Abstract
Objective
Women presenting with a large or complex ovarian cyst are referred to extensive surgical staging to ensure the correct diagnosis and treatment of a possible epithelial ovarian cancer. We hypothesized that measurement of the biomarkers HE4 and CA-125 preoperatively would improve the assignment of these patients to the correct level of care.
Methods
Patients diagnosed with a cystic ovarian mass and scheduled for an operation at our center of excellence for ovarian cancer surgery from 2001 to 2010 were prospectively included (n=394) and plasma was collected consecutively. Cut-off for HE4 was calculated at 75% specificity (85 pM and 71.8 pM for post and premenopausal women). For CA-125, 35 U/mL cut-off was used. The study population included women with malignant (n=114), borderline (n=45), and benign (n=215) ovarian tumors.
Results
Receiver operator characteristic (ROC) area under the curve (AUC) in the benign versus malignant cohorts was 86.8% for CA-125 and 84.4% for HE4. Negative predictive value was 91.7% when at least one of the biomarkers was positive, with only early stage epithelial ovarian cancer showing false negative results. Sensitivity at set specificity (75%) was 87% for risk of ovarian malignancy algorithm (ROMA) in the postmenopausal cohort (cut-off point, 26.0%) and 81% in the premenopausal cohort (cut-off point, 17.3%). ROC AUC in the benign versus stage I epithelial ovarian cancer was only 72% for HE4 and 76% for CA-125.
Ovarian tumors grow in combined cystic and solid formations. There is no reliable diagnostic test or imaging technique available to distinguish benign from malignant cysts [1]. The decision to operate is based on clinical findings, transvaginal sonography, computed tomography and/or magnetic resonance imaging, and cancer antigen 125 (CA-125) levels. Approximately 7 to 10 benign lesions are operated on for each case of ovarian cancer found [2]. Consequently, several patients undergo extensive surgical staging, including oophorectomy, without an assured diagnosis of a malignant tumor, resulting in increased morbidity. Thus, there would be both medical and socio-economic benefits if we could preoperatively identify patients with benign cysts and safely be able to recommend conservative laparoscopic staging operations [3].
The tumor marker CA-125 is used to predict the presence of malignancy in patients with a pelvic mass [4]. CA-125 is elevated (>35 U/mL) in 80% of cases of advanced cancer, but in fewer than 50% of cases in early stages. Moreover, CA-125 is often elevated in different benign gynecologic and non-gynecologic conditions and in premenopausal women [5]. Human epididymis protein 4 (HE4) is a prominent new candidate for the detection of ovarian cancer [6,7]. The marker was discovered in RNA expression arrays comparing normal epithelial cells and malignant tumors [8,9]. Hellstrom and colleagues [10] constructed HE4 antibodies and reported that in a rather small study population HE4 and CA-125 in serum samples detected ovarian cancer equally, but HE4 had a better capacity to distinguish healthy women and women with benign disease from those with malignant tumors. The findings indicated that HE4 used in combination with CA-125 might be a promising tool for the detection of ovarian cancer. Moore and colleagues [11] have created an algorithm for risk scoring called the risk of ovarian malignancy algorithm (ROMA) based on menopausal status and preoperative measurement of the dual markers. ROMA classifies women with ovarian cyst or pelvic mass scheduled to undergo surgery into low- and high-risk groups. Today, the question still remains whether HE4, ROMA, or both add sufficient information to CA-125 to be implemented in clinical practice [12,13].
It is evident that an early diagnosis is the most important factor for substantial improvement in the survival rate of patients with ovarian cancer, as shown by 5-year survival rates of over 80% for women in early stages to under 30% for those in stages III-IV [14]. The first published studies indicated that HE4 has higher sensitivity in identifying early stage disease than does CA-125 [7,15]. Conversely, later studies have shown CA-125 to be the best marker for detecting early stage disease [6,16].
We first hypothesized that known ovarian cysts in a study population might be better classified with HE4 alone or in combination with CA-125 than with CA-125 alone. Second, we intended to estimate an optimal cut-off value for HE4 in our study population [11,17]. Third, we intended to independently validate ROMA. We prospectively collected blood and tumor tissue from patients presenting with a suspicious ovarian cystic pelvic mass from 2001 to 2010. The patients had already been assigned to operation at our center of excellence for ovarian cancer surgery.
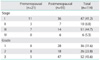
The study population (n=374) comprised of women with benign ovarian tumors (n=215), borderline type tumors (n=45), and epithelial ovarian cancer (EOC; n=114) (Table 1). Menopause status, defined as one year of amenorrhea, was checked for women between 47 and 56 years of age. Patients <47 years old were considered premenopausal, and women >56 years were considered postmenopausal. The local ethics committee at Gothenburg University approved the study protocol and samples were collected consecutively from all patients presenting with a suspected malignant ovarian cystic mass who signed a written informed consent. After surgery, tumors were examined by an experienced pathologist for diagnosis, histology, and grade and staged (I-IV) according to International Federation of Gynaecology and Obstetrics (FIGO) standards (Table 2).
Patients were prospectively included when admitted to operation for a clinically suspicious ovarian cystic mass at the section for gynecologic oncology surgery, Sahlgrenska University Hospital, Gothenburg, Sweden from 2001 to 2010. Patients were selected for operation at this specialized unit when diagnosed with a suspected malignant ovarian cystic mass. Generally, the criteria used for this selection were pre- or postmenopausal status, prior family or personal history of ovarian or breast cancer, and size, complexity at transvaginal ultrasound (double or multiple cysts, thick walls, excrescences), and fixed or bilateral nature of the tumors. Patients with a solid pelvic tumor were not invited to participate. Patients who did not want to be included were excluded. The patient was excluded if final histology showed the origin of the tumor was not ovarian.
Blood samples were collected after anesthesia but before surgery. Six milliliters of blood were collected in citrated vacutainers using standardized procedures and stored at 4℃ within 15-30 minutes. Plasma was collected after centrifugation, directly aliquoted into Eppendorf tubes, frozen, and stored at -80℃ within 30-60 minutes after withdrawal. Handling and processing were standardized for all patients included in the investigation. All analyses were performed on plasma.
The analyses were performed on plasma from patients diagnosed with a suspicious ovarian cystic mass, while serum is the ordinary analytic fluid to be used according to the manufacturer's instructions (Fujirebio Diagnostics, Goteborg, Sweden). Fujirebio Diagnostics performed a correlation study of plasma and serum HE4 levels prior to our analysis. Plasma and serum were drawn simultaneously from 44 women. Levels of HE4 matched with an acceptable correlation (R2=0.90).
HE4 plasma concentrations were determined using the HE4 EIA assay (Fujirebio Diagnostics) and plasma CA-125 levels were measured using Architect CA-125 II (Abbott Diagnostics, Abbott Park, IL, USA) at Fujirebio Diagnostics. The analytical runs of the biomarkers fulfilled the laboratory QC criteria for each analysis based on QC-samples within acceptance limits as well as dose response and reproducibility within predetermined limits. The laboratory technician performing the assays was blinded to both clinical diagnoses and individual pathology results and the pathologist was blinded to laboratory values.
Currently, there is no recommended cut-off value for HE4. According to the protocol from the manufacturer, 23 of 347 women (6.6%) with benign gynecological disease have HE4 >150 pM. Among apparently healthy females a cut-off value of 70 pM has been suggested [11], however, the value may vary depending upon the study population. Our analysis includes only patients already diagnosed with a suspicious cystic ovarian mass, so the cut-off value for this group had to be determined for HE4 and ROMA. In line with Moore et al. [11], who presented a comparable study population, specificity was fixed at 75% and the cut-off value in our material for that outcome was calculated for HE4 and ROMA. ROMA was estimated as previously described. If the sensitivity then exceeded 80%, at least 80% of the patients with malignant cystic pelvic masses would be operated on at the specialist unit for gynecologic oncology surgery. The threshold for positive diagnosis by CA-125 was set at 35 U/mL, which is routinely used in our clinic. Specificity and sensitivity for CA-125 were calculated using >35 U/mL as the cut-off point.
Statistical differences in protein levels between groups were evaluated using the Mann-Whitney U-test. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated for each marker and for ROMA. The protein levels were subjected to logistic regression analysis, the predictive probabilities for each model were used to construct receiver operating characteristic (ROC) curves, and area under the curve (AUC) values were calculated. For all statistical comparisons a value of p<0.05 was considered significant. Statistical analyses were performed in SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA).
We enrolled 394 patients with a suspicious cystic ovarian mass and excluded 20 because of non-ovarian histology. Of the 374 patients eligible for analysis, 57.5% had benign tumors, 12.0% had borderline tumors, and 30.5% had EOC (Table 1). Mean age in relation to menopausal status was equally distributed within the three cohorts, while overall mean age for the borderline cohort was 10 years younger. Serous histology was the most common diagnosis among the three cohorts. Mucinous histology was relatively higher in the benign and borderline cohorts than in the group with malignant tumors. In patients with EOC, 57 (50%) were diagnosed with early stage (I-II) and 57 (50%) with late stage (III-IV) disease (Table 2).
Analysis of tumor-marker levels was performed blinded and the cohort samples were mixed. A visual description of HE4 and CA-125 correlation within the 3 cohorts is presented in Fig. 1. Median HE4 plasma level for all benign-tumor patients was 66 pM (Table 3). Levels of HE4 significantly (p<0.001) distinguished the benign-tumor cohort from those with stage I EOC and those with any EOC, but not from those with borderline type tumors (Table 3). Significance was also reached, except for borderline type tumors in the premenopausal group, for distinguishing the cohorts into pre- and postmenopausal groups. Both biomarkers and ROMA demonstrated significance with low stringency (p<0.05) for benign versus stage I tumors in the premenopausal group. The median plasma level for CA-125 for all patients with benign tumors was 16 U/mL (range, 2 to 4,632 U/mL) (Table 3). Levels of CA-125 were significantly (p<0.001) different between the cohort with benign tumors and those with borderline tumors, stage I EOC, and all EOC (Table 3). Significance was also reached in distinguishing the cohorts into pre- and postmenopausal groups. The dual marker algorithm, ROMA, implemented by Moore et al. [11] was subsequently calculated for the study population, again clearly separating (p<0.001) the benign-tumor from the malignant-tumor cohort and the benign from early stage I EOC (p<0.05) for both pre- and postmenopausal women (Table 3).
The diagnostic accuracy of CA-125 and HE4 alone, in combination, and for ROMA was assessed by estimating ROC and AUC for patients with benign versus malignant tumors (Fig. 2). The highest ROC AUC was calculated for ROMA and CA-125 (87%), followed by the combination of CA-125 and HE4 (85%), and HE4 alone (84%) (Fig. 2, Table 4). Specificity was set to 75% for HE4, which we considered relevant for our selected material of suspicious cystic ovarian mass. At this level, to distinguish between the benign-tumor and the malignant-tumor cohorts, the estimated cut-off for HE4 was 85 pM. When using this cut-off sensitivity for HE4, CA-125 (specificity 80% at cutoff 35 U/mL) was 78% and 82% respectively. The best sensitivity (89%) and negative predictive value (92%) were achieved when at least one of the two biomarkers was positive at the set cut-off points (specificity 66%). In addition, we estimated the most common cut-off for HE4 used in previous investigations at 70 pM [11]. At this cut-off the sensitivity was 88% and the specificity 57% in our material. On examining the group of patients with malignant tumors who had negative results for one or both of the biomarkers (false negatives), we found that most were in FIGO stage I (CA-125, 18 of 21 false negatives; HE4, 19 of 25 false negatives; HE4+CA-125, 12 of 13 false negatives). In the last group (HE4+CA-125) 100% of the false negatives were in stage I (n=12) or stage II (n=1). False positives in the benign cohort were evenly distributed between the major histological subgroups for each biomarker, except for CA-125 in endometrioma, which had a much higher rate of false positives (45%).
The study population was subsequently divided into a preand a postmenopausal group. The ROC AUC values for the premenopausal cohort were similar for HE4 (82%), CA-125 (85%), and ROMA (83%) (Table 4). The cut-off value for HE4 was separately calculated in the premenopausal group as 71.8 pM and for ROMA as 17.3% at 75% specificity. The sensitivity among premenopausal women was higher for ROMA and HE4 (both 81%) than for CA-125 (76%). The cut-off point for ROMA in the postmenopausal group at 75% specificity was estimated as 26.0%. The sensitivity among postmenopausal women was very good for ROMA (87.1%) and diagnostic accuracy described by ROC AUC values were 85% for HE4, 87% for CA-125, and 89% for ROMA. Both biomarkers and ROMA diagnosed malignant disease more correctly in postmenopausal women than in premenopausal women.
The performance of CA-125 was the best of the markers in distinguishing between women with stage I EOC versus benign tumors, with an ROC AUC of 76% compared with 72% for HE4 (Table 4). Both sensitivity and specificity was higher for CA-125 in stage I EOC at the set cut-off points. Due to small sample size, stage I EOC was not divided into a pre- and postmenopausal group in the analysis, which could have affected the individual biomarkers performance. Calculation of ROC AUC and sensitivity in the groups with benign versus borderline type tumors did not add any useful clinical information (Table 4). Median levels of mucinous EOC were low in both the borderline and the stage I tumor groups, leading to several false negatives. In fact, the overall majority of false negatives were found in these two subgroups, strongly affecting the ROC AUC outcome.
We used consecutively collected blood samples from 374 patients scheduled for surgery for a suspicious cystic ovarian or pelvic mass and analyzed the levels of HE4 and CA-125. We found that HE4 did not perform better than CA-125 results in the total material, but may be more useful in premenopausal women. Negative predictive value was high (92%) if CA-125, HE4, or both were elevated, and all false negatives were found in early stage EOC. This finding suggests that HE4 adds information in the preoperative workup.
Women presenting with a suspicious ovarian cyst or cystic pelvic mass are presently commonly exposed to open laparotomy and an extensive staging operation. A patient with this diagnosis should always be operated on at a unit where the gynecologic surgeons are trained in optimal debulking surgery [18]. On the other hand, approximately 7 to 10 benign cysts are removed for each single discovery of ovarian cancer [2]. The lack of preoperative screening modalities to predict diagnostic outcome increases unnecessary extensive abdominal ovarian staging operations. The risk of malignity index (RMI), an algorithm based on CA-125, menopausal status, and transvaginal sonography, was the first to be used for referral of ovarian cancer patients [19]. Another algorithm, ROMA, based on HE4, CA-125, and menopausal status, was shown to stratify patients into high- and low-risk groups, enabling more accurate triage of patients to centers of excellence for ovarian cancer than RMI [20], while McDonald et al. [21] concluded that patients with solid or complex ovarian tumors and elevated CA-125 were those at high risk of ovarian malignancy. The results from our investigation suggest that adding measurements of HE4 to CA-125 in the preoperative evaluation of a suspicious ovarian cyst or cystic pelvic mass may help to choose the correct type and setting for the operation. If we had evaluated HE4 and CA-125 in addition to TVS and CT preoperatively, the majority of the patients in our study population could have had conservative laparoscopic staging, without the risk of an incorrect diagnosis [3] since every one of the 13 false negatives were in the early stage. With the incorporation of this measure preoperatively, not only will the patient have fewer preoperative complications and less co-morbidity due to unnecessary abdominal procedures, but she will also have a shorter stay at the hospital, be back to her ordinary life more quickly, and be left with one intact ovary.
Several groups have investigated HE4 in a possible screening setting and report good ROC AUC separating women with either early or late stage epithelial ovarian cancer from healthy controls [10,16,22,23]. HE4 is a biomarker that increases progressively with disease and is markedly lower in healthy women than in women with benign ovarian cysts [12]. This fact makes comparisons between the above-mentioned studies, which include patients without disease of the ovaries, and studies like ours and others [6,24], which compare prospective data from known ovarian masses less relevant. Very promising results that separate benign from malignant disease using HE4 alone have presented ROC AUC of 95% [25] and 91% [7], while we and others reached an ROC AUC of 84%, 84% [6], and 86% [24]. Different cut-off points, more postmenopausal women in the benign cystic cohort, and the fact that we analyzed plasma instead of serum could have influenced our results. As in several other studies, CA-125 performed better than HE4 in our estimation, not only in the whole group but also when we divided the cohorts into benign versus borderline and stage I EOC.
The sample characteristics in our investigation differ from the normal distribution one could expect because the patients were already qualified for operation at our centre of excellence for ovarian cancer surgery. Compared to a population-based incidence of operated ovarian cysts our cohort included fewer benign samples (58%), more early stage EOC (50%), and more postmenopausal women (74%). The young, fertile women with simple cysts considered to have a low risk of malignancy were operated on at the benign gynecology unit and were never part of the investigation. It is important to be aware that the composition of study populations varies greatly between published studies and very few present data from a normal clinical setting without exclusions. Relatively high or low numbers of women with endometrioma or mucinous tumors also affect the overall results for both biomarkers in analyses [26,27]. A large older population in the benign cohort, as in ours, will affect analyses because HE4 increases every two years in healthy postmenopausal women [28] and CA-125 decreases after menopause [26,29]. Both Moore et al. [11] and Van Gorp et al. [24] had more premenopausal women (57% and 47% compared to our 26%) in the benign group than we did. Another difference is the large proportion of early stage EOC in our study. Aggressive EOC with large numbers of small peritoneal metastases and ascites (stage IIIIV) seldom present themselves with cystic formations. These stage III-IV tumors were excluded according to the study criteria and could account for a lower proportion of late stage tumors than expected.
In healthy premenopausal women CA-125 is more often elevated than HE4 in different benign gynecologic conditions [5,11,23]. This is also true for our data, suggesting that HE4 is a good complement to distinguish CA-125 false positives from true positives, especially in fertile women. A previous investigation of serum from healthy women and women with ovarian cancer showed that CA-125 is a better marker than HE4 for women age 50 and over, and that HE4 had better specificity among women under the age of 50 [23]. Further, an investigation comparing benign and malignant tumors showed that HE4 had greater sensitivity than CA-125 among premenopausal women, and that CA-125 and HE4 perform at the same level among postmenopausal women [7]. We can confirm that HE4 yields higher sensitivity and is a more stable marker in premenopausal women at a set specificity than CA-125. For postmenopausal women CA-125 (with a cut-off of 35 U/mL) yielded higher specificity than for premenopausal women (83% vs. 75%).
The cut-off value for HE4 at 75% specificity in our analysis was 85 pM but mean HE4 levels were lower in the premenopausal women. Estimated cut-off in this group was 71.8 pM, which accords with the cut-off of 70 pM used in other studies [11,24,27]. Most algorithms for the referral of patients are based on an evaluation of TVS alone or in combination with biomarkers and menopause status [1,19,21]. Indeed TVS was performed on all patients in our cohort, but not in a standardized way. Instead, we calculated ROMA in our cohort. Diagnostic accuracy of ROMA described by ROC AUC was estimated at 88.7% (postmenopaus) and 83.1% (premenopaus), which is well in line with other published data. If both markers are measured in the future, the clinician may look at the independent values for the two markers (highest negative predictive value but lower specificity) or be calculating ROMA. HE4 and CA-125 in each patient might also need to be evaluated according to other factors such as chronic or intermittent disease, BMI, and smoking [28]. In our benign group, the three highest values of HE4 belonged to two patients with chronic kidney failure, a disease known to have increased HE4 values, and one patient with breast cancer, suggesting that patient history should be accounted for more strictly when the results of new biomarkers are being evaluated.
CA-125 is known to have low sensitivity and specificity in women with early stage cancer. Previous findings of the performance of HE4 and CA-125 in early stage tumors are contradictory, favoring both CA-125 and HE4 as the best marker to detect early disease [6,7,10]. We found that the ROC AUC and sensitivity were slightly higher for CA-125 than for HE4. The number of early stage tumors in the studies range from 7 to 132 (with 47 in our study), and the menopausal status of the women differ between analyses. In our study CA-125 is again favored by the large cohort of postmenopausal women with very low levels. Dividing fertile and postmenopausal women with early stage cancer into two groups before the analysis could perhaps have changed the data, especially for the premenopausal group, but this was not done because of the small sample size.
Currently many women are diagnosed with an ovarian cyst during a visit to a gynecologist or during investigation of unknown abdominal pain by computer tomography. Women presenting with an ovarian cystic pelvic mass may be classified more correctly by measuring both CA-125 and HE4. We suggest, based on this study, that these biomarkers could be included in a prospective study of patients diagnosed with an ovarian cyst scheduled for surgery. According to their HE4 and CA-125 levels, patients would be assigned to either a conservative laparoscopic ovarian cancer staging operation or an explorative laparotomy with debulking.
Figures and Tables
 | Fig. 1Correlation between HE4 and CA-125. Logarithmic scales are used, and the dotted lines show cut-off values. HE4, 85 pM; CA-125, 35 U/mL. |
 | Fig. 2Receiver operating characteristic curves of benign vs. malignant cases. ROMA, risk of ovarian malignancy algorithm. |
Table 3
Tumor marker levels and risk of ovarian malignancy algorithm (ROMA) among patients with benign, borderline type, and malignant samples

ACKNOWLEDGMENTS
This work was supported by the Swedish Cancer Foundation (KS) and the foundations of Assar Gabrielsson (KP and BK), Gothenburg Medical Society (BK), and Hjalmar Svensson (KP and BK).
References
1. Granberg S, Wikland M, Jansson I. Macroscopic characterization of ovarian tumors and the relation to the histological diagnosis: criteria to be used for ultrasound evaluation. Gynecol Oncol. 1989. 35:139–144.
2. van Nagell JR Jr, DePriest PD, Ueland FR, DeSimone CP, Cooper AL, McDonald JM, et al. Ovarian cancer screening with annual transvaginal sonography: findings of 25,000 women screened. Cancer. 2007. 109:1887–1896.
3. Suh-Burgmann E. Long-term outcomes following conservative surgery for borderline tumor of the ovary: a large population-based study. Gynecol Oncol. 2006. 103:841–847.
4. Bast RC Jr, Badgwell D, Lu Z, Marquez R, Rosen D, Liu J, et al. New tumor markers: CA125 and beyond. Int J Gynecol Cancer. 2005. 15:Suppl 3. 274–281.
5. Woolas RP, Xu FJ, Jacobs IJ, Yu YH, Daly L, Berchuck A, et al. Elevation of multiple serum markers in patients with stage I ovarian cancer. J Natl Cancer Inst. 1993. 85:1748–1751.
6. Nolen B, Velikokhatnaya L, Marrangoni A, De Geest K, Lomakin A, Bast RC Jr, et al. Serum biomarker panels for the discrimination of benign from malignant cases in patients with an adnexal mass. Gynecol Oncol. 2010. 117:440–445.
7. Moore RG, Brown AK, Miller MC, Skates S, Allard WJ, Verch T, et al. The use of multiple novel tumor biomarkers for the detection of ovarian carcinoma in patients with a pelvic mass. Gynecol Oncol. 2008. 108:402–408.
8. Hough CD, Sherman-Baust CA, Pizer ES, Montz FJ, Im DD, Rosenshein NB, et al. Large-scale serial analysis of gene expression reveals genes differentially expressed in ovarian cancer. Cancer Res. 2000. 60:6281–6287.
9. Schummer M, Ng WV, Bumgarner RE, Nelson PS, Schummer B, Bednarski DW, et al. Comparative hybridization of an array of 21,500 ovarian cDNAs for the discovery of genes overexpressed in ovarian carcinomas. Gene. 1999. 238:375–385.
10. Hellstrom I, Raycraft J, Hayden-Ledbetter M, Ledbetter JA, Schummer M, McIntosh M, et al. The HE4 (WFDC2) protein is a biomarker for ovarian carcinoma. Cancer Res. 2003. 63:3695–3700.
11. Moore RG, McMeekin DS, Brown AK, DiSilvestro P, Miller MC, Allard WJ, et al. A novel multiple marker bioassay utilizing HE4 and CA125 for the prediction of ovarian cancer in patients with a pelvic mass. Gynecol Oncol. 2009. 112:40–46.
12. Montagnana M, Lippi G, Ruzzenente O, Bresciani V, Danese E, Scevarolli S, et al. The utility of serum human epididymis protein 4 (HE4) in patients with a pelvic mass. J Clin Lab Anal. 2009. 23:331–335.
13. Li J, Dowdy S, Tipton T, Podratz K, Lu WG, Xie X, et al. HE4 as a biomarker for ovarian and endometrial cancer management. Expert Rev Mol Diagn. 2009. 9:555–566.
14. Heintz AP, Odicino F, Maisonneuve P, Quinn MA, Benedet JL, Creasman WT, et al. Carcinoma of the ovary: FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet. 2006. 95:Suppl 1. S161–S192.
15. Shah CA, Lowe KA, Paley P, Wallace E, Anderson GL, McIntosh MW, et al. Influence of ovarian cancer risk status on the diagnostic performance of the serum biomarkers mesothelin, HE4, and CA125. Cancer Epidemiol Biomarkers Prev. 2009. 18:1365–1372.
16. Havrilesky LJ, Whitehead CM, Rubatt JM, Cheek RL, Groelke J, He Q, et al. Evaluation of biomarker panels for early stage ovarian cancer detection and monitoring for disease recurrence. Gynecol Oncol. 2008. 110:374–382.
17. Fujirebio Diagnostics I. HE4 EIA package insert [Internet]. cited 2011 May 8. Goteborg: Fujirebio Diagnostics;Available from:
http://www.fdi.com/documents/products/inserts/eia/HE4%20EIA%20404-10,%202008-09,%20r1.pdf.
18. du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d'Investigateurs Nationaux Pour les Etudes des Cancers de l'Ovaire (GINECO). Cancer. 2009. 115:1234–1244.
19. Jacobs I, Oram D, Fairbanks J, Turner J, Frost C, Grudzinskas JG. A risk of malignancy index incorporating CA 125, ultrasound and menopausal status for the accurate preoperative diagnosis of ovarian cancer. Br J Obstet Gynaecol. 1990. 97:922–929.
20. Moore RG, Jabre-Raughley M, Brown AK, Robison KM, Miller MC, Allard WJ, et al. Comparison of a novel multiple marker assay vs the Risk of Malignancy Index for the prediction of epithelial ovarian cancer in patients with a pelvic mass. Am J Obstet Gynecol. 2010. 203:228.e1–228.e6.
21. McDonald JM, Doran S, DeSimone CP, Ueland FR, DePriest PD, Ware RA, et al. Predicting risk of malignancy in adnexal masses. Obstet Gynecol. 2010. 115:687–694.
22. Scholler N, Crawford M, Sato A, Drescher CW, O'Briant KC, Kiviat N, et al. Bead-based ELISA for validation of ovarian cancer early detection markers. Clin Cancer Res. 2006. 12(7 Pt 1):2117–2124.
23. Andersen MR, Goff BA, Lowe KA, Scholler N, Bergan L, Drescher CW, et al. Use of a Symptom Index, CA125, and HE4 to predict ovarian cancer. Gynecol Oncol. 2010. 116:378–383.
24. Van Gorp T, Cadron I, Despierre E, Daemen A, Leunen K, Amant F, et al. HE4 and CA125 as a diagnostic test in ovarian cancer: prospective validation of the Risk of Ovarian Malignancy Algorithm. Br J Cancer. 2011. 104:863–870.
25. Abdel-Azeez HA, Labib HA, Sharaf SM, Refai AN. HE4 and mesothelin: novel biomarkers of ovarian carcinoma in patients with pelvic masses. Asian Pac J Cancer Prev. 2010. 11:111–116.
26. Palmer C, Duan X, Hawley S, Scholler N, Thorpe JD, Sahota RA, et al. Systematic evaluation of candidate blood markers for detecting ovarian cancer. PLoS One. 2008. 3:e2633.
27. Huhtinen K, Suvitie P, Hiissa J, Junnila J, Huvila J, Kujari H, et al. Serum HE4 concentration differentiates malignant ovarian tumours from ovarian endometriotic cysts. Br J Cancer. 2009. 100:1315–1319.
28. Lowe KA, Shah C, Wallace E, Anderson G, Paley P, McIntosh M, et al. Effects of personal characteristics on serum CA125, mesothelin, and HE4 levels in healthy postmenopausal women at high-risk for ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2008. 17:2480–2487.
29. Menon U, Jacobs IJ. Ovarian cancer screening in the general population. Curr Opin Obstet Gynecol. 2001. 13:61–64.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download