Cryptorchidism is a testicular developmental disorder that is quite common in dogs and mainly associated with genetic causes [1]. In retained testes, there is an increased risk of neoplasms, such as Sertoli cell tumors and seminoma, which can exhibit more aggressive behavior than those in scrotal testes [3,9]. Approximately 70% of Sertoli cell tumors arising in abdominal testes are functional and associated with a feminizing paraneoplastic syndrome characterized by non-pruritic, bilateral symmetrical alopecia, hyperpigmentation, gynecomastia, edematous and pendulous penile sheath, prostatic dysfunctions, attraction to other males, and standing in a female posture to urinate [1,4,6,10]. Estrogen myelotoxicosis has been reported in 15% of these dogs and is characterized by bone marrow hypoplasia and non-regenerative anemia [10]. Retained testes are more susceptible than scrotal testes to spermatic cord torsion, and the risk of this condition is increased even more with progressive enlargement of the neoplastic organ [1,7,8]. Although closely linked to one another, concomitant association of cryptorchidism, Sertoli cell tumors, feminizing syndrome, and spermatic cord torsion has been rarely reported in the literature [5,8]. Here, we present two cases of cryptorchidism accompanied by spermatic cord torsion and feminization in dogs.
Case history 1: A 7-year-old male mixed breed dog weighing 27 kg was brought for our examination due to widespread alopecia with hyperkeratosis, progressive weight loss, feminine behavior during urination, and the absence of both testes from the scrotum. Non-pruritic alopecia had originated in the genital and perineal regions, and spread symmetrically into the ventral abdomen, flanks, thorax, and neck (Fig. 1A). Physical examination suggested the development of bilateral abdominal cryptorchidism. The prepuce was pendulous and the prostate was uniformly enlarged. Palpation of the left caudal abdomen identified a large, firm, and painful mass. Ultrasound examination showed a 'complex mass' structure enclosed by a hyperechoic capsule. In the other quadrant, another isoechoic formation of smaller dimensions that resembled testicular parenchyma was also observed. The prostate had increased in volume (4.7 × 4.8 × 7.8 cm), and contained a non-homogeneous parenchyma that included small anechoic areas likely to be cysts. Abdominal radiographs confirmed these findings and, together with the thoracic findings, did not reveal metastases.
Hematological analysis indicated moderate anemia and leukocytosis (hematocrit: 25.7%, hemoglobin: 11.90 g/dL, RBC: 4.37 × 106/µL, WBC: 21.60 × 103/µL). Endocrine evaluation showed alterations in sexual steroid levels with increases in estrogen [progesterone (P4) = 0.39 ng/mL, 17 beta-estradiol (E2) = 17.90 pg/mL, testosterone (T) = 0.66 ng/mL]. Suspecting a Sertoli cell tumor in the retained testis, an exploratory midline laparotomy was carried out to locate and remove both testes.
The left testis, greatly increased in size, presented multiple spermatic cord torsions (Fig. 1B). The right testis, moderately increased in size, was also neoplastic. Grossly, the left testis (10.5 × 6.5 × 5.5 cm) had a significant profile alteration and multilobular appearance; cross-sectionally, it appeared to be completely replaced by spongy neoplastic tissue. The right testis (5 × 4 × 2.5 cm) had a pyramidal shape and was almost completely replaced by lobular compact neoplastic tissue that was yellowish in color. Histopathological sections confirmed the presence of a Sertoli cell tumor with tubular and pseudofollicular patterns in both gonads.
Post-operative treatment was administered including anti-inflammatory drugs for 3 days and antibiotics for 7 days. After 1 month, the clinical symptoms significantly improved. Specifically, the prostate size was greatly reduced, hematological values appeared to recover, and sexual hormones returned to baseline levels (E2 and T were not detected. P4 = 0.14 ng/mL). Total remission of skin symptoms was observed 3 months after surgery.
Case history 2: An 8-year-old male Rottweiler dog weighing 35 kg was admitted for severe hematuria, weight loss, and progressive apathy that had developed during the preceding 5 months. Clinical signs included non-pruritic bilateral symmetrical alopecia in the flanks and thighs. The prepuce was edematous and pendulous, and moderate gynecomastia was also evident. The abdomen was extremely sensitive to palpation and a nodular mass was detected in the caudal quadrant. The left testis had decreased in size and consistency, and was noticeably close to the external inguinal ring. The prostate appeared enlarged and painful upon digital palpation.
Ultrasound examination of the caudal right abdominal quadrant revealed a 'complex mass' structure. The prostate measured 6.9 × 6.8 × 10.5 cm, and had a non-homogeneous echogenicity with cystic formations up to 2.2 cm in diameter. Hematological analysis revealed anemia and leukocytosis (hematocrit: 24.0%, hemoglobin: 8.10 g/dL, RBC: 3.36 × 106/µL, WBC: 33.30 × 103/µL). Endocrine evaluation showed alterations in sexual steroids with increased estrogen levels (P4 = 1.32 ng/mL, E2 = 23.05 pg/mL, T = 0.20 ng/mL). Blood transfusion was necessary to lower anesthetic risk before surgery.
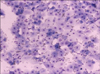
After removing the left testicle, a midline laparotomy identified the right neoplastic testis, associated with double torsion of the spermatic cord, in the abdomen. Following this procedure, the prostatic cyst content was aspirated and the abdomen was closed. Grossly, the right testis (2.5 × 1.5 × 1 cm) was atrophic while the left (4.5 × 3.5 × 2.7 cm) was round in shape and appeared to be completely replaced by neoplastic tissue with a spongy appearance and yellowish-gray in color (Fig. 2). Histological sections confirmed the diagnosis of a Sertoli cell tumor with a pseudotubular pattern characterized by highly vacuolized elements and modest nuclear atypia. Cytological examination of the prostatic cyst content revealed epithelial cells with signs of squamous metaplasia (Fig. 3).
Postoperative treatment included administration of anti-inflammatory drugs for 3 days and antibiotics for 7 days. Four weeks after surgery, the dog gained 4 kg of body weight, hematological parameters improved, and the endocrine profile returned to normal. After 3 months, complete remission of skin symptoms was evident and the prostate volume was markedly reduced (3.9 × 4.1 × 6 cm).
The two cases described above are comparable in terms of consequentiality of the disorders. In both dogs, non-descent of one or both testes favored the development of a functional Sertoli cell tumor similar to cases reported in the literature [1,3]. The associated feminizing syndrome is quite characteristic and often the only external clinical sign of this neoplastic change. Prostatic dysfunctions may be diagnosed during the development of this syndrome. These include benign hyperplasia, squamous metaplasia, and prostatic cysts with related symptoms [2,11]. A sexual hormone assay detected increased levels of estrogen, probably responsible for the blood anomalies. These levels returned to normal a few months after surgical removal of the neoplastic testes.
Retained neoplastic testes are considered to be more predisposed to testicular torsion that can aggravate the clinical signs and result in an inauspicious prognosis [1,7,8]. In the cases reported above, spermatic cord torsion did not provoke congestive or necrotic changes although it certainly contributed to abdominal pain. This study emphasizes the importance of monitoring cryptorchid dogs, especially given the possible complications which may occur over time, in order to correctly evaluate the risks and benefits of surgical gonad removal.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download