet Emerg Crit Care (San Antonio). 2010; 20:303–312.

23. Rosenbloom AL, Malone JI. Recognition of impending ketoacidosis delayed by ketone reagent strip failure. JAMA. 1978; 240:2462–2464.

24. Stephens JM, Sulway MJ, Watkins PJ. Relationship of blood acetoacetate and 3-hydroxybutyrate in diabetes. Diabetes. 1971; 20:485–489.

25. Taboulet P, Deconinck N, Thurel A, Haas L, Manamani J, Porcher R, Schmit C, Fontaine JP, Gautier JF. Correlation between urine ketones (acetoacetate) and capillary blood ketones (3-beta-hydroxybutyrate) in hyperglycaemic patients. Diabetes Metab. 2007; 33:135–139.

26. Turan S, Omar A, Bereket A. Comparison of capillary blood ketone measurement by electrochemical method and urinary ketone in treatment of diabetic ketosis and ketoacidosis in children. Acta Diabetol. 2008; 45:83–85.

27. Wallace TM, Matthews DR. Recent advances in the monitoring and management of diabetic ketoacidosis. QJM. 2004; 97:773–780.

28. Wallace TM, Meston NM, Gardner SG, Matthews DR. The hospital and home use of a 30-second hand-held blood ketone meter: guidelines for clinical practice. Diabet Med. 2001; 18:640–645.

29. Weingart C, Lotz F, Kohn B. Validation of a portable hand-held whole-blood ketone meter for use in cats. Vet Clin Pathol. 2012; 41:114–118.

30. Wess G, Reusch C. Capillary blood sampling from the ear of dogs and cats and use of portable meters to measure glucose concentration. J Small Anim Pract. 2000; 41:60–66.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download