Abstract
Thirty-one dogs with patellar luxation (grades 2 and 3) were categorized into three groups. Group 1 (G.1; n = 12) had sodium hyaluronate (SHA) intra-articularly injected into the stifle joint that received surgery. Group 2 (G.2; n = 10) received SHA twice: first after surgery and then 1 week later. Group 3 (G.3; n = 9) served as a control, without injection. Blood was collected before injection and then once a week for 4 weeks after injection for evaluation of chondroitin sulfate (CS-WF6) and hyaluronan (HA). The results revealed significantly (p < 0.05) improved clinical scores by the end of week 4 in G.1 and G.2 relative to G.3; however, there was no significant difference between G.1 and G.2. There was a significant decrease (p < 0.05) in serum CS-WF6 levels beginning at week 2 in G.1 and G.2. At weeks 3 and 4, serum HA in G.1 and G.2 differed from that in G.3 (p < 0.05). No significant difference (p > 0.05) was observed in serum biomarkers between G.1 and G.2. In conclusion, intra-articular injection with SHA after joint surgery may improve homeostasis of the joint, retarding the process of OA.
The major component of synovial fluids is hyaluronan (HA), which is also an important component of articular cartilage. HA (also known as hyaluronic acid) provides a hydrodynamic fluid with viscoelastic properties that allows efficient movement of joints. Hyaluronic acid is composed of repeating sequences of disaccharides, glucuronic acid and N-acetylglucosamine, which are mainly synthesized by synoviocytes [12]. A decrease in the concentration of synovial fluid and a reduction in its viscoelastic properties can lead to osteoarthritis [20]. During joint surgery, synovial fluid is drained out and the joint is occasionally washed with normal saline. Moreover, some of the synovial membrane is destroyed as a consequence of the surgical procedure. These situations could lead to decreased synthesis of synovial fluid after joint surgery is performed.
Hyaluronan preparations are viscous solutions derived from extracts of rooster combs or bacterial fermentation. Many hyaluronan products are commercially available worldwide. Several clinical studies of human patients with chronic osteoarthritis conducted using placebos and other drugs have demonstrated the beneficial effects of intra-articular injection of hyaluronic acid [2,6,7,14,15,20,32]. Some studies have also reported beneficial effects of hyaluronan in cases of canine osteoarthritis (OA) [4,8,17,18,30,34]. However, previous research has focused on the effects of hyaluronan in the treatment of canine OA induced by anterior cruciate ligament transection or other models. Indeed, there is no existing literature on the use of hyaluronan for the prevention of OA after joint surgery in dogs or humans. Therefore, this study was conducted to investigate the effects of hyaluronan injected after joint surgery on clinical signs and biomarker changes in dogs.
Thirty-one client-owned dogs with patellar luxation (grades 2 and 3) were used as subjects in this study and were categorized into three groups (Table 1). After surgery was performed, the first group (G.1) of 12 dogs (age = 24 ± 12 months, weight = 3.11 ± 1.13 kg) was injected once with 0.5~1.0 mL of sodium hyaluronate (Hyalgan; TRB Chemedica, Switzerland). The second group (G.2) of dogs (n = 10, age = 27 ± 12 months, weight = 2.36 ± 1.25 kg) was injected with sodium hyaluronate after immediately surgery and again one week after surgery. The final group (G.3) of dogs (n = 9, age = 26 ± 12 months, weight = 2.33 ± 1.33 kg) served as a control and did not receive intra-articular injection of sodium hyaluronate after surgery. To eliminate potential errors from surgical techniques, all dogs underwent the same procedure for the correction of patellar luxation performed by the same surgeon. All animals were operated on using a combined technique that included medial desmotomy, overlap of lateral retinaculum, fascia lata overlap, patellar and tibial antirotational suture ligament. Informed owner consent was obtained, and the trial protocol was approved by the Faculty of Veterinary Medicine and the Ethics Committee, Chiang Mai University, Chiang Mai, Thailand.
Two veterinarians recorded the severity of clinical signs at each visit (weekly) using a clinical scoring system applied from Nganvongpanit [27] (Table 2). All veterinarians were blinded to the study. During the experiment, 3 mL of blood was collected from the cephalic vein of each dog for evaluation of the level of biomarkers for OA weekly [21,27].
Efficacy of the treatment was assessed by a clinical scoring system [17] that assessed the specific animal's lameness, pain on palpation, and weight-bearing. The dogs walked and trotted 6 m three times for evaluation of lameness by two veterinarians. This was followed by palpation of the stifle joint for determination of joint mobility and pain evaluation. The palpation was performed by two veterinarians 30 min apart. This evaluation was performed weekly (four times) after surgery.
Blood (3 mL) was collected from the cephalic vein of each dog five times during the study, before surgery, and then every week for the next 4 weeks. Blood samples were used to evaluate hematology, biochemistry and biomarkers.
Blood samples were analyzed for complete blood counts (CBCs), including hematocrit and hemoglobin levels, red blood cell count, white blood cell count (WBC) and platelet count. Additionally, 2 mL of serum were analyzed for aspartate aminotransferase (AST), alanine aminotransferase (ALT), blood urea nitrogen (BUN) and creatinine.
A mouse monoclonal antibody, WF6, was raised against a shark cartilage aggrecan preparation. Quantitative ELISA for the epitope recognized by the monoclonal antibody WF6 was modified from a previous study [21,25,27]. The antibody was specific for intact chondroitin sulfate chains and showed no interaction with other sulfated glycosaminoglycans, hyaluronan, or other polyanions such as DNA, RNA or dextran sulfate. The standard used in the assay was shark cartilage aggrecan (A1 fraction) at concentrations of 19~10,000 ng/mL in 6% bovine serum albumin (BSA) in TE buffer (0.1 M tris-HCl, pH 7.4, containing 0.15 M sodium chloride, 0.1% Tween 20 and 0.1% BSA). Diluted human serum samples (1 : 5 in 6% BSA-TE) were added to 1.5 mL plastic tubes containing an equal volume of WF6 (cell culture supernatant, 1 : 200 dilution in TE buffer). Samples were incubated at 37℃ for 1 h, after which they were added to the microtiter plate, which was precoated with shark aggrecan (A1 fraction). Non-specific protein binding was blocked with BSA. The plates were incubated at 37℃ for 1 h, after which the wells were washed and peroxidase-conjugated anti-mouse IgM antibody (1 : 2,000) was added (100 µL/well, in TE buffer). The bound conjugate was detected by adding o-phenylenediamine dihydrochloride (OPD) substrate (100 µL/well in 0.05 M citrate buffer, pH 5.0). The reaction was stopped after 10 min by the addition of 50 µL/well of 4 M sulfuric acid, at which time the absorbance at 492 ~ 690 nm was measured using a microplate reader. The concentration of WF6 epitope in supernatant samples was calculated by reference to a standard curve.
Human serum samples or standard HA (Healon) at various concentrations (19~10,000 ng/mL in 6% bovine serum albumin-phosphate buffered saline [BSA-PBS], pH 7.4) were added to 1.5 mL plastic tubes containing biotinylated HABPs prepared as described above (1 : 200 in 0.05 M tris-HCl buffer, pH 8.6). The tubes were incubated at room temperature for 1 h, after which samples were added to a microplate that had been precoated with umbilical cord HA (100 µL/well at 10 mg/mL) and blocked with 1% BSA (150 µL/well). The plate was then incubated at room temperature for 1 h. Next, the wells were washed and 100 µL/well peroxidase-conjugated anti-biotin antibody (1 : 2,000 dilution) in PBS was added. The plate was then incubated at room temperature for another hour. OPD substrate was then used for detection of the conjugated antibody, and plate reading was carried out as described above. The concentration of HA in samples was calculated from the standard curve [21,25,27].
The results of serum CS-WF6 and HA analysis are presented as the mean ± SD. A non-parametric 2-sample Mann-Whitney procedure was used to test for differences between groups in the same week, as well as before and after treatment. Clinical scores were calculated as the mean ± SD. The relative data were analyzed using the Statistical Analysis System (SAS) version 8.0 (SAS Institute, USA) software package. A p ≤ 0.05 was considered to be statistically significant.
The dogs in this study (male = 13, female = 18) were small breeds, including Yorkshire terrier (n = 7), Chihuahua (n = 7), Pomeranian (n = 12), shih tzu (n = 3) and poodle (n = 2). Only dogs with a unilateral medial patellar luxation of grade 2 (n = 14) or grade 3 (n = 17) (left = 16, right = 17) were used as subjects in this study. During joint surgery, all articular cartilages were observed; however, OA lesions were not found in all joints. Complete blood counts and serum biochemistry in all animals were normal during the study (data not shown).
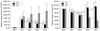
Clinical sign evaluations are shown in Fig. 1. Weight-bearing and pain on palpation scores for G.1 (2.8 ± 0.7, 1.5 ± 0.5) and G.2 (2.8 ± 0.5, 1.4 ± 0.5) were significantly lower (p < 0.05) than for G.3 (3.4 ± 0.5, 2.1 ± 0.7) at week 4 after surgery. Evaluation of the lameness score revealed that only G.2 (1.9 ± 0.6) was significantly lower than G.3 (2.5 ± 0.5).
The levels of serum CS-WF6 were elevated in all groups in the first week after surgery (Fig. 2). In G.3, this increase continued over the next 3 weeks, and was found to be very high in week 4 (2,575.33 ± 941.73). Conversely, in G.1 and G.2, the levels of serum CS-WF6 decreased after week 2. The level of CS-WF6 in G.3 was significantly higher (p < 0.05) than in G.1 and G.2 during weeks 2 to 4, while there was no significant difference between G.1 and G.2 (p > 0.05).
The level of serum HA in all groups decreased during the first two weeks, then increased over the last two weeks in G.1 and G.2, while it continued to decrease until the end of the study in G.3 (Fig. 2). The level of serum HA in G.3 was significantly lower (p < 0.05) than in the other two groups.
This study revealed that there was no significant difference in animals that received one- or two intra-articular injections of sodium hyaluronate after joint surgery and that both treatments were effective at preventing development of OA in canine stifle joints. These findings are similar to the results of a study conducted by Kolarz et al. [16], and suggest that sodium hyaluronate administered as either a single or repeat course is an effective and well-tolerated therapy for the long-term treatment of pain in OA. However, since no long-term effect was observed in our study, we terminated the experiment after 1 month. Accordingly, additional studies are needed for a thorough analysis of the effects of using single or multiple intra-articular injections of sodium hyaluronate, preferably experimental studies using animals rather than clinical studies so that all variable factors that have an effect on the results can be controlled.
This is the first report of the use of sodium hyaluronate after joint surgery in dogs. However, there were several limitations of this study. First, the injections were limited to once or twice during the first week, even though other studies have recommended 3~5 injections weekly [3,32]. This limitation was due to the procedure of intra-articular injection, during which dogs must undergo general anesthesia. In the present study, dogs were anesthetized much less often. Second, the number of samples was restricted because this was a clinical trial and not an experimental trial; consequently, the number of animals was limited by the number of cases in our hospital. Moreover, to avoid the effects of stage of disease and surgical technique, we limited the study to cases of unilateral medial patellar luxation grades 2~3. Finally, all procedures were performed by the same surgeon. Because of these restrictions, the number of animals that might have participated in the study was reduced by more than 50%. Third, we did not report the long-term effects (6 months or 12 months) after treatment because the number of dogs in each group was reduced due to owner conditions (time restrictions, moving away from the area, etc.). However, we are presently attempting to design an experiment to investigate the long-term effects of sodium hyaluronate injection during joint surgery for both single and multiple doses.
Human studies have shown that intra-articular injection of sodium hyaluronate is a relatively safe approach [9]. However, the side effects of sodium hyaluronate injection in dogs have not been reported. In this study, 32 intra-articular injections of sodium hyaluronate resulted in no observed side effects or adverse reactions. Nevertheless, some adverse effects have been reported in humans. Specifically, in a US study of 164 patients, 23% (n = 38) showed injection site pain [1]. Additionally, acute synovitis was associated with joint swelling lasting up to 3 weeks in some cases [28]. These reactions were typically mild and resolved without treatment. Based on our experience over the past three years, out of 154 joints injected with steroids or sodium hyaluronate, we found only 2 (1.3%) that showed side effects, which consisted of septic arthritis following injection (data not yet published). We believe that these side effects did not arise from the drugs, but from the intra-articular procedure itself.
Some previous human studies have shown that sodium hyaluronate injection (3 to 5 times) did not improve pain scores in OA patients [15,32]. However, the clinical scores in this study (including pain) were significantly improved in G.1 and G.2 at week 4 after surgery when compared to G.3, while there was no difference between G.1 and G.2 One important difference in our study may be that other studies primarily included OA patients who were mostly at the chronic stage, while the subjects in this study were at an early stage. It is possible that injection with sodium hyaluronate following joint surgery could improve clinical signs by decreasing pain and increasing function of the joint. Moreover, many other human studies have reported a significant reduction of pain. For example, sodium hyaluronate provided pain relief when a cycle of 3 to 5 injections was employed [22,26]. The effect of pain relief from sodium hyaluronate is not clearly understood; however, it may be due to its effects on nerve impulses and nerve sensitivity [26]. The analgesic effect of sodium hyaluronate is related to a reduction in sensitivity to mechanical forces of stretch-activated channels present in the membrane of joint mechanonociceptors [23]. The other possible mechanism of sodium hyaluronate in reducing pain is its effect on substance P (a small peptide involved in the transmission of pain signals). Sodium hyaluronate has been shown to inhibit increased vascular permeability induced by substance P [19]. Moreover, a previous review [20] reported that sodium hyaluronate has significant effects on inflammatory mediators such as decreased levels of prostaglandin E2 (PGE2) and leukotriene, suppressed production of tumor necrosis factor alpha (TNF-α), reduced arachidonic acid release or reduced nitric oxide (NO) production. It possible that reducing those inflammatory mediators has an effect on decreasing pain in sodium hyaluronate injected groups.
A novel monoclonal antibody, CS-WF6, recognizes an epitope in the native CS chain [25]. For anterior cruciate ligament (ACL) injury patients, instability results in an initial increase of proteoglycan content and collagen breakdown of articular cartilage within one year of injury [27,33]. This finding corresponds with the increasing proteoglycan level in synovial fluid and serum detected by cartilage markers. The present study also showed that after joint surgery dogs have increasing levels of serum CS-WF6, which indicates that the articular cartilage in the joint has degraded and developed a catabolism pathway. We found the levels of CS-WF6 in the first week of the study to be 1,450 ± 266% higher than pre-surgery levels. However, in the second week, CS-WF6 levels decreased in the sodium hyaluronate-injected groups (to 900 ± 105%) when compared to pre-surgery groups, while in the non-injected group the serum level increased to 2,085%. At the end of the study (week 4), the level of CS-WF6 between one-time and two-time sodium hyaluronate injection was not significantly different (618% and 530% higher than pre-surgery), while the level of CS-WF6 in the non-injected group was 2,575% greater than the pre-surgery level. Thus, it can be concluded that sodium hyaluronate injection can inhibit degradation of the cartilage matrix. In a review by Moreland in 2003 [20], many in vitro experiments indicated that sodium hyaluronate can enhance the synthesis of extracellular matrix proteins (i.e. chondroitin, keratin sulfate, and proteoglycans) and reduce expression of interleukin-1β and matrix matelloproteinase-3.
Previous studies have reported that sodium hyaluronate concentrations in the joint fluid and serum of animals with diseased joints were lower than normal [3,10,24]. Additionally, several studies using acute injury models have demonstrated decreasing HA concentrations in synovial fluid [3,10]. Our study revealed decreases of HA of 13 ± 3% and 30 ± 4% in the first and second weeks after surgery, respectively. The level of serum HA in the sodium hyaluronate-injected group was increased to close to pre-surgery levels in weeks 3~4, but there was no significant difference between groups that received one and two injections. However, in the non-injected group, serum HA levels decreased by 45% and 62% in weeks 3 and 4, respectively. Exogenous sodium hyaluronate may facilitate the production of newly synthesized HA by synoviocytes [31]. Although HA is a good biomarker, it is not suitable in all cases. For example, this biomarker cannot be used in hepatic disease because the level of serum HA may be elevated if liver function is interrupted by disease or chemicals [29]. To avoid these effects, we investigated the CBC and blood chemicals in all dogs; however, no abnormal liver signs were observed in either group. These results indicate that the level of serum HA in this study is a direct effect of cartilage metabolism and not a result of liver function.
More than 20 types of sodium hyaluronate are now commercially available worldwide. The sodium hyaluronate used in this study is a highly purified, viscous solution of natural SHA (molecular weight range 500 ~ 730 kDa, concentration 10 mg/mL) extracted from rooster combs. Sodium hyaluronate with the molecular weight used in this study has demonstrated many advantages over that with other molecular weight ranges [5,11]. However, some animal studies of OA conducted using sodium hyaluronate in a molecular weight range of 500~1,000 kDa have been found to be more effective at reducing inflammation and restoring the rheological properties of synovial fluid [11]. Moreover, this molecular weight range has shown the advantage of inducing newly synthesized HA by synoviocytes [31].
Although many reports have demonstrated the advantages of sodium hyaluronate intra-articular injection in human joint disease, few have been performed in dogs. Some previous reports of dogs have shown that sodium hyaluronate intra-articular injection could decrease the progress of OA [8,13]. Echigo et al. [8] found that dogs treated with intra-articular or intra-venous injection of sodium hyaluronate after ACL transection had fewer apoptotic chondrocytes than non-treated dogs. Together with these reports, we have demonstrated the usefulness of sodium hyaluronate in preventing OA development after joint surgery. In conclusion, intra-articular injection of sodium hyaluronate after joint surgery may prevent OA. No significant difference was shown between animals that received one and two injections based on both clinical signs and biomarker levels.
Figures and Tables
Fig. 1
Mean (±SD) score of weight-bearing, lameness, and pain on palpation. Values with different superscripts (a, b) are significantly different (p < 0.05) when compared in the same week.

Acknowledgments
The authors are grateful to the National Research University Project under Thailand's Office of the Higher Education Commission for research funding. The authors also express their gratitude to all staff members at the Bone and Joint Research Laboratory, Faculty of Veterinary Medicine, Chiang Mai University, Thailand, the Metta Pet Hospital, Chiang Mai, Thailand and TRB Chemedica, Thailand for their kind support.
References
1. Altman RD, Moskowitz R. Hyalgan Study Group. Intraarticular sodium hyaluronate (Hyalgan) in the treatment of patients with osteoarthritis of the knee: a randomized clinical trial. J Rheumatol. 1998; 25:2203–2212.
2. Berenbaum F, Grifka J, Cazzaniga S, D'Amato M, Giacovelli G, Chevalier X, Rannou F, Rovati LC, Maheu E. A randomised, double-blind, controlled trial comparing two intra-articular hyaluronic acid preparations differing by their molecular weight in symptomatic knee osteoarthritis. Ann Rheum Dis. 2012; 71:1454–1460.

3. Budsberg SC, Lenz ME, Thonar EJA. Serum and synovial fluid concentrations of keratan sulfate and hyaluronan in dogs with induced stifle joint osteoarthritis following cranial cruciate ligament transection. Am J Vet Res. 2006; 67:429–432.

4. Canapp SO, Cross AR, Brown MP, Lewis DD, Hernandez J, Merritt KA, Tran-Son-Tay R. Examination of synovial fluid and serum following intravenous injections of hyaluronan for the treatment of osteoarthritis in dogs. Vet Comp Orthop Traumatol. 2005; 18:169–174.

5. Coleman PJ, Scott D, Mason RM, Levick JR. Role of hyaluronan chain length in buffering interstitial flow across synovium in rabbits. J Physiol. 2000; 526:425–434.

6. Decaria JE, Montero-Odasso M, Wolfe D, Chesworth BM, Petrella RJ. The effect of intra-articular hyaluronic acid treatment on gait velocity in older knee osteoarthritis patients: A randomized, controlled study. Arch Gerontol Geriatr. 2012; 55:310–315.

7. DeGroot H 3rd, Uzunishvili S, Weir R, Al-omari A, Gomes B. Intra-articular injection of hyaluronic acid is not superior to saline solution injection for ankle arthritis: a randomized, double-blind, placebo-controlled study. J Bone Joint Surg Am. 2012; 94:2–8.

8. Echigo R, Mochizuki M, Nishimura R, Sasaki N. Suppressive effect of hyaluronan on chondrocyte apoptosis in experimentally induced acute osteoarthritis in dogs. J Vet Med Sci. 2006; 68:899–902.

9. Foti C, Cisari C, Carda S, Giordan N, Rocco A, Frizziero A, Della Bella G. A prospective observational study of the clinical efficacy and safety of intra-articular sodium hyaluronate in synovial joints with osteoarthritis. Eur J Phys Rehabil Med. 2011; 47:407–415.
10. Fuller CJ, Barr AR, Sharif M, Dieppe PA. Cross-sectional comparison of synovial fluid biochemical markers in equine osteoarthritis and the correlation of these markers with articular cartilage damage. Osteoarthritis Cartilage. 2001; 9:49–55.

11. Ghosh P, Guidolin D. Potential mechanism of action of intra-articular hyaluronan therapy in osteoarthritis: are the effects molecular weight dependent? Semin Arthritis Rheum. 2002; 32:10–37.

12. Girish KS, Kemparaju K, Nagaraju S, Vishwanath BS. Hyaluronidase inhibitors: a biological and therapeutic perspective. Curr Med Chem. 2009; 16:2261–2288.

13. Hellström LE, Carlsson C, Boucher JF, Michanek P. Intra-articular injections with high molecular weight sodium hyaluronate as a therapy for canine arthritis. Vet Rec. 2003; 153:89–90.

14. Huang TL, Chang CC, Lee CH, Chen SC, Lai CH, Tsai CL. Intra-articular injections of sodium hyaluronate (Hyalgan®) in osteoarthritis of the knee. a randomized, controlled, double-blind, multicenter trial in the Asian population. BMC Musculoskelet Disord. 2011; 12:221.

15. Jazrawi LM, Rosen J. Intra-articular hyaluronic acid: potential treatment of younger patients with knee injury and/or post-traumatic arthritis. Phys Sportsmed. 2011; 39:107–113.

16. Kolarz G, Kotz R, Hochmayer I. Long-term benefits and repeated treatment cycles of intra-articular sodium hyaluronate (Hyalgan) in patients with osteoarthritis of the knee. Semin Arthritis Rheum. 2003; 32:310–319.

17. Kuroki K, Cook JL, Kreeger JM. Mechanisms of action and potential uses of hyaluronan in dogs with osteoarthritis. J Am Vet Med Assoc. 2002; 221:944–950.

18. Marshall KW, Manolopoulos V, Mancer K, Staples J, Damyanovich A. Amelioration of disease severity by intraarticular hylan therapy in bilateral canine osteoarthritis. J Orthop Res. 2000; 18:416–425.

19. Moore AR, Willoughby DA. Hyaluronan as a drug delivery system for diclofenac: a hypothesis for mode of action. Int J Tissue React. 1995; 17:153–156.
20. Moreland LW. Intra-articular hyaluronan (hyaluronic acid) and hylans for the treatment of osteoarthritis: mechanisms of action. Arthritis Res Ther. 2003; 5:54–67.
21. Nganvongpanit K, Pothacharoen P, Chaochird P, Klunklin K, Warrit K, Settakorn J, Pattamapaspong N, Luevitoonvechkij S, Arpornchayanon O, Kongtawelert P, Pruksakorn D. Prospective evaluation of serum biomarker levels and cartilage repair by autologous chondrocyte transplantation and subchondral drilling in a canine model. Arthritis Res Ther. 2009; 11:R78.

22. Ozturk C, Atamaz F, Hepguler S, Argin M, Arkun R. The safety and efficacy of intraarticular hyaluronan with/without corticosteroid in knee osteoarthritis: 1-year, single-blind, randomized study. Rheumatol Int. 2006; 26:314–319.

23. de la Peña E, Sala S, Rovira JC, Schmidt RF, Belmonte C. Elastoviscous substances with analgesic effects on joint pain reduce stretch-activated ion channel activity in vitro. Pain. 2002; 99:501–508.

24. Plickert HD, Bondzio A, Einspanier R, Tichy A, Brunnberg L. Hyaluronic acid concentrations in synovial fluid of dogs with different stages of osteoarthritis. Res Vet Sci. 2013; 94:728–734.

25. Pothacharoen P, Teekachunhatean S, Louthrenoo W, Yingsung W, Ong-Chai S, Hardingham T, Kongtawelert P. Raised chondroitin sulfate epitopes and hyaluronan in serum from rheumatoid arthritis and osteoarthritis patients. Osteoarthritis Cartilage. 2006; 14:299–301.

26. Pozo MA, Balazs EA, Belmonte C. Reduction of sensory responses to passive movements of inflamed knee joints by hylan, a hyaluronan derivative. Exp Brain Res. 1997; 116:3–9.

27. Pruksakorn D, Rojanasthien S, Pothacharoen P, Luevitoonvechkij S, Wongtreratanachai P, Ong-Chai S, Kongtawelert P. Chondroitin sulfate epitope (WF6) and hyaluronic acid as serum markers of cartilage degeneration in patients following anterior cruciate ligament injury. J Sci Med Sport. 2009; 12:445–448.

28. Pullman-Mooar S, Mooar P, Sieck M, Clayburne G, Schumacher HR. Are there distinctive inflammatory flares after hylan g-f 20 intraarticular injections. J Rheumatol. 2002; 29:2611–2614.
29. Sakugawa H, Nakayoshi T, Kobashigawa K, Yamashiro T, Maeshiro T, Miyagi S, Shiroma J, Toyama A, Nakayoshi T, Kinjo F, Saito A. Clinical usefulness of biochemical markers of liver fibrosis in patients with nonalcoholic fatty liver disease. World J Gastroenterol. 2005; 11:255–259.

30. Smith GN Jr, Mickler EA, Myers SL, Brandt KD. Effect of intraarticular hyaluronan injection on synovial fluid hyaluronan in the early stage of canine post-traumatic osteoarthritis. J Rheumatol. 2001; 28:1341–1346.
31. Smith MM, Ghosh P. The synthesis of hyaluronic acid by human synovial fibroblasts is influenced by the nature of the hyaluronate in the extracellular environment. Rheumatol Int. 1987; 7:113–122.

32. Sun SF, Hsu CW, Sun HP, Chou YJ, Li HJ, Wang JL. The effect of three weekly intra-articular injections of hyaluronate on pain, function, and balance in patients with unilateral ankle arthritis. J Bone Joint Surg Am. 2011; 93:1720–1726.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download