The success of influenza viruses lies in their ability to infect and replicate in a host by constantly changing the immunogenic pocket on the surface-exposed hemagglutinin molecule. Another hallmark of this successful pathogen is its ability to establish itself in an intracellular niche, outrace the host innate immune responses, and exit the host using one of the several cell egress pathways before a sustained adaptive immune response is generated.
One cell exit pathway used by viruses is to induce cell death by manipulating host apoptotic pathways [2]. One of the three proteins encoded by internal start sites of the segment 2 (PB1) of the RNA polymerase, PB1-F2, has been shown to localize in the inner mitochondrial membrane and orchestrate programmed cell death or apoptosis [12,13]. Furthermore, it has been demonstrated that the amino acid (aa) at position 66 of PB1-F2 affects the pathogenicity of an H5N1 virus in mice. The N66S mutation contributed to the high pathogenicity of the 1918 pandemic A/Brevig Mission/18 virus, and its replacement (S66N) attenuated this virus in mice [2]. Therefore, PB1-F2 has been identified as a key virulence factor among influenza A viruses.
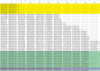
Extensive amino acid sequence analysis of the 2009 (H1N1) influenza A pandemic viruses by our group (n = 397) and others [4,9,10] revealed a major change in PB1-F2 in these strains. A point mutation in nucleotide 129 (C→A change) led to the formation of a STOP codon in place of serine [11], truncating PB1-F2 to an 11 amino acid (aa) peptide instead of the typical, full-length 90 aa protein generally seen in swine viruses (Fig. 1). This change appears to be the one unique genetic event that separates the 2009 pandemic strain from its recent ancestors. Therefore, we seek an explanation of how this change may be involved in the newly found enhanced transmissibility, virulence, and pathogenicity of this pandemic strain of influenza A virus among humans.
Recent studies on PB1-F2 polymorphisms in influenza virus strains associated with major outbreaks in swine since the 1950s have identified three possible truncation mutations after codons 11, 25, and 34, all of which were conserved across other lineages of influenza A viruses suggesting a functional consequence to these mutations [14]. Truncated proteins have been shown to have a more cytoplasmic distribution in the cell in contrast to the mitochondrial inner membrane distribution of full-length proteins, a possible reason for sustained viral replication in cells and increased proinflammatory responses [14]. Our analysis of 12 virus isolates from clinical swine influenza episodes in the US showed that 11 carry a full length PB1-F2 (87-90 aa) and one had a truncated (57 aa) protein, suggesting that minor truncations have not played a role in severe disease seen in pigs in the recent past. On the other hand, if major truncations in PB1-F2 previously ameliorated disease in pigs, they have not been found in this study.
In vivo and in vitro characterizations of the 2009 pandemic (H1N1) influenza virus revealed that it replicates efficiently and causes more severe pathological lesions in mice, ferrets, and non-human primates than a currently circulating seasonal human H1N1 virus [6]. Similar findings on pathogenicity and transmissibility of the 2009 pandemic H1N1 viruses have been described in the ferret model [8]. In contrast, relatively mild clinical signs/disease have been described in pigs inoculated with the 2009 pandemic H1N1 strain [7]. These findings support the hypothesis that the truncated PB1-F2 carried by the current 2009 pandemic H1N1 may be associated with relatively milder infections in pigs in contrast to those identified in experimental animals and humans.
Studies of the 1918 pandemic strain of influenza suggested that a variant of PB1-F2 that carries eight amino acid changes throughout its full-length protein relative to more recent strains suggests that this protein is probably involved in virulence and pathogenicity [2,3]. In another study, one mutation shared by the 1918 strain of flu and Hk/97 was shown to be sufficient for pathogenicity [3]. It is also suggested that strains carrying the truncated PB1-F2 may not be efficient in inducing apoptosis and may produce less inflammation [5]. To date, all of the 2009 pandemic (H1N1) isolates have a PB1-F2 truncation. Therefore, we hypothesize that this truncated PB1-F2 may play an important role in the pathogenicity and tranmissibility of 2009 pandemic H1N1.
Other questions related to the biology of these viruses also arise - Does this S12Atop polymorphism in PB1-F2 lead to a variation in host specificity or host adaptation resulting in less severe disease in swine host versus a sustained infection in humans? Does the localization of PB1-F2 in the cytoplasm versus mitochondria lead to greater efficiency in viral replication? A synthetic peptide of PB1-F2 has been shown to be a potent pro-apoptotic factor, and a C-terminal peptide has been shown to be proinflammatory [1].
Next, does a truncation mutation that rescues only 11 amino acids of the N-terminal part of 2009 H1N1 strain explain, in part, the enhanced virulence or replication efficiency of this virus in human hosts? Or does this peptide even get stably translated in the cells? Experimental studies with pigs have shown low pathogenicity that may be related to the truncation of PB1-F2. We, therefore, propose that a better understanding of the pathogenesis will come from studies on PB1-F2 peptide, and whole virus (with the truncated PB1-F2 or complemented full-length PB1-F2) inoculation studies in animal models. Such studies should also address the replication and transmission efficiencies in and among a variety of hosts. Retrospective analyses of influenza A viruses isolated from clinically and pathologically well-characterized swine populations would be necessary to understand the natural history and emergence of this new pandemic strain.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download